Fig. 5.1
Revised classification of endometriosis by American Society for Reproductive Medicine. The localization and size of the endometriotic lesions are the main markers used to provide classification of the disease (According to the American Society for Reproductive Medicine, classification can only be determined after surgery)
). Therefore, the classification of disease can only be determined after surgical pelvic evaluation [6].
Owing to the difficulties found in the use of the existing methods of classification, the American Association of Gynecological Laparoscopists (AAGL) is formulating a new classification for the disease based on pain, infertility, and surgical difficulty, which are criteria that are not considered by the ASRM classification [7]. The main symptoms of endometriosis are dysmenorrhea, chronic pelvic pain, dyspareunia, cyclical intestinal alterations, cyclical urinary alterations, and infertility, with the latter occurring in 40 % of women with endometriosis [2, 8]. Pain is usually assessed by a visual scale analysis. The clinical examination, including the gynecologic examination, can be normal or unspecific. Some of the alterations that can be found are visible lesions on external genital organs, pain during the mobilization of the cervix, nodules, and thickenings on palpable ligaments.
Table 5.1
Main symptoms of endometriosis
Symptom | Peritoneal | Ovarian | Deep | P |
|---|---|---|---|---|
Severe dysmenorrhea | 22 (51.8 %) | 126 (48.5 %) | 229 (62.9 %) | 0.005 |
Chronic pain | 96 (50.3 %) | 143 (54.8 %) | 233 (63.5 %) | 0.006 |
Infertility | 56 (28.7 %) | 66 (25.2 %) | 124 (34.1 %) | 0.03 |
Cyclic dyschezia | 21 (11.4 %) | 33 (13 %) | 120 (33.5 %) | <0.001 |
Cyclic dysuria | 27 (14.1 %) | 34 (13 %) | 56 (15.3 %) | 0.71 |
Dyspareunia | 97 (51.6 %) | 138 (52.9 %) | 227 (63.4 %) | 0.007 |
Many scientists have attempted explanations Physiopathology for the development of endometriosis, such as endometrial tissue and cell reflux during menstruation as described by Sampson [9], the differentiation of other cells from endometrial cells (metaplasia), and the hematogenous and lymphatic spread of endometrial cells [9, 10]. However, the disease has been evidenced in patients with the absence of a uterus or in men who have taken high doses of estrogen for prostatic cancer, showing that no theory fully explains the physiopathology of endometriosis [9, 10].
What is known is that genetics plays an important role in its development. Patients who have first-degree relatives who have or have had the disease have a six times higher possibility of developing endometriosis than those without such a relative. The prevalence is 4–9 % in first-degree relatives [11]. Diagnosis histology is still the gold standard to diagnose endometriosis. Biopsy is done by laparoscopy. However, surgical diagnosis is considered an invasive procedure, and efforts are being made to develop less invasive techniques with high sensibility and specificity, such as transvaginal ultrasonography and the CA 125 test.
The CA 125 blood levels measurement is a laboratory test commonly used as an ovarian cancer marker of epithelial origin and also to evaluate patient response to chemotherapy. But it can also be used as a predictor of endometriosis [12]. However, many studies demonstrate that it is not as good a predictor for early stages such as I and II (mild and moderate endometriosis) as it is for severe endometriosis [13].
It has been established that the best examination to evaluate endometriosis is transvaginal ultrasonography (TV-USG) with bowel preparation. It can detect lesions that are larger than 2 cm. For deep infiltrating endometriosis (DIE), studies have demonstrated that the TV-USG has 98 % sensibility and 100 % specificity, which are better than the results of magnetic resonance imaging (MRI) [14]. Therefore, it is important and feasible to diagnose the disease early in life in order to prevent long-term complications.
Likewise, ovarian endometriosis has been well documented with TV-USG as well as with MRI. Both show the same results, but the former is less expensive. On the other hand, lesions involving ureters are better evaluated by MRI than by TV-USG for a more accurate identification of the site of the lesion.
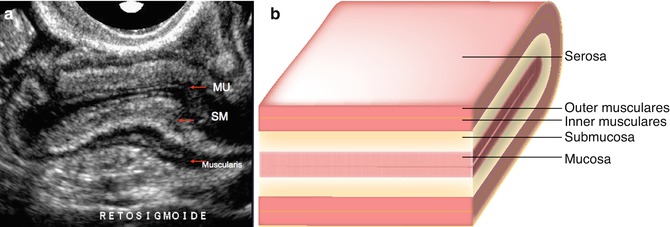
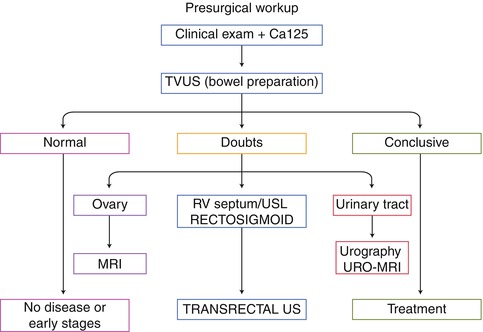
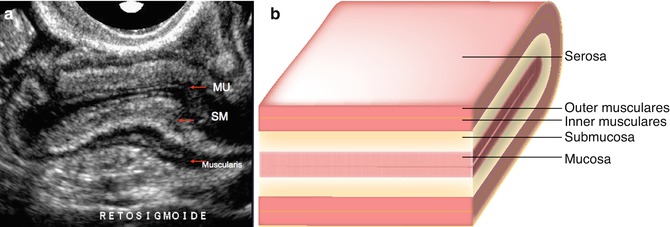
Fig. 5.2
Transvaginal ultrasound showing intestinal layers. (a) A rectosigmoid section showed by ultrasound with all layers delimited. (b) With careful analysis of each layer, endometriotic lesions can be diagnosed by ultrasound. MU musculares, SM submucosas
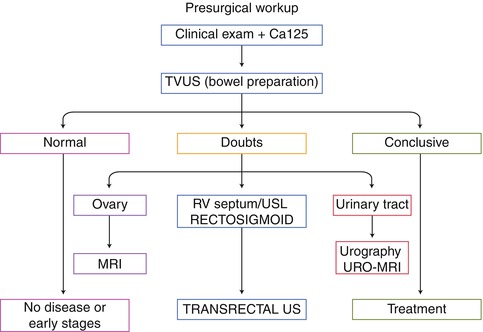
Fig. 5.3
Flow chart for diagnosis of endometriosis. The investigation starts with the clinical history and the physical examination; although the measure of CA 125 levels can be used as well, it has low sensibility and specificity. The next step is to perform a transvaginal ultrasound (TV-US) with bowel preparation by professionals specializing in finding lesions of endometriosis in ultrasound images. If these steps are conclusive for endometriosis, then treatment should be planned. With a normal image examination, there is probably no disease or it is in very early stages. If the initial investigation is inconclusive, other imaging examinations can be indicated according to the probable location of the lesions. MRI magnetic resonance imaging, URO-MRI urologic magnetic resonance imaging
5.3 Treatment
Treatment for endometriosis should be individualized for each patient. Management of the disease should only be initiated after careful analysis of symptoms and image examinations, after thorough discussion with the patient regarding the consequences of each procedure and reason for treatment (pain, pregnancy). Furthermore, endometriosis is frequently a multisystem disease, and this is the reason why treatment requires a multidisciplinary team to provide the best care for patients [15]. This often includes other areas of medicine, such as proctology and urology, as well as other health care areas, such as psychology and physiotherapy.
Treatment of endometriosis consists mainly of three procedures: pharmacologic ovarian suppression, painkillers, and video-assisted laparoscopic surgery. The pharmacologic treatment involves any agent that blocks ovarian hormone production and theoretically reduces pain, as endometriotic lesions are responsive to hormone levels [16].
5.4 Laparoscopic Surgery
The benefits of laparoscopic surgery versus laparotomy for endometriosis have been established in the literature [17]. Laparoscopic surgery provides better visualization of the pelvic cavity, less formation of adhesions, faster discharge of the patient, lower costs, and less postoperative pain, the last being essential for a patient who already suffers pain owing to the disease.
The objectives of laparoscopic ablation or excision of endometriotic lesions include pain relief, improved fertility, and improved patient quality of life [18]. It is imperative to remove all visible lesions and to biopsy any doubtful lesions to reduce the chance of recurrence and reoperation [19]. However, even with complete resection, the recurrence rate is high [19]. Fibrotic tissue surrounding the lesions should be removed as well because the tissue is reactive to hormones and can lead to recurrence of disease [19].
The main indications for laparoscopic surgery are pain, pelvic pain refractory to pharmacologic treatment, severe disease with anatomic distortion, large endometriomas, bowel involvement, urinary obstructions, contraindication for hormone therapy, and potential malignant disease. There is also scientific evidence supporting the benefits of laparoscopic surgery in infertile endometriosis patients who have previously failed to conceive spontaneously or by in vitro fertilization (IVF). Laparoscopic surgery has been shown to increase pregnancy outcome [20].
The first step of laparoscopic treatment should always be a diagnostic procedure, despite previous image evaluation. Careful analysis of pelvic anatomy during surgery can help with more precise excision of lesions and in classification of disease stage. Many implants are called “iceberg lesions,” when the deep level of the disease is not consistent with its superficial laparoscopic appearance, another reason to insist on a complete examination of pelvic lesions.
There are two possible surgical approaches: conservative and complete. Conservative surgery consists of maintaining the uterus and as much of the ovarian tissue as possible in order to preserve fertility. On the other hand, complete surgery is characterized by total removal of the uterus with or without removal of the ovaries. According to the ASRM, the indications for a complete surgery are recurrent conservative surgeries, disabling pain without reproductive desire, and associated uterine diseases that must be treated with hysterectomy [21].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








