Eric J. Silberfein
DEFINITION
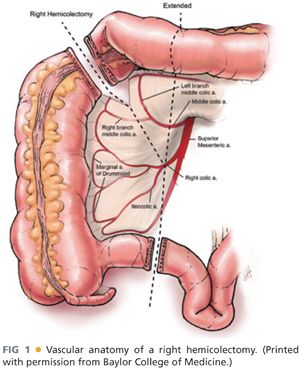
■ Right hemicolectomy refers to the removal of the cecum, the ascending colon, the hepatic flexure, the proximal portion of the transverse colon, and part of the terminal ileum (FIG 1). It is the standard surgical treatment for malignant neoplasms of the right colon and involves ligation of the ileocolic, right colic, and right branch of the middle colic vessels.
DIFFERENTIAL DIAGNOSIS
■ Various benign and malignant conditions require right hemicolectomy. The most common indication is a mass in the right colon. Other indications include neoplasms of the cecum or appendix. Benign conditions for which right hemicolectomy is performed include adenomatous polyps that cannot be removed endoscopically, cecal volvulus, inflammatory bowel disease, and right-sided diverticulitis, among others.
PATIENT HISTORY AND PHYSICAL FINDINGS
■ A thorough history and physical examination is mandatory.
■ Findings such as ascites or diffuse adenopathy may result in additional diagnostic workup to rule out metastatic disease and this may alter the overall care plan for the patient.
■ A baseline nutritional and functional status should also be ascertained in the preoperative setting.
■ Previous abdominal surgeries should be noted.
■ A thorough family history, including history of colonic polyps and cancers, should be obtained.
IMAGING AND OTHER DIAGNOSTIC STUDIES
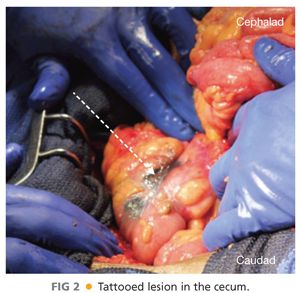
■ A full colonoscopy should be obtained to examine the remainder of the colon, which has up to a 5% chance of synchronous disease. Colonoscopy can also allow for India ink tattooing of the lesion to facilitate accurate intraoperative localization (FIG 2).
■ Preoperative imaging also includes high-quality dual phase computed tomography (CT) imaging of the abdomen and pelvis to not only assess for metastatic disease but also to evaluate the primary tumor’s relationship to nearby structures such as the kidney, ureter, duodenum, and nearby vessels such as the vena cava, superior mesenteric vessels, and middle colic vessels. Tumors that involve adjacent organs require additional preoperative planning and consultation with ancillary services may be necessary. Attempts at en bloc resection should be made in cases where the tumor involves adjacent organs or structures.
■ Additional workup includes a CT of the chest, complete blood cell count, and comprehensive metabolic panel. A baseline carcinoembryonic antigen (CEA) level should be obtained to assist with postoperative surveillance for recurrence. Positron emission tomography (PET)-CT is not routinely indicated.
SURGICAL MANAGEMENT
Preoperative Planning
■ Preoperative bowel preparation is not mandatory but it may make manipulation of the colon more manageable. If intraoperative colonoscopy is required, a prepped colon would also be preferred.
■ Preoperative antibiotic prophylaxis for skin and bowel flora is recommended. Intravenous broad-spectrum antibiotics that contain second- or third-generation cephalosporins (such as cefoxitin or ceftriaxone) or fluoroquinolones (such as ciprofloxacin) along with metronidazole will adequately cover gram-negative and anaerobic pathogens. Alternatively, ertapenem, a carbapenem with activity against gram-positive, gram-negative, and anaerobic flora, can be used. Prophylactic antibiotics should be at therapeutic bloodstream levels at the time of incision. Redosing the antibiotic should be considered when taking into account the length of the operation, the estimated blood loss, and the half-life of the antibiotic.
■ Venous thromboembolic prophylaxis for patients undergoing right hemicolectomy includes both mechanical interventions, such as pneumatic compression devices, and pharmacologic interventions, such as low-molecular-weight heparin or unfractionated heparin. These agents should be delivered prior to induction of anesthesia as the dramatically decreased level of vascular tone associated with anesthesia results in venous stasis and risks thrombosis. Patients on preoperative warfarin should be transitioned to either low-molecular-weight or unfractionated heparin.
■ Preoperative thoracic epidural placement for postoperative pain control should be offered to patients without contraindications to this form of analgesia. Epidural pain control reduces narcotic requirements postoperatively and decreases risk of postoperative ileus and pulmonary complications. Otherwise, patient-controlled analgesia is preferred. Intravenous nonsteroidal antiinflammatory drugs (NSAIDs) should also be considered in the perioperative period to decrease the use and side effects of narcotic analgesia.
■ Ancillary surgical services may be required to assist in the patient’s care for procedures such as preoperative placement of ureteral stents or assistance in resection or reconstruction of involved adjacent organs, such as the kidneys, ureters, or the duodenum.
TECHNIQUES
ANESTHESIA AND PATIENT POSITIONING
■ General endotracheal anesthesia is preferred for right hemicolectomy. However, spinal anesthesia alone is feasible if necessary.
■ The patient is placed supine with or without the arms tucked.
■ After induction of anesthesia, the bladder is catheterized and an orogastric tube is placed.
■ The entire abdomen is prepped and draped.
■ The surgeon stands on the patient’s right and the first assistant on the left.
INCISION
■ A midline laparotomy is made.
■ Upon entering the abdominal cavity, inspect for evidence of metastatic disease. The liver should be palpated for masses and biopsied as needed, and the small bowel eviscerated and inspected from the ligament of Treitz to the ileocecal valve. The colon and rectum should be inspected and palpated. The omentum and peritoneum should be evaluated for tumor implants or carcinomatosis. In women, the ovaries should also be inspected for abnormalities.
RIGHT COLON MOBILIZATION
■ Placement of self-retaining retractors, such as a Balfour, may be used to improve exposure. Otherwise, the abdominal wall is retracted with handheld instruments.
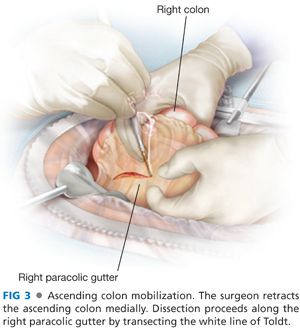
■ The cecum and ascending colon are freed from the peritoneal reflection by incising along the white line of Toldt (FIG 3). The terminal ileum is also freed from the retroperitoneum and mobilized by incising the peritoneum along the root of the mesentery.
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








