■ Two laparoscopic high-definition screens, one on each side of the OR table, are used.
■ We use a bariatric length, 10-mm 30-degree camera. If needed, we use a right-angle adaptor for fiberoptic attachment to the camera to avoid conflict of the fiberoptic cord with other laparoscopic instruments. Using camera heaters and a smoke evacuator channel can avoid the need for repeated camera cleansing, leading to a decrease in operative length.
■ We use two bariatric length laparoscopic bowel graspers, laparoscopic scissors, and bariatric length laparoscopic 5- to 10-mm suction irrigation.
■ We prefer to use a bariatric length laparoscopic energy device such as the 43-cm LigaSure 5-mm device. Energy devices that produce excessive moisture or fog may impair visibility.
■ Laparoscopic Endoloop polydioxanone (PDS) for the ileocolic vascular pedicle
■ Staplers
■ Linear GIA 100-mm, triple blue staple lines for the ileal pouch formation
■ A 28- to 29-mm circular stapler for a stapled ileoanal pouch anastomosis
■ A 60-mm Endo GIA for distal division of the rectum as indicated
■ A second set of instruments is necessary for an extracorporeal anastomosis.
Patient Positioning
■ The patient is placed on modified lithotomy position on Allen stirrups with arms tucked (FIG 1). The patient is secured to the table, with foam pad placed under the patient’s torso and with Velcro or broad tape placed across the chest. Rolled surgical towel is placed under the sacrum to elevate the pelvis and assist with the coloanal or ileoanal anastomosis.
■ A Foley catheter is inserted and taped over the right thigh in order to avoid urethral trauma with the OR table tilting.
■ A bear hugger or other thermal device is applied to the chest and legs.
■ A protecting foam pad is placed over the head to protect from injury with laparoscopic instrument positioning.
■ We recommend using laparoscopic draping with side plastic bags or pockets to allow for bariatric instrument placement. All laparoscopic cords and energy device cords are brought out via the patient’s upper chest.
TECHNIQUES
DIAGNOSTIC LAPAROSCOPY—SINGLE MULTICHANNEL PORT TECHNIQUE
■ A 2.5-cm circular incision is performed at the right lower quadrant (RLQ) premarked temporary ileostomy site. Alternatively, a 3.5-cm periumbilical vertical midline incision is performed. A wound protector is inserted, followed by attachment of the single-incision laparoscopic surgery (SILS) port (FIG 2A,B).
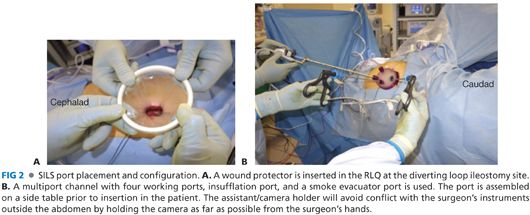
■ Assemble all channels of the SILS port on the back table to avoid losing parts outside the sterile field. Insert the laparoscopic multichannel single port with a wound protector. Insufflate pneumoperitoneum carbon dioxide (CO2) to 15 mmHg of pressure.
■ Perform a diagnostic laparoscopy. The surgical assistant/camera holder and the surgeon stand by the patient’s right side when addressing the left colon, sigmoid, or rectum and by the patient’s left side when addressing the right colon. For the transverse colon mobilization, either side may be suitable or the surgeon may be positioned between the patient’s legs. Tilt the OR table to a steep Trendelenburg position and airplane it to the left or right for maximum exposure.
■ Minimize excursion/cluster effect around hands and camera between the surgical assistant and operating surgeon with adherence to the principle that the surgeon should position his or her assisting (nondominant hand) instrument’s distal tip (used for grasping, retracting, or suctioning) as close as possible to his or her operating (dominant hand) instrument’s (i.e., energy device) tip. This distance should be about 3 to 4 cm between the two instruments’ tips. For example, hold the ileocolic vascular pedicle just above the site of the division site rather than holing the cecum itself, which is far more distant from the pedicle. This technique allows achieving a wide angle between the two instruments outside the abdomen as they exit and cross via the single port, thus minimizing instrument conflict effect between the surgeon’s hands.
■ The assistant/camera holder will avoid conflict with the surgeon’s instruments outside the abdomen by holding the camera as far as possible from the surgeon’s hands and by using the camera’s 30-degree angulation for side view as well as the zoom-in option (FIG 2B).
■ Minimize the need for frequent laparoscopic instrument exchange, such as exchanging of graspers with monopolar laparoscopic scissors. Instead, consider using multiuse energy devices that provide dissection and sealing-cutting capabilities, thus allowing constant progress in the operating field and significant time saving.
■ The surgeon and the assistant can either switch sides during the various steps of the procedure or just rotate the single port clockwise or counterclockwise while the instruments stay in the abdomen under direct visualization with the camera, thus achieving different camera angles, better exposure, and better visualization.
■ The OR table can also be tilted accordingly during the various steps of the procedure to increase the exposure and prevent instrument conflict.
MOBILIZATION OF THE RIGHT COLON: PRESERVATION OF THE ILEOCOLIC VASCULAR PEDICLE
■ The patient is positioned in a steep Trendelenburg position with the OR table tilted maximally toward the patient’s left side. The surgeon is standing on patient’s lower left side using a grasper in the nondominant hand and the energy device on the dominant hand. The camera holder stands cephalad to the surgeon.
■ If the omentum is adherent medially to the hepatic flexure or the ascending colon itself, we start the procedure with the dissection of the omentum off the colon. We may perform omentectomy by including the omentum with the transverse colectomy.
■ Dissect the terminal ileal retroperitoneal attachments and mobilize it toward the midline (FIG 3), exposing the origin of the superior mesenteric artery and the third and fourth portions of the duodenum. Morbidly obese patients require a generous terminal ileal medial mobilization to allow for a tension-free ileoanal pouch anastomosis.

■ Proceeding from a caudad to cephalad direction, dissect the ascending colon mesentery off its retroperitoneal attachments without entering Gerota’s fascia and preserving the right gonadal vessels and the right ureter intact. Dissect the ascending colon mesentery off the second and third portions of the duodenum in an atraumatic fashion.
■ Using an energy device, we hemostatically divide the ascending colon mesenteric vascular arcade while protecting the ileocolic vascular pedicle up to the mesenteric level of the ileocecal valve (FIG 4). This is critical to ensure a good blood supply to the pouch. Avoiding an ileocolic mesenteric bleeding or hematoma is crucial for preservation of the vascular supply to the ileal J-pouch.
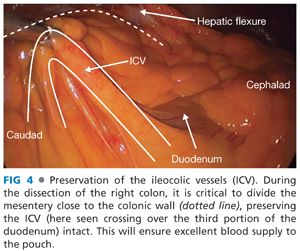
■ Divide with the energy device the ascending colon mesentery flush to the ileocolic vascular pedicle (staying close to the colonic wall), up to the mesenteric border of the terminal ileum at the selected site of proximal intestinal division, just proximal to the ileocecal valve.
■ Proceed with laparoscopic division of the incidental right colonic artery/vein if present.
■ Mobilize the ascending colon medially by transecting the white line of Toldt.
MOBILIZATION OF THE TRANSVERSE COLON
■ The surgeon stands in between the patient’s leg. Place the patient on Trendelenburg and keep the OR table tilted to the left for the proximal transverse colon mobilization or to the right for the distal transverse colon and the splenic flexure mobilization. Alternatively, we may place the patient on reverse Trendelenburg for exposure and the assistant may use a laparoscopic grasper to assist with the retraction—“tenting”—of the transverse colon.
■ Enter the lesser sac via the antimesenteric border of the proximal transverse colon and perform a hepatic flexure mobilization by dividing the hepatocolic ligament with the energy device (FIG 5).

■ Divide the gastrocolic ligament adjacent to the mesenteric border of the transverse colon while preventing inadvertent injury of the gastroepiploic arcade.
■ The omentum may be included with the transverse colon into the specimen.
■ Dissect the root of the hepatic flexure and proximal transverse colon mesentery and identify the origin of the middle colic artery and vein. Using an energy device, divide the middle colic vascular pedicle at the root of the mesocolon while holding the stump with a grasper to avoid retraction or residual bleeding (FIG 6).
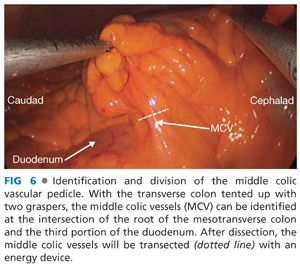
■ Place hemostatic clips or Endoloop PDS at the divided stump to secure the hemostasis. There is no need to use an Endo GIA stapler, unless severe atherosclerosis or vessels larger than 7 mm in size are present, which preclude usage of an energy device.
■ Complete the dissection of the root of the distal transverse mesocolon off the retroperitoneum, pancreas, and fourth portion of the duodenum with the energy device.
SPLENIC FLEXURE MOBILIZATION, LEFT COLECTOMY, AND SIGMOID COLECTOMY
■ The surgeon stands on the patient’s right side and caudally to the assistant, with the OR table tilted to the right.
■ Start the dissection of the root of the sigmoid mesocolon off the retroperitoneal attachments by dissecting dorsal to the superior hemorrhoidal vessels (FIG 7A). Identify and preserve the left ureter (FIG 7B), gonadal vessels, and hypogastric nerves intact.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








