■ This position is defined as Trendelenburg position with legs apart.
■ The thighs are level with the abdomen as this allows efficient placement of a self-retaining retractor without creating excessive pressure between the retractor and the patient’s thighs.
■ All pressure points are padded to avoid potential neurovascular injuries.
■ The perineum is positioned flush with the edge of the operating room table for easy access during the perineal phase of the operation.
■ The pelvis is supported with a folded sheet to lift the entire perineum and facilitate exposure during the perineal dissection.
■ The arms are placed in a neutral position and supported with suitable armrests or tucked to the side.
TECHNIQUES
PLACEMENT OF INCISION
■ A midline vertical incision is made.
■ A suitable laparotomy retractor is inserted.
■ After general inspection to see if there are any contraindications to performing RP/IPAA, the small bowel is packed with moist large swab packs into the upper abdominal cavity.
MOBILIZATION OF THE RIGHT COLON: PRESERVATION OF THE ILEOCOLIC VASCULAR PEDICLE
■ The surgeon stands to the patient’s left side. The patient is placed on a Trendelenburg position with the right side up to facilitate exposure.
■ A full Cattell-Braasch maneuver is performed to mobilize the right colon of its retroperitoneal attachments.
■ The cecum and ascending colon are freed from the peritoneal reflection by incising along the white line of Toldt (FIG 2). The terminal ileum is also freed from the retroperitoneum and mobilized by incising the peritoneum along the root of the mesentery.

■ As the colon and terminal ileum are reflected anteriorly and medially, the right gonadal vessels and right ureter should be identified in the retroperitoneum and not mobilized anteriorly so as to avoid injury.
■ The lateral dissection is carried sharply up and around the hepatic flexure in the avascular, embryologic plane between the mesocolon and the duodenum. The second and third portions of the duodenum are identified near the hepatic flexure and injury to this structure must be avoided.
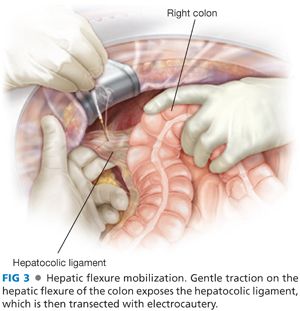
■ The hepatocolic ligament is transected (FIG 3).
■ Using an energy device, we hemostatically divide the ascending colon mesentery between the mesenteric vascular arcade and the colon wall (FIG 4) while protecting at all times the ileocolic vascular pedicle up to the mesenteric level of the ileocecal valve. This will allow excellent prograde blood supply to the pouch later on. Avoiding an ileocolic mesenteric bleeding or hematoma is crucial for preservation of the vascular supply to the ileal J-pouch.
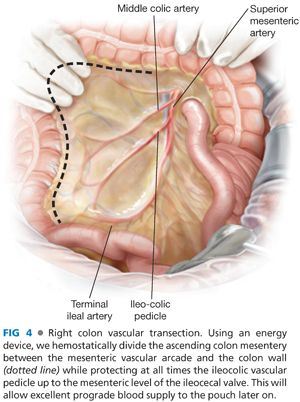
■ The mesenteric division extends from the midtransverse colon down to the mesenteric border of the terminal ileum at the selected site of proximal intestinal division—just proximal to the ileocecal valve.
TRANSVERSE COLON MOBILIZATION
■ The gastrocolic ligament is exposed as the assistant retracts the greater omentum superiorly while the surgeon retracts the transverse colon anteroinferiorly.
■ Diathermy is used to separate the greater omentum from the anterior leaf of the transverse mesocolon.
■ Mobilization of the spleen needs to be approached from both sides to facilitate ease of mobilization of the splenic flexure (FIG 5). The patient is placed on a reverse Trendelenburg position with the left side up to allow the spleen to come down into the surgical field.

■ Once the gastrocolic ligament has been completely transected, transection of the lateral peritoneal attachments (phrenocolic ligament) allows for lateral mobilization of the splenic flexure.
■ At this point and from the right side of the table, the surgeon hooks the splenocolic ligament anteriorly with his or her right index finger, exposing the ligament adequately for the assistant to transect it using electrocautery. The splenocolic ligament is divided as close to the colon as feasible, avoiding undue traction on the spleen.
DESCENDING COLON MOBILIZATION
■ The surgeon stays on the right side of the table. The patient is placed on Trendelenburg position with the left side up.
■ The descending colon is mobilized by medial traction and dissection along the left paracolic gutter using diathermy.
■ The colon is mobilized from the retroperitoneum using a lateral to medial approach.
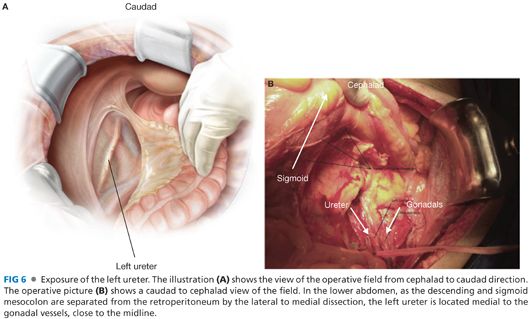
■ Care is taken to identify, and avoid damage to, the left gonadal vessels and left ureter (FIG 6). In the lower abdomen, the left ureter is located medial to the gonadal vessels, close to the midline.
INFERIOR MESENTERIC ARTERY TRANSECTION
■ With the assistant holding the proximal and distal sigmoid colon up, the root of the mesosigmoid colon is clearly visualized by the surgeon from the right side of the table. At the root of the mesentery, the arch of the superior hemorrhoidal vessels (SHV) can be seen and palpated.
■ Placing the index finger behind the SHV arch allows the surgeon to incise with electrocautery the right surface of the peritoneum just under the dorsal surface of the SHV.
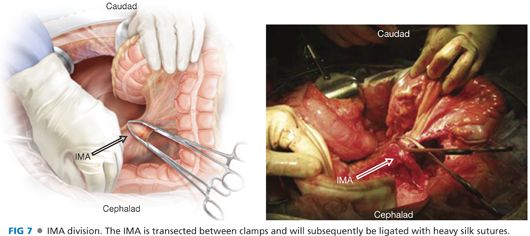
■ This plane of dissection along the dorsal aspect of the SHV is carried distally over the promontory (leading into the presacral space) and proximally, up to the origin of the inferior mesenteric artery (IMA). The IMA is dissected circumferentially at its origin from the aorta.
■ The IMA is then ligated between Sarot clamps, incised, and doubly ligated with braided 2-0 suture (FIG 7).
PROCTECTOMY
■ The posterior pelvic dissection is performed first. Using a lighted St. Mark’s retractor for exposure, the presacral fascia is entered between the investing layer of fascia propria of the mesorectum and presacral fascia (FIG 8).

■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








