and Hubert Lepidi1
(1)
UER Médecine, Aix-Marseille Université, Marseille, France
Abstract
The topographical anatomy of the bulbo-clitoral organ was already partially covered in the first chapters, with its morphology and structure having been observed in situ, i.e. within the external feminine genitalia. However, several points remain to be clarified and very specific connections have yet to be studied. We will discuss the connections with the vestibule, labia and greater vestibular glands; the connections with the urethra, the vagina and the perineal membrane; and finally, the relations with the pelvic diaphragm (levator ani muscles).
13.1 General
The topographical anatomy of the bulbo-clitoral organ was already partially covered in the first chapters, with its morphology and structure having been observed in situ, i.e. within the external feminine genitalia. However, several points remain to be clarified and very specific connections have yet to be studied. We will discuss the connections with the vestibule, labia and greater vestibular glands; the connections with the urethra, the vagina and the perineal membrane; and finally, the relations with the pelvic diaphragm (levator ani muscles).
13.1.1 Connections with the Vestibule
13.1.1.1 Position of the Bulbs
These connections mainly involve the bulbs for which we have already examined the naming difficulties. Are the spongy bulbs pressed against the walls of the vestibule or do they go deeper? Against the terminal urethra? Against the end of the vaginal duct?
L. Kobelt, who first gave an exact and complete description of the bulbo-clitoral organ, was also the first to replace the older terminology (plexus retiform, plexus reticular) with the name “vestibular bulbs”. But a semantic ambiguity should immediately be noted as this author explains why he calls them as such since the formations “are not located around, but at the entry to the vagina”. Is this enough to abandon the terminology “vaginal bulbs”? The reality is in fact more complex and only frontal sectioning of the external genitalia makes it possible to reveal the details of bulb topography: The result of these sections is incontrovertible. The bulbs are directly connected not only to the urethral and vaginal orifices but also to the parts preceding it, i.e. the vestibule and the base of the labia minora and what follows the entire distal part of the vagina (Fig. 13.1) and the end of urethra. In other words, the terms “vestibular bulbs”, “vaginal bulbs” and “urethral bulbs” all have an element of truth and remain perfectly valid. However, it is the term “vestibular bulbs” that was retained by the Nomina Anatomica. We would have preferred “spongy bulbs in women” (or female spongy bulbs) which is more general and less subject to discussion. Please note, however, that the terminology now present in the nomenclature is in accord with Kobelt, thus paying homage to this author. As for choosing which of the adjectives “urethral” or “vaginal” is best suited for describing the bulbar topography, let us agree that there is no cause for debate. The sections clearly show that the two adjectives are true since the bulbs border the external orifices of both ducts. However, for the urethra, 3/4 of the circumference of its external orifice is lined by spongy bulbar tissue, whereas for the vaginal orifice, only the lateral parts are lined by this tissue. It should also be noted that the bulbs are of varying length and often asymmetrical, such that the lateral walls of the vagina may not be entirely lined by the bulbs or one of the walls may be lined to a greater extent than the other! Finally, let us recall the terminology proposed by H.E. O’Connell et al.: “clitoral bulbs”, which cannot be supported from a semantic point of view given that the clitoris and bulbs are two different parts of a whole. In the interest of accuracy, one should therefore refer to “bulbs of the bulbo-clitoral organ” or “genital bulbs” which are easier to express.
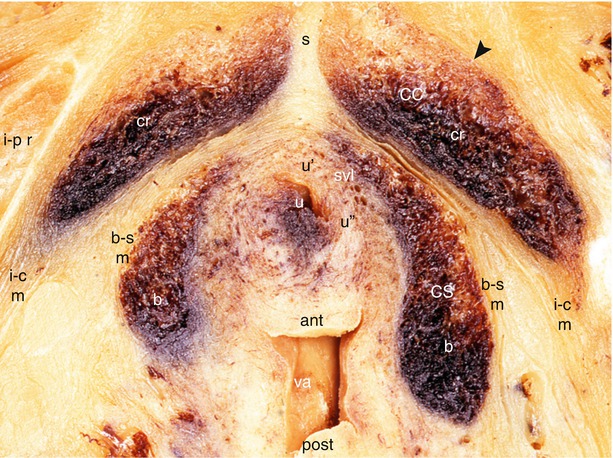
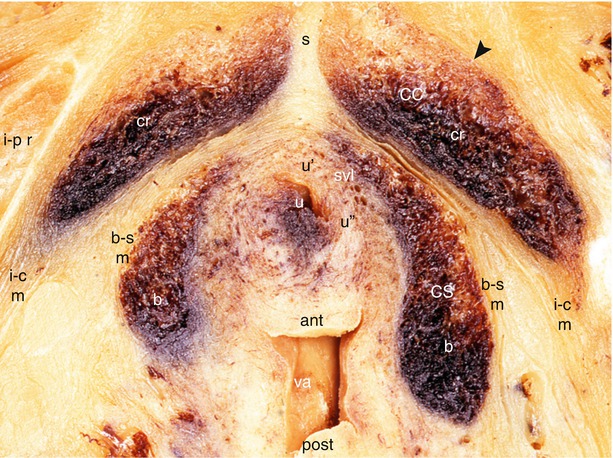
Fig. 13.1
Relationships between both the urethra and vagina with female erectile bodies. Tranverse section of female pelvis through the anterior perineum. ant anterior vaginal wall, b bulb, b–s m bulbo-spongiosus muscle, CC corpus cavernosum, cr crus clitoridis, CS corpus spongiosum, i–c m ischio-cavernosus muscle, i–p r ischio-pubic ramus, post posterior vaginal wall, s septum of the crura, svl superficial vascular layer (of urethra), u urethra, u′ anterior wall (of urethra), u′′ lateral wall (of urethra), va vagina, Black arrowhead it points the clitoral albuginea. Note the close relationship between the bulbs and the urethro-vaginal pyramid
13.1.1.2 The Greater Vestibular Glands
On either side of the vestibule, the spongy bulbs connect with the two greater vestibular glands or Bartholin’s glands.1 These glands are well known to gynaecologists and their patients due to their frequent infection (bartholinitis may be the manifestation of a sexually transmitted infection, notably the infection caused by gonococcus: gonorrhoea). These muciparous glands are topographically in contact with the posterior extremity of the bulbs. The glands have an average diameter of 15 mm, a more or less spherical, slightly flattened shape, sometimes ovoid, with an irregularly mammillated surface. Their firm consistency allows them to be easily identified upon palpation during dissection. However, strong adherence of the gland to the adjacent cell tissue renders its release difficult. This notion is also demonstrated during surgical release in view of exeresis of this gland, which is made all the more difficult due to the significant inflammatory adherences. The gland has very tight connections with the swollen posterior part of the bulb (Fig. 13.2), connections that the surgeon must be very aware of so as to avoid often serious haemorrhaging due to injury to the homolateral spongy bulb. The gland may be located to the rear and simply tangent to the convexity of the bulb’s swollen extremity. More often, it is inserted into this extremity, carving out a sort of bulbar cavity in which it is housed. The vestibular gland may therefore be described as follows: an anterior extremity directed towards the external orifice of the vagina; a posterior extremity connected to the superficial transverse muscle; one medial vulvar surface that is more or less concave; a convex lateral surface facing, but at a distance from, the initial tapered pillar of the clitoris; a superior edge pressed against the inferior fascia of the urogenital diaphragm; and an inferior edge in contact with the superficial transverse muscle. The bulbospongiosus muscle is applied to the inferior edge and then to the inferior surface of the bulb, as seen previously. The excretory duct2 measures 1–2 cm. Its diameter can reach 2 mm. Slanted forward and inward, it opens into the vestibular sulcus3 along the insertion of the hymen or its carunculate remnants (carunculae hymenales), at the junction of the anterior 2/3 and posterior 1/3 of the vestibule. The secretion produced by this gland (tubulo-alveolar gland from a histological perspective) is a transparent or opalescent, runny mucus. It is secreted during coitus and contributes to lubrication of the walls of the external genitalia.4 The neurovascular connections of the greater vestibular gland are lateral. The neurovascular bundle (Fig. 13.2) engaged above the lateral surface of the gland includes rami of the deep perineal artery (bulbar artery), voluminous veins and the deep ramus of the pudendal nerve perineal branch.
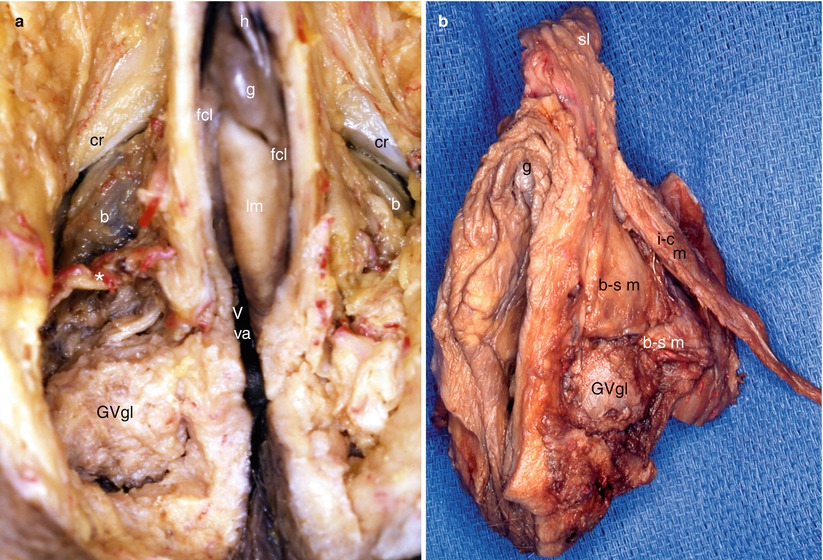
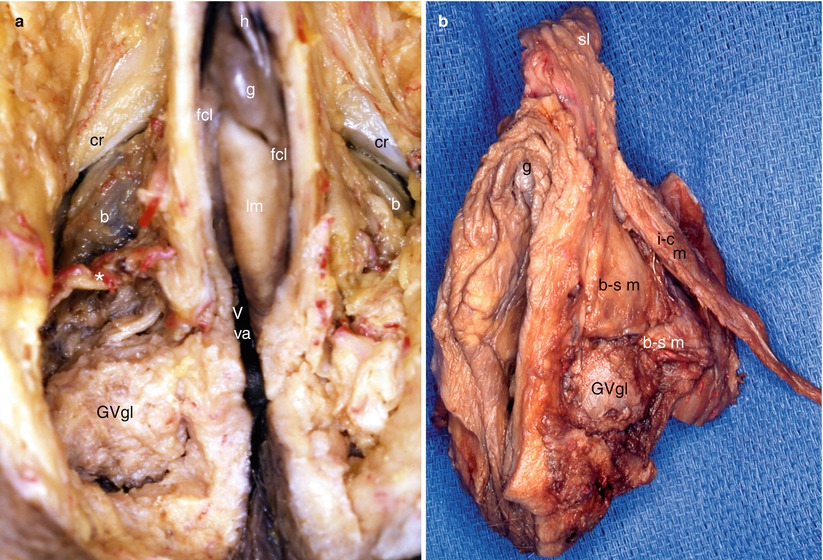
Fig. 13.2
Two dissections of the anterior perineum to show the close relationship between the bulbs and the greater vestibular glands (Bartholin’s glands). (a) Anterior view showing the right great vestibular gland behind the right bulb; notice the neurovascular bundle* (bulbar artery and rami from the pudendal nerve’s perineal branch) engaging obliquely in front of the gland. (b) Lateral left view showing a left great vestibular gland, behind the left bulb covered by the bulbospongiosus muscle. b bulb (with bulbospongiosus muscle), b–s m bulbospongiosus muscle (black legend medial part of the muscle, white legend lateral part), cr crus of clitoris, fcl frenum (frenulum clitoridis), g glans clitoridis, h hood, lm labium minus (lesser lip), GVgl greater (or major) vestibular gland (Bartholin’s gland), Vva vestibule of vagina
13.1.2 Connections with the Urethra
These connections are exceptionally important and had surprising consequences from an anecdotal point of view (see Chap. 1). Despite the shortness of this duct, we now know the various parts of the feminine urethra well (Fig. 13.3) and notably the part that is connected to the bulbo-clitoral organ: It is the distal part of this duct, immediately beyond the posteroinferior edge of the pubic symphysis and more accurately immediately beyond the passage through the urogenital diaphragm. This is therefore the extra-pelvic portion of the urethra. This part, called the “distal urethra”, very thoroughly evaluated by J.O.L. Delancey, corresponds to the terminal segment extending from 79 % of the total length of the duct to the external orifice (situated at “100 % of the length”). If we take the average length of the female urethra to be 3 cm (extremes: 25–44 mm), the distal urethra only represents 0.8 cm! Serial sectioning of this short segment, perpendicular to the urethral axis, allowed us to gain very precise information to complete the general notions that appeared during dissection.
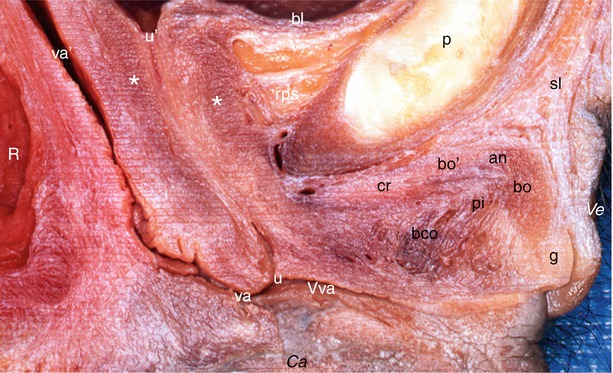
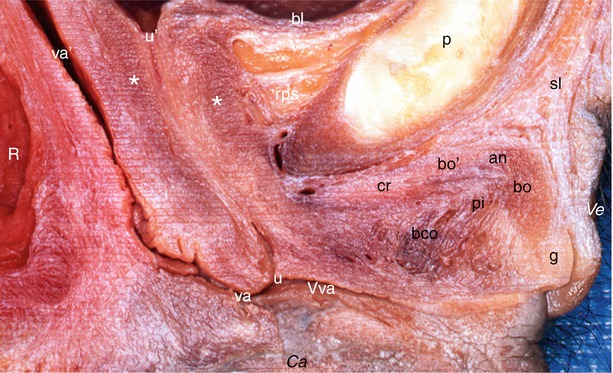
Fig. 13.3
Part of a median sagittal section through the female pelvis showing the location of the bulbo-clitoral organ and its immediate surroundings. Ve ventral, Ca caudal, an angle (elbow), bco bulbar commissure, bl bladder, bo clitoral body (descending part), bo′ clitoral body (ascending part), cr crus clitoridis, g glans, pi pars intermedia of Kobelt, p pubic symphysis, R rectum, rps retro-pubic space, sl suspensory ligament, u external urethral orifice, u′ internal urethral orifice, va vaginal orifice (introïtus), va′ vagina, Vva vestibule of vagina, white asterisks external sphincter urethrae
We were able to observe deep and superficial connections during dissection.
Observation of deep connections first requires dissection of the bulbo-clitoral organ. The organ has to be pushed back and down with a fair amount of force (thus sacrificing the two thin cavernous nerves) in order to access the thin subpubic urethral plate (or supra-urethral lamina). This lamina continues from the retro-crural fascia (see Chap. 5). The underlying urethral duct can be felt through the lamina with a fingertip. As soon as the transversal incision is made in the lamina, the urethra appears (Fig. 13.4). The duct will then pass through the urogenital diaphragm behind the transverse perineal ligament. It is now becoming perineal. It appears as a cylindrical tube, slightly widened, with a thick wall.
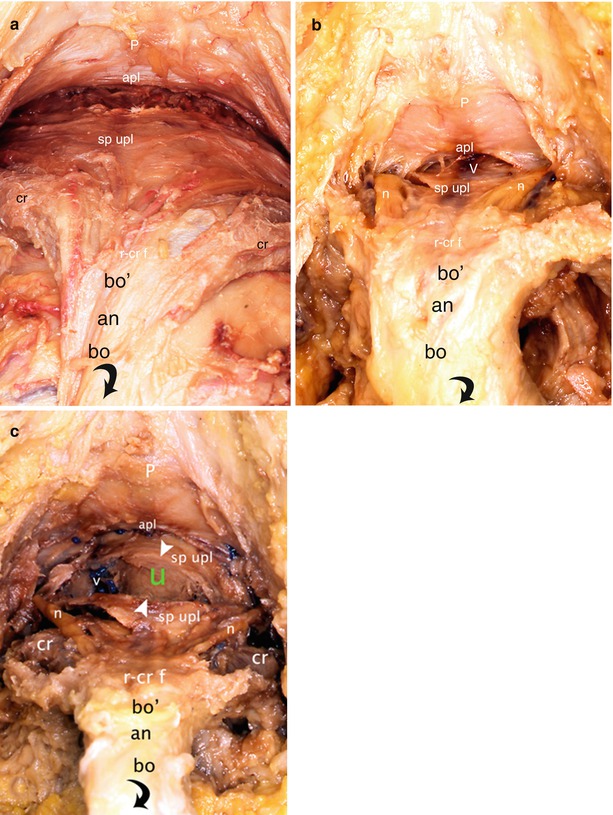
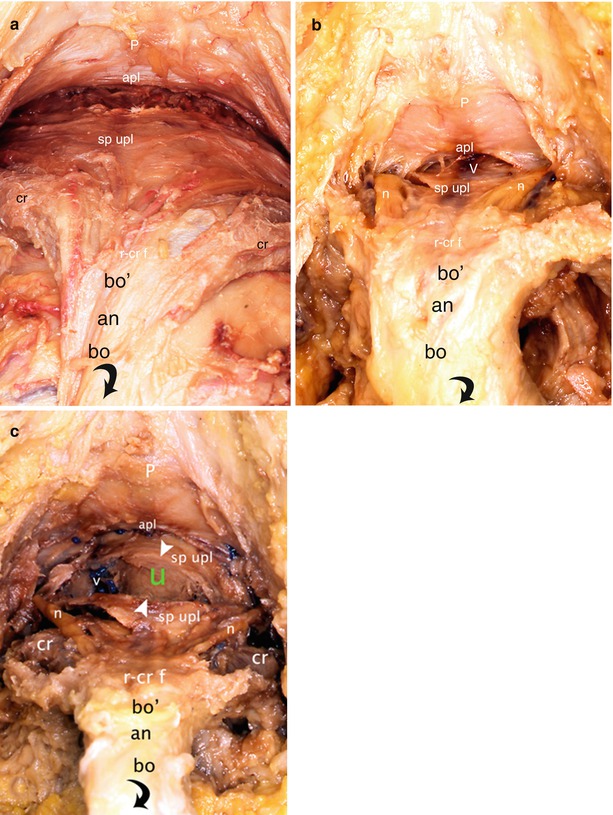
Fig. 13.4




Dissections of the pre- and infra-pubic areas to show the relationship between the dorsal parts of the bulbo-clitoral organ and the urethra (bird’s eye views). The clitoral body has been retracted back and down (black curved arrow). (a, b) Gradual release of the subpubic urethral plate. (c) Transversal incision of the subpubic urethral plate highlighting the urethra. an angle, apl arcuate pubic ligament, bo′ ascending part of the clitoral body, bo descending part of the clitoral body, cr crus clitoridis, n dorsal nerve of clitoris, P pubic symphysis, r–cr f retro-crural fascia, sp upl subpubic urethral plate, u (green) urethra, V deep vein of the clitoris (seen by transparency through the sp upl), v right latero-urethral venous plexus, white arrowheads they show the two banks of the subpubic urethral plate cut transversally
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








