Recurrent Hernia in the Morbidly Obese
David B. Earle
The indications and contraindications for treating any disease process are the same, and the treatment of recurrent hernia in the morbidly obese patient is not different. The indications are either the relief of symptoms, or the prevention of future problems. It is therefore important for the surgeon to establish exactly what symptoms the patient feels are related to the hernia, the likelihood that the symptoms are related to the hernia, and the severity of the symptoms, particularly those limiting quality of life in a negative way. It is also important for the surgeon to put the potential deleterious effects of untreated hernia disease in a proper perspective in an unbiased manner. By way of example, a physician may tell a patient with a small asymptomatic hernia at the umbilicus that no treatment is necessary unless the hernia becomes bothersome. On the contrary, the physician may relate a story of a patient with a small umbilical hernia that became acutely incarcerated, requiring emergency surgery. This example illustrates how easy it is for the surgeon to influence the patient’s decision with anecdotal evidence, and how important it is to clearly establish the possible outcomes, risks, and potential benefits, of observation versus treatment in an unbiased manner.
For hernia disease, common problems related to existing hernias of any size include pain (mild, moderate, or severe), enlargement, physical deformity, skin ulceration, difficulty fitting clothes and performing daily activities due to the deformity, and recurrent bouts of acute incarceration. Establishing a direct cause and effect relationship between the hernia and the symptoms is sometimes not possible, and the surgeon should give his or her best estimate.
In summary, the indications for fixing a recurrent ventral hernia in the setting of morbid obesity should be for symptom relief and/or prevention of future problems with the hernia. Relative contraindications to electively repair of recurrent hernia in the setting of morbid obesity include the repair of large defects without some sort of preoperative weight loss, particularly if there is some element of loss of domain. This is also true in the emergency setting where options for repair are limited—for example, operating for the bowel obstruction in the setting of a large, recurrent hernia in the setting of obesity. This type of case may best be treated by simply closing the skin after treating
the bowel obstruction, and leaving the complex hernia repair for another day. These indications and relative contraindications however are not absolute, and highly dependent on the clinical situation. The surgeon must take into account the primary goals and objectives as well as the myriad of individual patient factors when making a treatment decision regarding recurrent hernia in the morbidly obese patient.
the bowel obstruction, and leaving the complex hernia repair for another day. These indications and relative contraindications however are not absolute, and highly dependent on the clinical situation. The surgeon must take into account the primary goals and objectives as well as the myriad of individual patient factors when making a treatment decision regarding recurrent hernia in the morbidly obese patient.
Indications
Relief of existing symptoms
Prevention of hernia-related problems (risk–benefit ratio particularly important)
Relative Contraindications
Elective repair of large defects (greater than 10 cm between rectus muscles) without preoperative weight loss and/or smoking cessation
Complex hernia repair in the setting of the treatment of another intraabdominal surgical emergency (skin/subcutaneous tissue closure alone may be appropriate)
The preoperative planning process for recurrent hernia in the setting of morbid obesity is very important. Firstly, it is important to establish the specific goals of the hernia repair for the patient, and then align the surgeon’s goals with those of the patient. Next, it is important to elicit details from previous hernia repairs, particularly infectious related complications. A history of previous mesh infection or wound infection would place the patient in a higher risk category in terms of infectious complications during hernia repair. Additionally, a history of intermittently draining abdominal wall sinus is important as old suture and prosthetic material may harbor pathologic bacteria for many years. Exploration of chronic and intermittent sinus tracts should be performed to search for and remove the foreign body responsible for its persistence. Details of the previous hernia repairs such as suture type and technique as well as prosthetic type and technique are also important to elucidate to avoid performing the same technique, and expecting a different outcome. In addition to reviewing the old operative reports, reviewing the anesthesia record is important to determine the length of the operations, and reviewing the discharge summary will help determine what the postoperative course in length of stay were like. This information is extraordinarily helpful in terms of informing the patient what their anticipated course will be like, as well as for scheduling purposes for both the operating suite and the surgeon. Finally, determining the size of the hernia is important for choosing a technique. For midline hernias, the size should be based on the distance between the medial borders of the rectus muscles. A common error is to determine the size and number of punched out defects within a hernia sac or scar tissue, and ignore the entire area encompassed between the rectus muscles. Treating the patient based on multiple defects within an area rather than the area as a whole may lead to inadequate planning, and poorer outcomes. Abdominal CT scans without enteral or intravenous contrast are the most effective way of determining the distance between the rectus muscles, and the precise size and shape of the defect regardless of location. I consider three categories of midline hernia related to the size, or width between the medial borders of the rectus muscles. “Small” hernias are associated with defects less than 5 cm in width, “medium” sized defects from 5 to 10 cm in width, and “large” defects greater than 10 cm in width.
The surgical procedure is dependent on the specific clinical situation. Once the goals of the operation have been established and aligned, the surgeon must choose the technique that will be most likely to achieve those goals. When considering the
technique, the relative risks and expected benefits of the technique relative to others should be analyzed.
technique, the relative risks and expected benefits of the technique relative to others should be analyzed.
Options for Repair
Open primary repair—not viable
Open repair with prosthetic “inlay”—sewed to the edges of the defect with little (<3 cm) to no overlap—not viable
Open repair with permanent, synthetic prosthetic (sublay or onlay)—viable; relatively higher chance for wound complications compared to laparoscopic repair
Laparoscopic repair with permanent, synthetic prosthetic—viable; low risk of wound complications; technically challenging; does not allow closure of defect for medium to large defects
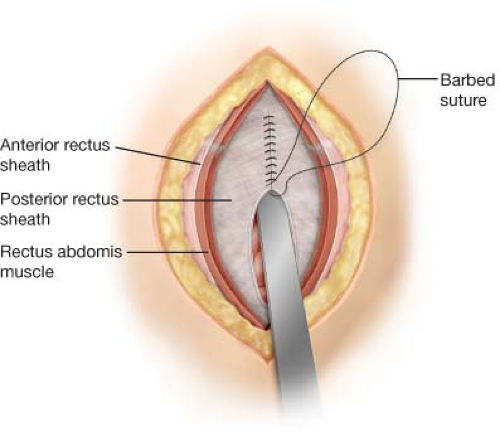
Open repair with component separation and prosthetic (sublay or onlay)—viable; technically challenging; component separation has many varieties; prosthetic choice variable; allows closure of midline with “short-stitch” suturing technique (Figs. 26.1 and 26.2)
Laparoscopic repair with component separation and prosthetic (intraperitoneal)—viable; technically challenging; prosthetic choice variable; laparoscopic assisted techniques with suture passing devices do not allow for fine suture technique to close midline
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree