and Andrea Bischoff1
(1)
Pediatric Surgery, Colorectal Center for Children Cincinnati Children’s Hospital, Cincinnati, OH, USA
15.1 Definition/Frequency
15.2 Associated Defects
15.3 Diagnosis
15.4 Treatment
15.6 Complications
15.7 Functional Results
15.9 Surgical Technique
Electronic supplementary material
Supplementary material is available in the online version of this chapter at 10.1007/978-3-319-14989-9_15.
15.1 Definition/Frequency
Rectovestibular fistula is the most important anorectal malformation in females. This is due to the fact that, by far, it is the most common defect seen in females. Two hundred and ninety of our 1,123 female patients were born with this malformation. Two hundred and seventeen were operated primarily by us, and 73 were reoperations due to a previous failed attempted repair. Interestingly, our series include 531 patients with a cloaca. However, we are convinced that this high number of cloacas in our series is because ours is a referral center. We believe that vestibular fistula is much more common in the general population. Most of the vestibular fistula cases are operated at the place where the babies are born, whereas many cloacas are referred to us due to the complexity of the repair. When this malformation is repaired with a meticulous surgical technique, the recovery of the patients is excellent, and the functional results are also very good. Unfortunately, another characteristic of this malformation is the fact that it is frequently mismanaged. We compared the results obtained in a group of patients that were repaired primarily by us with those of the group that had a secondary procedure due to the fact that the patient underwent a previous failed attempted repair. The difference in terms of bowel control is significantly different. Therefore, we can repeat what other pediatric surgeons through history have said, and that is that “these patients have a single opportunity to have a good repair.”
In the old literature [1] one can find that this malformation received different names, including “anovestibular fistula.” The authors believed that this was a more benign variant of defect and that these patients had a very short fistula and a very low-lying rectum. They also believed that malformation owed to be distinguished from a “rectovestibular fistula,” which has a long, narrow fistula and a rectum located higher in the pelvis, and, therefore, they believed that the prognosis was not as good as the one observed in cases of “anovestibular fistula” [1, 2]. We also found the term “vestibular anus”; the authors believed that some patients were born with an otherwise normal anus located in the vestibule of the female genitalia [2]. We have never seen this type of defect. We do not use those three terms mentioned here, because we found that all our patients with an anal opening located in the vestibule can be repaired with the same surgical procedure and have the same functional prognosis; therefore, we consider the old terminology impractical and misleading. It is true that some patients have a longer fistula than others; those cases may require more dissection to bring the rectum down. However, our results are uniformly good, regardless the type of fistula.
Rectovestibular fistula is a defect in which the rectum opens in the vestibule of the female genitalia. This should not be confused with a rectovaginal fistula. In order for us to call a malformation “rectovaginal fistula,” one must see the anal opening located inside the vagina, deeper to the hymen. Vestibular fistula patients have a normal hymen, and the anal orifice is located posterior to the hymen (Figs. 15.1 and 15.2). The anal opening is visible most of the time, provided the clinician separates the labia of the baby’s genitalia. The newborn female frequently has a significant degree of edema and swelling of that area, considered to be a consequence of the effect of maternal hormones. Therefore, in the newborn baby, it may be a little bit more difficult to see the precise location of the vestibular fistula (Fig. 15.3).

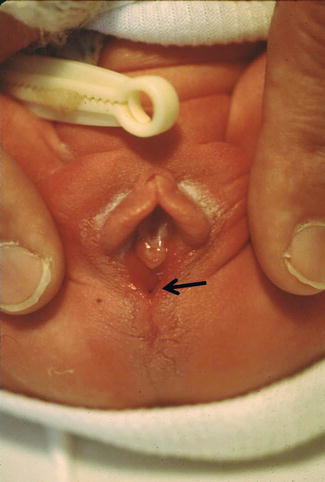
Fig. 15.1
Diagram of vestibular fistula. (a) Sagittal view. (b) Perineum

Fig. 15.2
Picture of a vestibular fistula
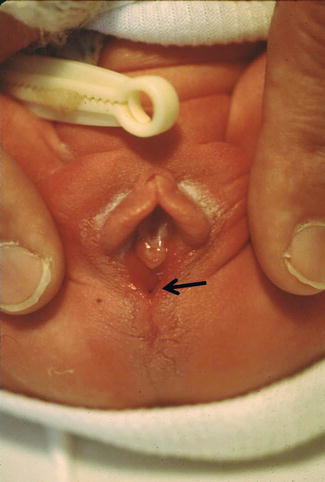
Fig. 15.3
Vestibular fistula in a newborn baby. Arrow shows the fistula site
Some cases of vestibular fistula have the anal opening located rather deep and are almost impossible to see it without general anesthesia. In fact, some patients have a rather small-looking genitalia (vulva) similar to what we see in cases of cloaca. The anal orifice is located very deep in the vestibule, and the urethra is also located deeper than normal, which is what urologists call “female hypospadias.” This particular variant, we call “cloaca type I,” one could also use the term “deep vestibular fistula with a female hypospadias” (Fig. 15.4). We consider this particular type of malformation a transition in between a cloaca and a vestibular fistula.


Fig. 15.4
Deep rectovestibular fistula with female hypospadias – observe small vulva
Some patients are born with the anal orifice located just in between the perineal body (skin lined) and the vestibule, wet tissue (Fig. 15.5). This type of defect is considered intermediate between the vestibular fistula and perineal fistula. The management of these patients is not different from any other type of vestibular fistula. This defect is also known as “fourchette fistula.”


Fig. 15.5
Fourchette fistula
15.2 Associated Defects
A retrospective review of 290 patients with vestibular fistulas operated by us (217 primary and 73 secondary) showed a significant number of associated defects. Since vestibular fistula is considered a malformation representative of the “good side” of the spectrum of anorectal defects in general, the frequency of association of all the defects is rather low. Yet, it is significant enough to be searched for.
15.2.1 Sacral
We were able to measure the sacral ratio in 113 of our cases and found that the average AP ratio was 0.57 and lateral was 0.7. Six percent of these cases had a ratio lower than 0.4. This is consistent with the fact that we consider this malformation a “benign” one, with good functional prognosis. Fourteen cases had a hemisacrum and a presacral mass, and as previously mentioned, presacral masses occur more frequently in lower defects.
15.2.2 Spinal
Approximately, 9 % of our patients had some form of spinal defect, mainly hemivertebra.
15.2.3 Urologic
Ten percent of vestibular fistula cases had a single kidney, which as we know is the most common anatomic abnormality associated to all anorectal malformations, and 13 % of patients had vesicoureteral reflux, which is consistent with the fact that this disorder is the most common functional urologic abnormality seen in anorectal malformation cases. Hydronephrosis was present in 6 % of the cases.
15.2.4 Gynecologic
There are not many reports in the literature, related to this very important assoc [3, 4]. A retrospective review of our patients with vestibular fistula showed that 17 % of them had associated genital anomalies [5]. Eight percent had absent vaginas or vaginal atresia. Figure 15.6 shows the different types of absent vaginas or vaginal atresias encountered.
Fig. 15.6
Vestibular fistula with absent or partially absent vagina. (a) Photograph. (b) Diagram of a sagittal view and one type of repair, using the rectum to replace the vagina. (c) Diagram showing the internal genitalia of a patient with a high vaginal atresia, with a piece of colon. (d) Diagram showing an absent vagina as well as the uterus, the vagina totally replaced with colon. (e) Two types of vaginal atresia. Prepuberty and postpuberty
Figure 15.6a shows the perineum of one of these patients, and there is no vaginal opening. Figure 15.6b shows a diagram of a sagittal view and the type of repair that we used, consisting in leaving the rectum attached to the urethra, to function as a neovagina and pulling the upper rectum down to the perineum.
Eighty percent of the patients with vestibular fistula and absent vagina are born with agenesis of the internal genitalia (uterus and fallopian tubes). In such cases the vagina is replaced with a piece of colon; this is done only for the patient to have sexual function. Twenty percent of the patients have a uterus and a blind ending of vagina, usually located very high in the pelvis (Fig. 15.6c). In that type of case, the lower vagina is replaced with a piece of colon with dual purpose (sexual and reproductive).
Some cases of vestibular fistula with absent vagina can be repaired without vaginal replacement, but rather pulling down their native vagina. That can only be done in cases with a large blind vagina.
Five percent suffered from some sort of septation disorder of the Müllerian structures. These included a vaginal septum, always associated with the presence of two hemicervices and two hemiuteri (Fig. 15.7). Three patients had a unilateral streak ovary; the rest had two normal ovaries. Two patients had a perineal lipoma, and one patient had a labial hemangioma.
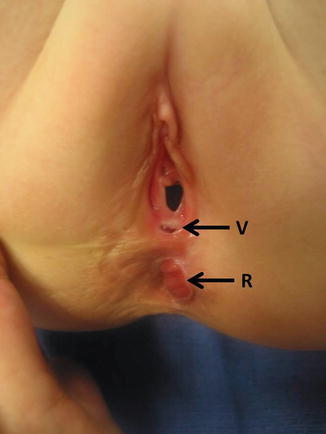
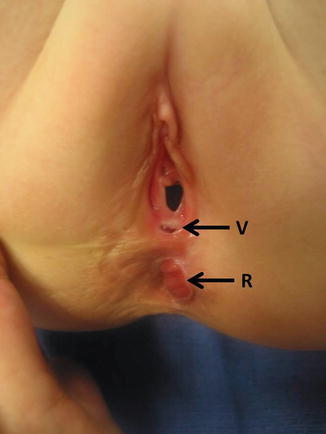
Fig. 15.7
Pocket of the original vestibular fistula in a patient previously operated with the erroneous diagnosis of a “rectovaginal fistula.” (R) rectum, V original fistula
We were able to see patients born with a vestibular fistula that came to us as adolescents; they had a repair in the past, but the surgeons missed the diagnosis of a vaginal septum. These vaginal septa can only be detected when the surgeon suspects their existence. Based on these findings, it is our routine and our recommendation to perform a vaginoscopy with a pediatric cystoscope in all patients with vestibular fistula. The presence of a vaginal septum may, in some cases, interfere with tampon placement and sexual intercourse when the patient grows up. But more important than that is the fact that the presence of a vaginal septum means, by definition, that the patient has two hemiuteri, representing a partial or total septation disorder. Hemiuteri have important gynecologic and obstetric implications. We know that patients with hemiuteri may have a higher degree of infertility, and those patients who become pregnant have a higher incidence of miscarriages and premature labor. Therefore, it is extremely important to make the diagnosis as early as possible in order to provide these patients with special gynecologic and obstetric care later in life.
It is our routine to do a vaginoscopy in every case of vestibular fistula. We perform that study with a baby cystoscope, during the same anesthesia given for the repair. Figure 15.8 shows the aspect of a normal infant cervix.


Fig. 15.8
Vestibular fistula with a vaginal septum. Arrow shows the fistula site
15.2.5 Gastrointestinal
Six percent of our patients with vestibular fistula had an associated esophageal atresia, one patient without a fistula, and all the others with a tracheoesophageal fistula; 1 % had a form of duodenal obstruction (atresia or stenosis).
15.2.6 Tethered Cord
Fifty-seven patients were evaluated with an ultrasound (first 3 months of life) or with an MRI, looking for spinal cord anomalies; twenty of them had tethered cord (35 %). These figures are higher than the average of all anorectal malformations, and we believe that this is explained by the fact that the incidence of presacral masses is also high in this malformation. Tethered cord is very common in cases with presacral mass.
15.2.7 Cardiovascular
Twenty-seven patients (9 %) had an atrial septal defect. Twenty-two (8 %) had a ventricular septum defect. Fourteen (5 %) had a patent ductus arteriosus, and four (1 %) suffered from tetralogy of Fallot. Most of these defects (approx. 80 %) did not require treatment, since the patients were hemodynamically stable.
15.3 Diagnosis
The diagnosis of vestibular fistula is a simple one. It only requires a meticulous inspection of the genitalia of the baby. Yet, amazingly, many patients are not diagnosed or are misdiagnosed as having “rectal vaginal fistula.” From our series of 1,123 female patients, we have only seen seven cases of documented real rectovaginal fistula. During the same period of time (over 30 years), we have operated on 290 cases of vestibular fistula. Fifteen of them come to our center with a previous diagnosis of “rectovaginal fistula.” Actually, they were born with a vestibular fistula as evidenced by the presence of a little pocket where the vestibular fistula used to be located (Fig. 15.9). Forty-five female patients also came to us after a failed attempted repair of a malformation diagnosed as “rectovaginal fistula.” A careful examination revealed that those patients actually had a persistent urogenital sinus, which means that they were actually born with a cloaca and the surgeons only repaired the rectal component of the malformation, because they were thinking that the patient only had a rectovaginal fistula (see Chap. 16, Sect. 16.1.4).


Fig. 15.9
Aspect of a normal cervix in a baby with a vestibular fistula
Prior to 1980, the literature [2, 6–13] reported an elevated number of cases of “rectovaginal fistula” in female patients. In contrast, those authors reported very few vestibular fistula cases and very rare cloaca cases. A few publications after 1980 persist reporting “rectovaginal fistula cases.” Interestingly, looking at the diagrams of most of those publications, they actually show vestibular fistulas, although they call them “vaginal fistula.” The term “vestibular fistula” has been used correctly by some authors with large experience in the management of these defects [14–21].
We believe that this is not a simple semantic problem, but rather has important clinical implications [22]. We have seen patients born with vestibular fistula that were previously misdiagnosed as “vaginal fistula” and underwent a type of repair designed to repair “high” malformations, namely, a contraindicated abdominoperineal (open or laparoscopic) procedure that resulted in fecal incontinence. We also have seen that at least 30 patients born with a cloaca received the wrong diagnosis of “rectovaginal fistula” and underwent a repair only of the rectal component of the malformation, leaving the patient with a urogenital sinus [22].
15.4 Treatment
15.4.1 Colostomy or No Colostomy
This is a frequently debated subject. Many surgeons claim that they routinely repair vestibular fistulas without a colostomy and they have “good results” [12, 23–27]. Many others prefer to open a colostomy in all cases with a vestibular fistula. In the meantime, we see many patients that underwent a repair of a vestibular fistula without a colostomy and suffered from serious complications, including dehiscence and retraction of the rectum as well as reopening of the fistula. However, this recurrent fistula is frequently an acquired rectovaginal fistula, due to the fact that during the attempted repair, the posterior wall of the vagina was damaged.
As discussed in the Chap. 5, we believe that the answer for this question of colostomy or no colostomy is different for every surgeon and his/her different surrounding circumstances. It very much depends on the experience of the surgeon, the clinical condition of the patient, and the infrastructure of the hospital where the patient is treated.
In general, at our institution, if a baby is born with a vestibular fistula, we operate on her within the first 5 days of life without a colostomy, provided the baby is in good clinical condition, is full term, and does not have severe associated defects.
Consider the case of a premature baby with a cardiac condition and vestibular fistula. Under those circumstances, dilatations of the fistula may prove to be useful for the patient to be able to pass stool, eat, and grow. That would allow the surgeon to postpone the decision of colostomy or primary repair. On the other hand, a full-term baby in good clinical condition without associated defects in an institution with a good infrastructure and a pediatric surgeon with experience in the management of this defect, the patient can be operated before starting her feedings, at a time when the patient is still passing meconium, because when it is done in that way, the patient actually does not need any kind of bowel preparation.
Most of our patients come to us after the newborn period and with a colostomy already opened at another institution, sometimes in another country. Many other patients come to us after several months of passing stool with difficulty through the non-operated vestibule, with severe constipation and megacolon. Those patients are also treated without a colostomy at our institution, but our routine includes the admission of the patient 1 or 2 days prior to the main operation, insertion of a nasogastric feeding tube, and administration of GoLYTELY 1 at a rate of 25 mL/kg/h until the colon is completely clean. The patient receives a PICC line and parenteral nutrition for a period of 7–10 days postoperatively.
When the patient has a colostomy, the operation can be done without following this routine, but rather irrigating only the distal stoma of the colostomy the day before surgery. In that case, the baby can eat the same day of the operation; she will stay for 48 h in the hospital receiving intravenous antibiotics. Our experience is that the pain that these patients experience postoperatively is rather minimal. We have operated on primarily without a colostomy in approximately 50 % of our cases.
We use a posterior sagittal approach to repair these malformations. Other approaches do exist, and the most traditional and popular was described by Dr. Potts and is called a fistula transplant [28–32]. Some surgeons describe an operation called “anterior sagittal approach” [33–37]. We found that the word “anterior” in those publications was actually not referring to the incision, but rather to the position of the patient; in other words, the patient is positioned in lithotomy position, rather than prone, but the incision is always posterior to the fistula, because there is no way to make an incision anterior to the fistula site. In other words, the so-called “anterior sagittal approach” is actually a posterior sagittal approach performed in lithotomy position.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








