Fig. 1
A 30-year-old patient, 22 weeks pregnant, with right lower quadrant pain, vomiting, and elevated white blood cell count due to appendicitis, as demonstrated on magnetic resonance imaging (MRI). a Axial T1-weighted gradient-recalled-echo (GRE) image through the lower abdomen shows an 11-mm appendix extending posteriorly from the cecum, with inflammatory changes surrounding the more distal appendix, including fascial thickening. b Axial T2-weighted GRE image at the same level demonstrates the same finding. The appendix was correctly identified as being perforated on the prospective interpretation of this MRI examination, as proven at subsequent emergency surgery
Acute Pain in an Abdominal Quadrant
The differential diagnosis in a patient with an acute abdomen is influenced greatly by the nature and location of the pain. Therefore, imaging strategies localized to each of the four abdominal quadrants is discussed first, followed by diffuse or localized pain to the flank or the epigastric region.
Right Upper Quadrant
Pain from gallstones, and particularly acute cholecystitis, are by far the most common disorders presenting with acute right upper quadrant pain. Other differential diagnostic considerations include hepatitis from a variety of etiologies, liver abscess, and, rarely, a ruptured liver mass (usually hepatocellular adenoma or carcinoma).
US is the imaging examination of choice for evaluating acute right upper quadrant pain. It is an accurate examination for diagnosing or excluding acute cholecystitis. Sonographic findings include gallstones, a sonographic Murphy’s sign, wall thickening ⩾3mm, and pericholecystic fluid/inflammatory changes. The more of these findings that are present, particularly gallstones combined with a sonographic Murphy’s sign, the more likely acute cholecystitis is present. Isolated gallbladder wall thickening may be due to a variety of etiologies in addition to acute cholecystitis.
Recent publications show that CT and MRI are relatively accurate imaging examinations for cholecystitis, although the findings may be more subtle compared with sonography, especially early on (Fig. 2a). In our experience, patients with nonspecific abdominal pain and the eventual diagnosis of cholecystitis may be sent for CT on a relatively frequent basis rather than for sonography. Radiologists need to be aware of the potential for establishing or suggesting this diagnosis based on the initial CT findings, which are very similar to those on sonography, although pericholecystic inflammatory changes may be more obvious on CT and MRI. If the CT findings suggest cholecystitis but are not definitive, US can be performed. CT is also an excellent imaging examination for demonstrating complications of cholecystitis, including perforation/ abscess formation, hemorrhage, gas (in diabetic patients with emphysematous cholecystitis), and wall gangrene (Fig. 2b). CT findings of a stone lodged in the gallbladder neck or cystic duct and areas of absent wall enhancement correlate with the need for an open rather than a laparoscopic cholecystectomy.
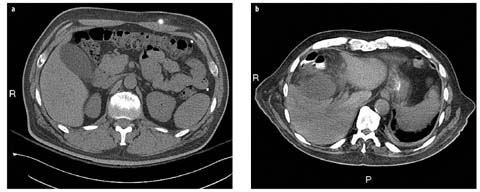
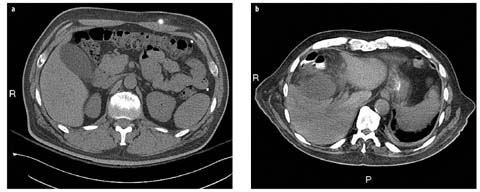
Fig. 2 a,b
a A 46-year-old man with acute right flank and right mid-abdominal pain, with suspected urolithiasis and previous gastric banding. Noncontrast computed tomography (CT) image shows a mildly distended gallbladder, with subtle wall thickening and inflammation adjacent to the gallbladder neck. CT correctly demonstrated acute cholecystitis, although subsequent ultrasound (US) findings (not shown) were more obvious and confirmatory. b A 76-year-old man with renal dysfunction, diabetes, and Escherichia coli bacteremia. Axial computed tomographic (CT) image, performed with orally administered contrast only, shows prominent focal inflammatory changes associated with a distended gallbladder, which proved to be due to gangrenous cholecystitis. There is also interposition of the hepatic flexure of the colon anterior to the liver, with associated liver remodeling. Inflammatory changes spread to the adjacent colon
US, CT, and MRI are all accurate imaging examinations for diagnosing (and following-up) liver abscesses (Fig. 3), which are usually pyogenic but which also may be amebic. US usually demonstrates a round or oval hypoechoic mass or masses, which may produce low-level echoes. Occasionally, a hepatic abscess may simulate a solid (or partially solid) hepatic mass on cross-sectional imaging examinations (especially with certain Klebsiella species). Pyogenic liver abscesses may be idiopathic or result from seeding from infection in the biliary tract, from the luminal gastrointestinal tract, or from the portal/ mesenteric venous system. An enhancing wall and a peripheral zone of edema are common on CT and MRI but are not universally present.
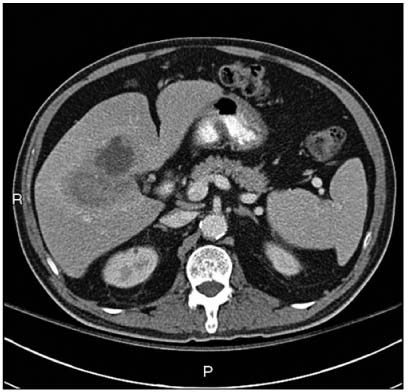
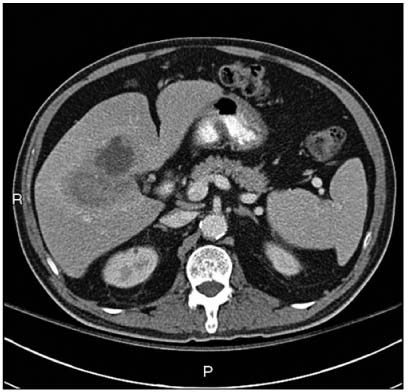
Fig. 3
A 73-year-old man with fever. Axial computed tomography (CT) image with contrast administered orally and intravenous (IV) demonstrates an abscess in the central liver. The posterior component is less li quified centrally than the anterior component and is associated with thrombosis of a portion of the right portal venous system
Spontaneous rupture of a hepatocellular carcinoma with associated hemoperitoneum is a frequent complication in countries with a high incidence of this type of tumor; however, it is highly uncommon in Western countries (>2% of cases). Hepatocellular carcinoma is usually vascular, and tumor necrosis with associated hepatic capsular rupture and rupture of vessels within the tumor is the presumed etiology. The differential diagnosis includes spontaneous hemorrhage within a hepatic adenoma or a hepatic metastasis. Patients present with acute pain and blood loss. Rapid diagnosis and therapy are essential. Transcatheter embolization is the treatment of choice.
Left Upper Quadrant
Although infrequent, acute left upper quadrant pain is most often caused by splenic infarction or abscess (e.g., secondary to bland or septic emboli to the spleen) (Fig. 4). It may also occur in the setting of acute gastric disorders, including gastritis and ulcer. Generally, CT is performed first, although US may occasionally be the first imaging examination. The diagnosis of gastric pathology is best established by endoscopy, although patients may present with left or right upper abdominal pain and other nonspecific signs and symptoms; CT may reveal the diagnosis when it is not clinically suspected. CT findings include focal or diffuse gastric wall thickening, increased mucosal enhancement, submucosal edema, and perigastric inflammatory changes. Focal ulceration with or without perforation also may be identified, which is generally of benign but occasionally of malignant etiology.
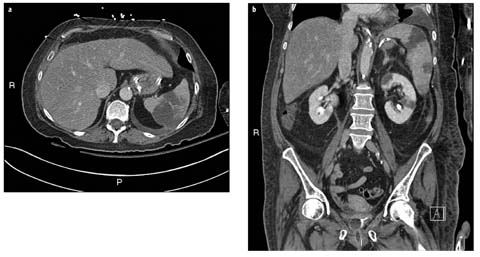
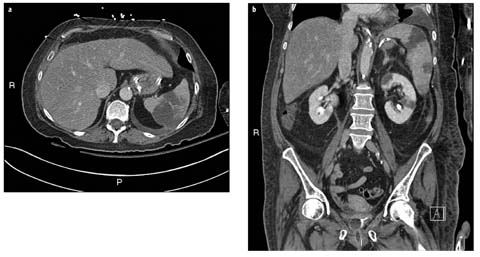
Fig. 4 a,b
A 65-year-old woman with fever and bacteremia and known endocarditis. a Axial computed tomography (CT) image with IV-administered contrast shows acute infarction in the spleen due to septic emboli. There is a small, reactive left pleural effusion. b Coronal CT reformation shows the extent of splenic infarction and bilateral acute renal infarcts due to septic emboli, left larger than right
Splenic infarction may be focal and less commonly global. Other etiologies of splenic infarction include marked splenomegaly with outgrowth of the splenic blood supply, and pancreatitis. Typical infarcts are wedge shaped and hypoattenuating on CT. Most splenic abscesses are secondary to hematogenous dissemination of infection and are seen primarily in immunocompromised individuals and IV drug abusers. On CT, splenic abscesses demonstrate low attenuation centrally with an enhancing rim and occasionally display central gas. Spontaneous splenic rupture can occur in patients with splenomegaly caused by hematologic malignancy or viral infection (e.g., mononucleosis).
Right Lower Quadrant
Appendicitis is the most frequent cause of acute right lower quadrant pain and the most commonly encountered diagnosis leading to surgery. Other disorders that can present with acute right lower quadrant pain include Crohn’s disease, right-sided colitis or diverticulitis, and pelvic inflammatory disease, ovarian cysts (and their complications, including rupture, hemorrhage, and torsion), and other obstetric and gynecologic conditions in women. Less common causes include omental infarction (which can also present with upper or mid right abdominal pain), epiploic appendagitis, and small-bowel diverticulitis (ileal or Meckel’s).
Preoperative cross-sectional imaging continues to play an important role in diagnosing or excluding appendicitis and in identifying complications or alternative diagnoses. At most centers, even when the clinical presentation is typical (in up to one-third of patients it is not), CT usually is obtained to confirm the diagnosis and serve as a surgical road map (Fig. 5). The most specific CT finding is a thick-walled, dilated, fluid-filled appendix (occasionally containing gas), which may have one or more liths. Contrast-enhanced CT often demonstrates stratification in which the individual layers of the appendiceal wall can be identified, with mucosal hyperenhancement and submucosal edema. As the disorder progresses, there is increasing inflammation of the adjacent fat. Findings indicative of perforation include periappendiceal abscess, extraluminal gas or lith(s), defects in the appendiceal wall, and associated SBO.


Fig. 5 a–c
Ultrasonography (US) of acute appendicitis in a 12-year-old girl. Oblique (a, b) and transverse (c) views show a swollen appendix (diameter 10 mm), with a target configuration
Opacification of the entire appendiceal lumen is a helpful finding to exclude appendicitis if contrast is administered orally; however, as noted, some institutions/practices have eliminated the routine use of orally-administered contrast for CT of the acute abdomen. Regardless of the specific CT protocol used, interpretation depends in part on the experience of the interpreting radiologist. In a minority of cases, particularly in early and subacute/chronic appendicitis, imaging findings can be subtle. It should be noted that an appendix >6 mm in transverse diameter can be normal on CT if other findings of appendicitis are absent. In evaluating suspected appendicitis in children (Fig. 6) and in selected nonpregnant women of childbearing age, US is considered the initial examination of choice, if available, although CT has a higher accuracy rate. Demonstration of a swollen, noncompressible appendix >7 mm in diameter, with a target configuration and with pain corresponding to the site of the appendix, are the primary US criteria. Appendicolith or liths may be identified.
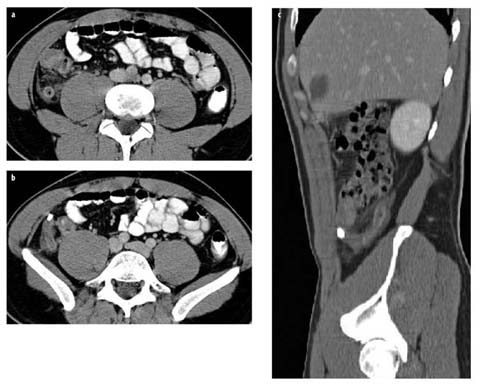
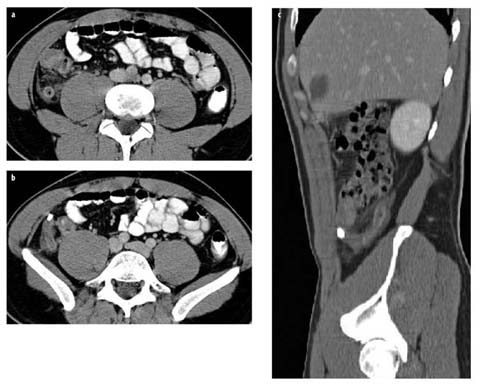
Fig. 6 a–c
Acute appendicitis. a, b Axial computed tomography (CT) images and c sagittal CT reformation demonstrate a dilated appendix in a retrocecal position, an appendicolith at the base of the appendix (c), and inflammatory changes of the mesenteric fat (a)
In pregnant women, appendicitis has a more variable presentation, and diagnosis is more challenging with all cross-sectional imaging modalities. US remains the initial imaging examination despite its poor sensitivity and specificity in this clinical setting. Noncontrast MRI is used increasingly in such patients after nondiagnostic US; it demonstrates high accuracy for the diagnosis and exclusion of appendicitis, and for the identification of alternative diagnoses. CT should be reserved as a third-line examination and used only if needed.
CT findings of right-sided diverticulitis are similar to those of the more common left-sided diverticulitis, including an inflamed diverticulum, adjacent diverticula, colonic wall thickening, and pericolonic inflammatory changes. Localized inflammation may be substantial. When considering a diagnosis of cecal diverticulitis, it is important to identify a normal appendix. Microperforation may occur, but more substantial complications, which are common in left-sided diverticulitis, such as abscess formation, fistula, and obstruction, are highly unusual in right-sided diverticulitis.
Crohn’s disease is often first evaluated with CT; however, because patients with known Crohn’s disease usually are young and require serial imaging, follow-up imaging with MR enterography is increasingly important to reduce radiation exposure. Cross-sectional imaging permits evaluating wall thickening and enhancement; changes of adjacent fat, vessels, and lymph nodes; and assessment of complications, including formation of abscesses, strictures, and fistulas.
Left Lower Quadrant
Diverticulitis of the sigmoid or descending colon is a common disorder in middle-aged and older patients but also can affect young individuals. CT is the examination of choice and is typically performed with IV-administered contrast with or without orally or rectally administered contrast. Other protocols include noncontrast CT. In uncomplicated disease, CT (or MR) findings are the same as with right colonic diverticulitis. Patients with redundancy of the sigmoid colon may present with midline or right lower quadrant pain. CT also demonstrates complications, including microperforation/extraluminal gas (Fig. 7), fistula/abscess formation, and unusual complications, such as venous thrombosis, liver abscess, urinary tract obstruction, and adnexal involvement. Recent data suggest that only selected patients identified with what is believed to be left colonic diverticulitis on CT require follow-up optical colonoscopy to exclude underlying carcinoma (i.e., those with atypical and/or complicated CT findings).
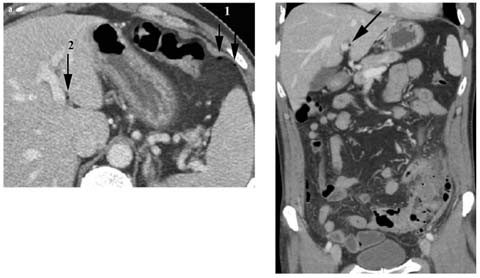
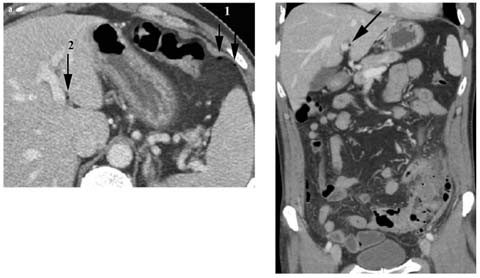
Fig. 7 a,b
Perforated sigmoid diverticulitis. a Axial computed tomography (CT) image demonstrates tiny bubbles of extraluminal gas within the left subphrenic space (arrows, 1) and hepatic pedicle (arrow, 2). b Coronal CT reformation shows thickened sigmoid colon, with associated diverticular disease, inflammation of the adjacent fat, and thickening of the root of the sigmoid mesocolon. Note the tiny bubble of extraluminal gas (arrow) within the hepatic pedicle
Other diagnostic considerations in patients presenting with left lower quadrant pain include colitis of a variety of etiologies, including infection (especially from Clostridium difficile in the correct clinical setting) (Fig. 8) and ischemia; functional colonic disorders (especially constipation, and also obstruction from a variety of other etiologies); urinary tract infection; and gynecologic disease.


Fig. 8 a,b
A 73-year-old woman with abdominal pain. The patient had been on antibiotics orally for 10 days for an upper respiratory tract infection. Noncontrast coronal computed tomography (CT) reformations demonstrate moderate to marked thickening of the entire colonic wall, as well as some associated ascites, which proved to be due to Clostridium difficile
Epiploic appendagitis is a relatively common, self-limiting condition in which an appendage of fat along the external aspect of the colon — left side much more common than right — undergoes torsion, with subsequent venous thrombosis. CT findings include a swollen, ovoid, 1.5− to 3.5− cm fat-containing focus with peripheral thickening and associated inflammation. The adjacent colon is usually normal or nearly normal.
Gynecologic Disorders
US is the primary imaging examination in women with suspected gynecologic pathology. Human chorionic gonadotropin (HCG) level should be checked emergently in all patients with acute, nontraumatic abdominal and pelvic pain to exclude ectopic or incidental pregnancy. MRI is used increasingly as a problem-solving examination after pelvic US and for follow-up. However, because women with acute gynecologic disorders often present with nonspecific signs and symptoms, CT is ordered frequently to evaluate their abdominal pain. Therefore, radiologists interpreting CT of the acute abdomen and pelvis must be familiar with the findings of a wide variety of gynecologic disorders that may present emergently. CT can also be used selectively as a problem-solving tool in patients with known or suspected gynecologic disorders.
Ovarian Torsion
If ovarian torsion is suspected prospectively, pelvic US is performed emergently. However, CT and MRI findings are also characteristic, are similar to US findings, and may complement US if the sonographic examination is initially equivocal. Radiologists must maintain a high index of suspicion for ovarian torsion, as the clinical presentation is variable; the possibility of torsion should be suspected if imaging findings suggest or strongly indicate this diagnosis. Cross-sectional imaging findings include an enlarged, edematous ovary with or without an associated cyst or mass (most commonly a teratoma), deviation of adnexal structures to the contralateral side, deviation of the uterus to the side of torsion, twisting of the adnexal/vascular structures, decreased ovarian vascularity, multiple peripheral ovarian follicles, inflammation of the adjacent fat, and ascites.
Ovarian Cysts
Ovarian cysts are very common and may be complicated by hemorrhage. Associated hemoperitoneum, if present, is usually self-limited. The differential diagnosis of a hemorrhagic ovarian cyst is endometrioma. It is particularly critical to check the HCG level in a woman with otherwise unexplained hemoperitoneum to ensure that a ruptured ectopic pregnancy is not present.
Pelvic Inflammatory Disease
Pelvic inflammatory disease (PID) is also common and has a broad spectrum of findings and presentations. If PID is known or suspected, US is done first. However, CT may initially be performed if the diagnosis is not known and the clinical presentation is nonspecific (Fig. 9). The most common causative organisms are Gonococcus and Chlamydia. Because PID most commonly results from ascending infection, it usually involves both adnexa. In the earlier stages of PID, there may be no or only subtle findings on cross-sectional imaging. There may be swelling of the ovaries and/or fallopian tubes, abnormal enhancement of the adnexal structures, and mild adjacent edema. In later stages, tubo-ovarian abscesses and/or hydrosalpinx/pyosalpinx may be identified, and adjacent organs may also be involved in complicated cases. Imaging findings include thickening and increased enhancement of the dilated, tortuous fallopian tube(s), a septated mass in the ovary or ovaries, and adjacent edema. Other presentations of PID include endometritis, cervicitis, and Fitz-Hugh-Curtis syndrome in which perihepatitis leads to increased enhancement of the liver edge.


Fig. 9
A 32-year-old woman with lower abdominal pain and previously unknown pelvic inflammatory disease. Axial computed tomography (CT) image with contrast orally and IV reveals dilated, tortuous, bilateral, fluid-filled fallopian tubes containing a small amount of ascites
Other Acute Gynecologic Disorders
Other acute gynecologic disorders that can be identified on cross-sectional imaging examinations include less common forms of PID (e.g., actinomycosis), endometritis, ovarian vein thrombosis (typically following cesarean section), uterine rupture following delivery, gynecologic tumors, and complicated uterine leiomyomas (e.g., hemorrhage/ degeneration, torsion, and acute prolapse).
Acute Abdomen with Diffuse Pain
Any disorder that involves a large portion of the gastro-intestinal tract or irritates the peritoneum can cause diffuse abdominal pain. The most common disorder is gastroenteritis, in which CT findings often are normal or may show mild bowel wall thickening and increased intraluminal fluid. Patients with colitis have varying degrees of colonic wall thickening/edema, with inflammation of the adjacent fat. Other important disorders that present with diffuse abdominal pain include bowel obstruction and ischemia.
Bowel Obstruction
Bowel obstruction is a very frequent cause of abdominal pain in the emergency setting. Small-bowel obstruction (SBO) is usually due to adhesions — more commonly in patients with previous surgery but occasionally seen in patients without prior surgery and less commonly due to hernias (external or internal), obstructing tumors, perforated appendicitis, inflammatory bowel disease, and complicated diverticulitis. Less common etiologies include gallstone ileus, intussusception, intramural small-bowel hematoma, and radiation enteritis. Large-bowel obstruction (LBO) is most commonly due to colorectal carcinoma, but diverticulitis and sigmoid or cecal volvulus are also important etiologies.
Bowel obstruction is usually diagnosed on clinical grounds and then confirmed and further evaluated as needed by imaging, typically with CT, with or without initial plain radiographs. However, frequently, the diagnosis of bowel obstruction is not clear or clinically recognized, and obstruction is established on the basis of imaging. CT reveals the presence or absence of obstruction, as well as site, level, and cause of obstruction, and permits identification of associated ischemia (Fig. 10). In SBO, the radiologist should search for the transition zone between the dilated proximal small bowel and the collapsed distal small bowel. There is often a segment of small bowel containing feces-like material just proximal to the transition zone. Review of multiplanar CT reformations is important to help identify the site of transition, which may be difficult to find conclusively on review of transaxial images alone. In a minority of cases, CT reveals a closed-loop SBO, which usually requires emergency surgery. In this situation, two points along the course of the small bowel are obstructed at a single site, usually associated with an adhesive band or hernia. Less commonly, closed-loop SBO may be due to volvulus of the small bowel.
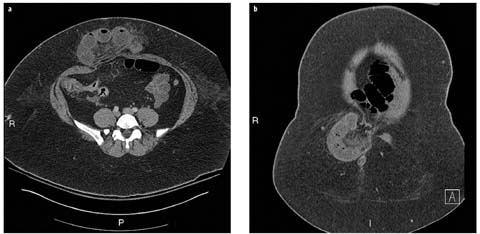
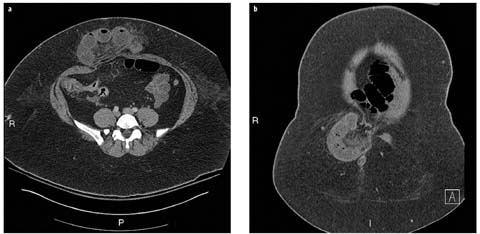
Fig. 10 a,b
A 41-year-old woman with acute abdominal pain and gastric bypass surgery. a Axial computed tomography (CT) image with IV contrast and b coronal reformation show an anterior abdominal wall hernia containing dilated loops of small bowel, with associated mesenteric edema and thickening of the small bowel loops, representing obstruction with associated strangulation. The patient required emergency surgery
SBO needs to be differentiated from LBO and from ileus and motility disorders involving the small and/or large bowel. Ileus of the small and/or large bowel is common after abdominal surgery and has multiple etiologies. In LBO, CT demonstrates distension of the large bowel to the point of obstruction, with collapse of the distal large bowel. The small bowel may demonstrate varying degrees of associated dilation. Colonic volvulus should be readily identified (Fig. 11), particularly on review of multiplanar reformations. A variety of CT signs are reported, and volvulus may be complicated by ischemia and subsequent perforation. Marked dilation of most or all of the colon may be seen in toxic megacolon from a variety of etiologies, as well as in pseudo-obstruction, the latter of which can also lead to subsequent volvulus. A very common cause of abdominal pain in emergency department patients is constipation, which may be of varying degrees of severity, usually without an associated focal obstructing lesion. Other motility disorders, such as scleroderma and administration of anticholinergic or opioid medications, also may lead to the need for CT in patients presenting with acute abdominal pain.
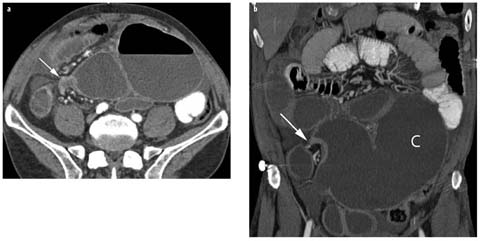
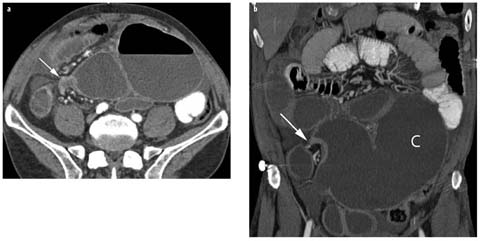
Fig. 11 a, b
Cecal volvulus. a Transverse computed tomography (CT) image and b coronal CT reformation demonstrate a markedly dilated cecum (C) located in the midline and left lower abdomen and upper pelvis. The arrows point to the area of colonic twisting. Note the dilated small-bowel loops due to the proximal colonic obstruction
Bowel Ischemia
Bowel ischemia has a variety of etiologies, including arterial thrombosis or embolism, venous thrombosis, hypo perfusion, and vasculitis. Occlusive disease involves the mesenteric arteries, most commonly the superior mesenteric artery, whereas bowel ischemia secondary to venous thrombosis is much less common. The only direct CT (or MRI) sign of vascular impairment of the bowel is diminished wall enhancement, whereas increased bowel wall enhancement is seen in a wide variety of disorders, including in a subset of patients with bowel ischemia due to reactive hyperemia, loss of autoregulation, or compromised venous outflow. Other cross-sectional imaging findings include direct visualization of embolus or thrombus in the mesenteric arterial circulation or thrombus in the mesenteric venous circulation. Bowel distension and wall edema are nonspecific findings that may be identified in ischemia but also may be present in various infectious, inflammatory, or immunologic conditions and in primary bowel obstruction. Nonocclusive acute mesenteric ischemia is usually due to hypoperfusion secondary to severe cardiac disease; generalized decreased caliber of the arterial circulation is present.
Bowel ischemia may also be secondary to bowel obstruction, particularly a closed-loop SBO, but may also be identified secondary to large-bowel obstruction or volvulus. Focal or regional bowel wall thickening due to edema and hemorrhage may be seen on CT, with decreased bowel wall enhancement and edema adjacent to the affected bowel. With frank infarction, pneumatosis, portal/mesenteric venous gas, peritonitis/ascites, and free gas can be found.
Bowel Perforation
Gastrointestinal perforation usually causes localized pain initially, which becomes more diffuse if peritonitis develops. Perforation due to peptic ulcer disease or a necrotic neoplasm have become less frequent due to earlier diagnosis and improved therapy (Fig. 12a). However, the incidence of perforation resulting from endoscopic procedures has increased. Perforation of the small bowel is relatively uncommon but may be secondary to a foreign body, diverticulitis, or trauma, among other possibilities. Perforation of the colon is more frequent and can occur when the colon becomes markedly dilated proximal to an obstructing lesion (e.g., tumor, volvulus) or when the colonic wall is friable (e.g., diverticulitis, ischemia, ulcerative colitis, tumor) (Fig. 12b–c).










