Chapter 84A Radioembolization for liver tumors
Overview
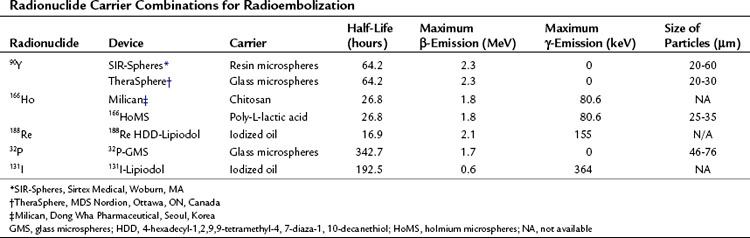
Interventional oncology is a field that is establishing its role in the management of liver tumors. The techniques used in this field are targeted to the tumors to allow delivery of toxic chemotherapeutic, radiotherapeutic, and thermal doses with minimal toxicity to normal structures; this minimizes the systemic toxicity associated with these therapeutic options and allows delivery of doses to the tumor that would not be possible using systemic delivery methods. In this chapter, the general concepts associated with radioembolization and its specific use in different primary and secondary malignancies of the liver will be discussed (Table 84A.1)
Vascular Anatomy of the Liver and Its Tumors (See Chapter 1B)
Hepatic Artery
Unlike the normal hepatic parenchyma, liver tumors are supplied primarily by hepatic arterial blood and are hypervascular structures compared with the surrounding uninvolved parenchyma (see Chapter 86). Hepatic tumors may parasitize arterial blood flow from the arteries that supply segments adjacent to the segment the tumor is in and those of surrounding organs, such as the stomach. This relative arterial hypervascularity of the tumors with respect to the normal parenchyma has been the basic principle behind transarterial therapies for targeting liver tumors.
History of Radioembolization
External Radiation (See Chapter 84B)
The use of external radiation for liver tumors has traditionally held limited value because of the sensitivity of the normal hepatic parenchyma to the radiation dose (Ingold et al, 1965; Geschwind et al, 2004). A dose greater than 35 Gy has led to the development of a radiation-induced liver disease (RILD); a clinical syndrome of ascites, anicteric hepatomegaly, and elevation of liver enzymes. Conformal-beam therapy, which uses a three-dimensional approach rather than broad axial plane techniques, has been shown to minimize the toxicity to normal hepatic parenchyma (Dawson et al, 1999). However, even when using conformal-beam therapy, the radiation delivered to normal hepatic parenchyma limits the maximum dose that can be delivered to the tumor without compromising safety.
External-beam radiation had limitations in treating liver tumors in specific locations; this includes tumors near the dome of the liver, which carry the risk of exposing the lungs to radiation and increasing the risk of radiation pneumonitis, and tumors in the caudate lobe in close proximity to the porta hepatis, where risk of damage to the major biliary and vascular structures is a consideration. Dose fractionation, dose delivery to the tumor in fractions, is beneficial in targeting radiosensitive and radioresistant malignant cells at different sessions, but multiple treatments are required. The normal tissue complications probability (NTCP) is an important parameter when calculating radiation dose delivery (Dawson et al, 2002), but its use has been challenged (Langer et al, 1998). Respiratory movement must be considered to minimize the incidence of normal tissue complications, although recent advances in the technology of external-beam radiation have been shown to increase safety and efficacy of this technique, such as stereotactic body radiotherapy, proton radiotherapy, and carbon ion radiotherapy; these are establishing the role of external-beam radiotherapy in the management of liver tumors (Dawson & Guha, 2008; Fukumitsu et al, 2009; Nomiya et al, 2008).
Radioembolization
Radioembolization was first studied by Nolan and Grady (1969) using yttrium-90 oxide (90Y2O3) contained in a metal particle 50 to 100 µm in size. Their study consisted of a small number of patients but showed a favorable response, observed by the reduction in size of palpable masses. The next 90Y study was published in 1982 by Mantravadi and colleagues and studied the effect and distribution of 90Y after whole-liver delivery via the hepatic artery; the authors concluded that patients with hypervascular tumors are much more likely to benefit from this treatment. A dose-escalation study on animals was performed, which formed the basis of the Phase I dose-escalation evaluations in humans (Wollner et al, 1987). Shepherd and colleagues (1992) conducted a Phase I dose-escalation study using 90Y microspheres in 10 patients. Extrahepatic shunting was assessed using technetium-99m–labeled macroaggregated albumin (99mTc-MAA). In contrast to earlier studies, none of the patients in this study experienced hematologic toxicity, a fact that emphasizes the value of assessing angiographic findings and extrahepatic shunting before treatment (Shepherd et al, 1992). The technical aspects of dosimetry, radioassays, safety, and efficacy were discussed by many studies that followed (Andrews et al, 1994; Yan et al, 1993). Lau and colleagues (1994) showed that tumor response was proportional to the dose delivered, with improved survival in patients receiving more than 120 Gy. Recent data on the safety and efficacy of this treatment are discussed below.
90YTTRIUM Microspheres
Pretreatment Evaluation
Pretreatment Angiography and Coil Embolization
Radioembolization requires pretreatment diagnostic mesenteric angiography. The aortogram, superior mesenteric angiogram, and celiac trunk angiogram allow the interventional radiologist an opportunity to study the vascular anatomy of the liver and its surrounding structures in detail. The patency of the portal vein and the presence of arterioportal shunting are assessed. The inadvertent spread of the microspheres is prevented by a meticulous study of the vascular anatomy of the liver and collateral nontarget flow (Covey et al, 2002). Coil embolization of nontarget vessels may be necessary to decrease the unintended deposition of microspheres. Some examples of vessels that may need to be embolized are inferior esophageal, left inferior phrenic, accessory left gastric, supraduodenal, and retroduodenal arteries. The minimal incidence of complications following coil embolization and the grave clinical consequences associated with the inadvertent deposition of microspheres in the stomach, duodenum, or pancreas favor prophylactic coil embolization before radioembolization in select cases.
Available Devices
TheraSphere
SIR-Spheres
Dose Calculation for SIR-Spheres
Three methods for dosimetry of SIR-Spheres are recommended by the manufacturers. The partition method is seldom used, as it is applicable only in special circumstances. The empiric method is outlined in Table 84A.2.
Table 84A.2 Empiric Method for Dose in SIR-Spheres*
| Tumor Involvement of Liver (%) | Dose (Whole Liver) |
|---|---|
| ≤25 | 2 GBq |
| 25-50 | 2.5 GBq |
| >50 | 3 GBq |
New Concepts
Radiation Segmentectomy
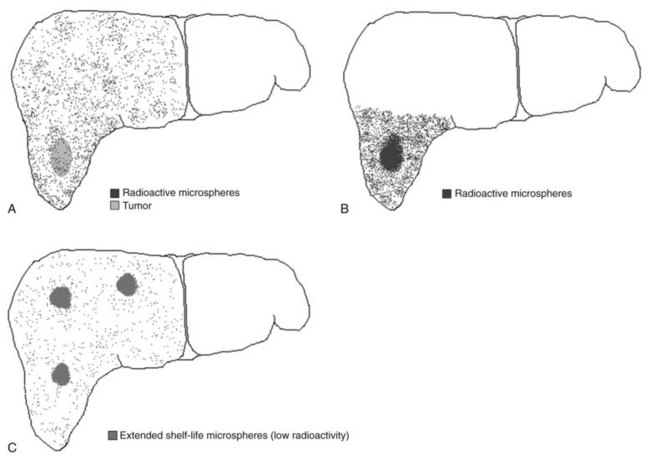
Recently, the concept of radiation segmentectomy has been discussed. This is schematically shown in Figure 84A.1B. The current dosimetry models assume lobar infusion; however, if the tumor is localized to two or fewer liver segments, the interventional radiologist can infuse the dose at the segmental level. This maximizes the dose delivery to the tumor and minimizes delivery of radioactive microspheres to the normal parenchyma (Riaz et al, 2010), an approach that has proven to be a safe and effective method of treatment delivery.
Extended Shelf Life Microspheres
Lewandowski and colleagues (2009b) recently published a report on the concept of extended shelf life microspheres, which can be used for large or multifocal tumors. As stated above, the difference in vials of different activities is the number of microspheres. If the vials of high activities (more microspheres) are allowed to stay on the shelf longer, the activity per microsphere will decrease. This allows the delivery of a higher number of microspheres to larger volumes of the liver with minimal radiotoxicity to the normal parenchyma (Lewandowski et al, 2009b).
Radiation Lobectomy
An animal study concluded that portal fibrosis was seen after the use of radioactive microspheres (Wollner et al, 1988). Gaba and colleagues (2009) recently published a comprehensive analysis on the concept of radiation lobectomy, whereby infusion at the lobar level was used to treat the tumors. Because of fibrosis of the normal parenchyma, decreases in volumes of the treated lobe were seen. Furthermore, compensatory increases in the volumes of the untreated lobes were also observed.
New Concepts
Blood Flow Patterns for Dose Calculation
Kennedy and colleagues (2010) have recently published their analysis on computer modeling of 90Y resin microsphere transport in the hepatic arterial tree. They conclude that computer simulations of both blood flow patterns and microsphere dynamics have the potential to provide insight on methods to optimize microsphere implantation into hepatic tumors while sparing normal tissue.
Transcatheter 90Y Radioembolization
Radioembolization is a transcatheter therapy performed by interventional radiologists. The tumor is approached using its arterial supply, and the vial is injected into the vessel feeding the tumor. The distribution of the tumor is the factor that allows the treatment to be selective, allowing delivery to one lobe, or superselective, allowing delivery to one segment. The apparatus for the administration of 90Y is designed to minimize the radiation exposure to those involved in the procedure, but a physicist should be present throughout the case to ensure that proper protocols are followed to minimize accidental radiation exposure. The procedure is performed on an outpatient basis, and the patient is discharged on the same day (Salem et al, 2002).