Chapter 26 Quality of life and hepatopancreatobiliary tumors
Quality of Life
Quality of life (QoL) is a clinically and biologically meaningful outcome for the oncologic patient. Historically, surgical, procedural, and interventional outcomes have been measured in clinical and objective terms using end points such as morbidity, mortality, and disease-free survival. In the 1990s, there was increased recognition of the need to evaluate the patient’s subjective experiences, how they felt and functioned. Measurement of a patient’s QoL throughout the clinical course should be standard practice. A surgeon often manages the care of a hepatopancreatobiliary cancer patient beyond the surgical procedure alone. Management includes orchestrating diagnostic tests, biliary interventions, and percutaneous ablative therapies. For any of these procedures, the goal of the physician is to minimize the impact on a patient’s function and to improve overall QoL (Langenhoff et al, 2001; Miner et al, 2002; Blazeby & Vickery, 2001; Sajid et al, 2008; Pallis & Mouzas, 2004; Sun et al, 2008).
Surgical resection of malignant tumors of the liver, bile ducts, gallbladder, and pancreas is performed for both curative and palliative reasons. Hepatopancreatobiliary surgical outcomes have continued to improve, because advancements in presurgical imaging and surgical techniques have resulted in better patient outcomes, fewer complications, and higher survival rates. After recovery from surgery, while a patient remains disease free, QoL is usually excellent. For those patients who are not candidates for a curative resection, palliation is the major treatment goal (Sun et al, 2008; Abraham et al, 2002; Singhal et al, 2005). Indications for palliative surgical resection include locoregional disease control and surgical bypass to relieve biliary or gastrointestinal obstruction (Nakakura & Warren, 2007; Koninger et al, 2007). Resolution of symptoms such as pruritus, anorexia, fatigue, and pain and improvement of QoL are the major treatment goals.
Definition of Quality of Life
In 1947, the World Health Organization (WHO) broadened the definition of health to include not only the absence of disease but also “the complete physical, mental, and social well-being of a person” (WHO, 1947). Karnofsky and Burchenal (1949) subsequently outlined basic criteria for evaluation of new chemotherapeutic agents, describing a simple scale to measure the effect of nitrogen mustard on patients with lung cancer. In the years following, numerous anticancer therapies emerged that increased survival, but toxicities were significant. Izsak and Medalie (1971) sought to identify the “costs of survival” among cancer patients. Noting that a growing number of patients with cancer were surviving longer, they began looking at the lives of the survivors from multiple angles, namely the psychological, behavioral, and environmental aspects. This new insight into patient health care caused a dramatic increase in interest in the new field of QoL research (Aaronson, 1988). One event that placed QoL end points in the spotlight was the controversial approval of gemcitabine for the treatment of pancreatic cancer on the basis of a beneficial clinical response. The “surrogate end point” of clinical benefit was likened to improvement in QoL based on the parameters of pain intensity, analgesic consumption, performance status, and weight gain (Burris et al, 1997). The concept of clinical benefit has increased dialogue about pancreatic cancer and QoL and undoubtedly has raised awareness of the importance of QoL assessment in palliative care settings.
In an effort to better describe clinical benefit, the term health-related quality of life emerged and has come to include the aspects of QoL that are most influenced by health and health care interventions (Kassa & Loge, 2002). The terms quality of life and health-related quality of life are often used interchangeably, but no single definition of either exists. There is consensus, however, that QoL is multidimensional and at a minimum encompasses physical symptoms, treatments, functional ability, family factors, emotional well-being, intimacy, and social aspects (Cella, 1998).
The broad overuse of the term quality of life has led to the misleading notion that measurements of performance status (e.g., Karnofsky and Eastern Cooperative Oncology Group, 1949), clinical indicators (e.g., bilirubin level), or symptom checklists adequately reflect QoL (Blazeby & Vickery, 2001). Other clinical factors—including laboratory values, postoperative complications, and time spent in the hospital—also have been translated into QoL results. Although these assessments have value in clinical care and research, care must be taken not to mistake or substitute them for proper QoL measurement.
Applications of Quality of Life Assessments in Surgery
In the past, informal feedback from patients regarding symptoms and functional status combined with the clinician’s objective assessment was considered sufficient for making judgments about patients’ QoL. Over the past few decades, a demand for more information about the broader effects of treatment and illness has required more formal definitions and evaluations of QoL (Blazeby & Vickery, 2001; Gouma et al, 1999; Barbarisi et al, 2001). In addition to defining the patient’s physical, psychological, and functional problems, QoL assessments also evaluate surgical outcomes, compare treatment options, aid preoperative selection of patients, predict prognosis, and monitor quality of care. In the case of neurosurgical measurements of QoL, the standard remains the Karnofsky Performance Status (KPS) set by Karnofsky and Burchenal (1949), which only addresses three variables of QoL: 1) work, 2) activity, and 3) self-care (Meyers & Weitzner, 1995).
Quality of Life as an Outcome
Outcomes research is a new and interesting field in clinical research and in daily clinical practice. In 1996, the American Society of Clinical Oncology published a special article to clarify effectiveness of cancer treatments (ASCO, 1996). Outcomes were divided into cancer outcomes (response rate) and patient outcomes (survival and QoL). As a surgical outcome, QoL has become an issue of increasing importance. The American College of Surgeons has dedicated a section of its Surgical Forum to QoL and outcome studies since 1996 (Tassinari et al, 2003; Velanovich, 2001). More holistic patient outcomes can be given priority over cancer outcomes in several situations. Examples of surgical trials in which consideration should be given to QoL data are 1) adjuvant trials in which a moderate risk of disease recurrence is present; 2) trials in which survival is not expected to differ between treatment arms, but QoL might be affected; 3) trials in which the primary intent is palliative; and 4) equivalency trials in which lesser surgical procedures are done with the expectation that survival and tumor control will be equal (Whalen & Ferrans, 2001).
Psychological Screening
For many patients with newly diagnosed cancer, the psychological trauma can be quite intense. This is particularly true for patients with hepatopancreatobiliary cancer, most of whom face an uncertain future, with much of their remaining time consumed by oncologic treatment. The psychological impact of receiving such a diagnosis and living with the disease is profound. Depression and anxiety have been reported in 50% of patients with pancreatic cancer before their diagnosis, and several studies have suggested hormonal and neuropsychiatric links to explain this phenomenon (Holland et al, 1986; Passik & Breitbart, 1996; Passik & Roth, 1999). Attention to the emotional sequelae of hepatopancreatobiliary cancer may improve QoL and treatment adherence significantly. QoL questionnaires and/or psychological questionnaires may be used early in the diagnosis to identify problems that may not otherwise be detected during routine evaluation. Linden and colleagues (2005) found the Psychological Screen for Cancer to be an important tool in screening and for “following changes in patient distress throughout the cancer care trajectory.” Early identification of depression or anxiety allows for prompt evaluation by a mental health professional. Subsequent intervention with psychotherapy and/or medication may result in better psychological outcome for many patients.
Prognostic Indicators
QoL data have been shown to have prognostic value in several chemotherapeutic trials in patients with advanced metastatic colorectal cancer. Earlam and colleagues (1996) reported physical symptom scores were better predictors of survival than tumor size. In three large studies, QoL scores were independent predictors of survival; QoL was a stronger predictor of survival than clinician-rated performance status in two of these studies (Earlam et al, 1996; Schoffski et al, 1996; Maisey et al, 2001). One author concluded that QoL measurement may help stratify patients in clinical trials and may facilitate comparisons between studies (Blazeby & Vickery, 2001; Conroy & Blazeby, 2003). Pretreatment QoL was found by de Graeff and others (2001) to be a strong predictive indicator in the assessment of cancer survival in which performance status, physical functioning, and well-being were the QoL variables. For many patients with primary liver cancer or metastatic neuroendocrine cancer in the liver, treatment is often palliative and multimodal in nature, consisting of surgical, hormonal, ablative, and chemotherapeutic approaches. QoL assessment as a prognostic indicator and stratification tool may be useful for treatment algorithms and may help patients with poor performance status avoid futile treatments.
Physician-Patient Communication and Decision Making
The surgical oncologist is responsible for explaining surgical and ablative treatment options and for discussing treatment side effects, potential for cure, and impact of treatment on QoL. Physicians should have open discussions with patients as they advise them in these important treatment decisions. The physician opens the door for better communication by first trying to understand the value each patient places on issues such as survival, toxicity, disease-free interval, and impact on functional status; by matching treatment options to the patient’s value system, the physician can become more effective. Research has shown that patients differ greatly in how they view risk/benefit ratios. A study evaluating treatment options for elderly patients found that meetings with a facilitator along with written information allowed the patient and the family to make decisions better suited to their QoL needs (Matulonis, 2004). Knowledge of and effective communication of QoL results may lead to better informed, shared decision making and ultimately may improve the physician–patient relationship and the outcome (D’Angelica et al, 1998).
Quality of Life After hepatopancreatobiliary Surgery
Over the past 10 years, hepatopancreatobiliary operations have moved from high morbidity and high mortality procedures to procedures that are safe and effective in an experienced surgeon’s hands. When procedures are performed with the intent to cure, patients are usually accepting of a short-term decline in QoL as a part of recovery from surgery or as a surgical or procedural complication (Perez et al, 1997). When consenting for a procedure, patients usually assume the risks of the surgery willingly as the price of a cure. In this setting, assessment of QoL improves understanding of the impact of a surgery. On the other hand, for both procedural and surgical palliative interventions, patients are less forgiving of postprocedure complications that cause a decline in QoL in the face of an imminently diminishing life span. Therefore QoL becomes an important outcome to include when evaluating a palliative intervention.
Miner and others (2002) offer insight into outcomes after palliative surgeries for advanced malignancy. Their study, limited by a small number of subjects (n = 36) and early mortality (median survival, 108 days), found that 54% of the patients who underwent palliative operations for unresectable disease experienced no clinical improvement after surgery, and these patients died significantly sooner than those who experienced a benefit. For those who did experience an improvement in QoL, duration of improvement was a median of 3.4 months. The surgeon’s preprocedure predictions regarding ability to relieve symptoms were correct 78% of the time for those with positive outcomes, while he or she only mistakenly thought they could ameliorate 1 (7%) of the 14 patients who did not improve. The reasons for the surgeon proceeding with the surgery in the belief of a poor clinical outcome were not discussed. Prior to surgery, 26% of patients expressed fear that they did not expect to survive the surgery; patients also reported a strong relationship with their surgeon before the surgery, and this did not change significantly afterward.
Unfortunately, the study found that 46% of patients undergoing palliative surgery expressed hope that their physician would find no evidence of disease at the time of surgery (Miner et al, 2002). This belief cannot simply be attributed to optimism, hope, or a delusional process; however, it is likely that these patients harbored misconceptions regarding the procedure that were not corrected during the consenting process. It is critical that patients understand that a palliative procedure is being done only to improve QoL; a cure cannot be achieved, and there will still be evidence of disease. Furthermore, patients should have a realistic expectation as to whether the goal of palliation is achievable. Surgeons should trust their clinical judgment regarding their ability to bring about a favorable clinical outcome as well as the potential for futility. These opinions should be discussed with patients, and such discussions are likely to be in depth and difficult; but the end goal of more realistic patient expectations should not be undervalued, and this is an important topic in palliative medicine that should be further explored.
Measurement and Interpretation of Quality of Life End Points
It has been established that QoL is an important outcome that should be incorporated into surgical oncology, but the problem remains: How should it be measured? Specifically, what should be measured? First, the concept needs to be clearly defined, because a great deal of variability surrounds the way QoL might be measured in a clinical trial. In a review of QoL studies in six major surgical journals, Velanovich (2001) found that many studies made errors in conceptually defining QoL and in choosing QoL questionnaires. Passik and Kirsch (2000) suggested a “levels of evidence” approach to understanding QoL end points in clinical trials. Such an approach is based on the type and sophistication of the questionnaire chosen for the trial and the conclusions one can make from the resulting data. This approach may be helpful in interpreting QoL conclusions made by authors and in aiding investigators in trial design (Table 26.1). The European Organization for the Research and Treatment of Cancer (EORTC) has placed the evaluation of QoL on questionnaires such as the QLQ-C30, SF-36, and the Rotterdam Symptom Checklist and on modules specific to the disease and treatment (Giannakopoulos et al, 2005). Better understanding of the QoL concept would help the investigator design a study, and it would help to make the published results more meaningful (Koller & Lorenz, 2002; Sprangers, 2002).
Table 26.1 Levels of Evidence for the Determination of QoL in Clinical Trials
| Level of Evidence | Approach Taken | Explanation |
|---|---|---|
| Low | Single items | This approach includes the use of face-valid items only. Typically, these are designed by researchers for a particular study and have not been piloted or validated by any formal psychometric means. |
| Middle (A) | Conversion of existing tools | This approach is highlighted by the adaptation of tools from traditional psychology and psychiatry to oncology and assuming that they will be valid and reliable indicators for cancer patients (e.g., Ways of Coping population questionnaire). |
| Middle (B) | Assessment of a singular domain of QoL | The middle level of evidence also may focus on measuring a single domain of QoL. Typically, the focus is placed on physical well-being and measurement of side effects of treatment (e.g., toxicity ratings of treatments). |
| High | Multidimensional assessment of QoL | The highest level of evidence requires a multidimensional approach. This should cover the domains of physical, psychological, social, and functional well-being (e.g., FACT, FLIC, CARES). |
QoL, Quality of life; FACT, Functional Assessment of Cancer Therapy; FLIC, Functional Living Index-Cancer; CARES, Cancer Rehabilitation Evaluation System
From Passik S, Kirsch K, 2000: The importance of quality-of-life endpoints in clinical trials to the practicing oncologist. Hematol Oncol Clin North Am 14:877-886.
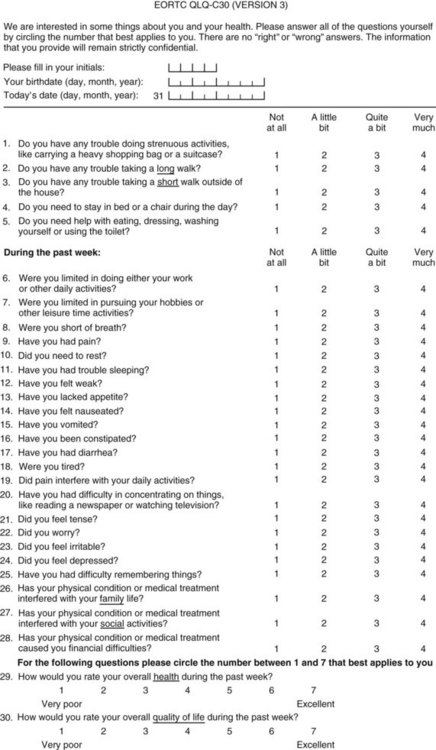
Types of Quality of Life Instruments
Perhaps the gold standard of QoL instruments for cancer patients is the modular questionnaire. Two examples are the Functional Assessment of Cancer Therapy (FACT), also known as the Functional Assessment of Chronic Illness Therapy (FACIT), and the EORTC QLQ-C30. They combine assessment of overall QoL domains—physical, social, functional, and emotional well-being—with disease-specific subscales or “modules.” This approach often eliminates the need for multiple instruments yet results in general and disease-specific or treatment-specific QoL information. The FACT and QLQ-C30 are multilingual and are widely used around the world. They are considered by many experts to be the most valid and standardized instruments for QoL assessment in cancer patients, and each has disease-specific subscales developed for use in patients with hepatopancreatobiliary cancer, such as the FACT-HEP (Blazeby et al, 2004; Fitzsimmons et al, 1999; Heffernan et al, 2002; Kavadas et al, 2003; Pallis & Mouzas, 2004). The FACT-HEP is shown in Figure 26.1, and the QLQ-C30 is shown in Figure 26.2. Disease-specific subscales for the QLQ-C30 include the QLQ-LMC21 (metastatic colorectal cancer), PAN-26 (pancreatic cancer), and HCC-18 (hepatocellular carcinoma).
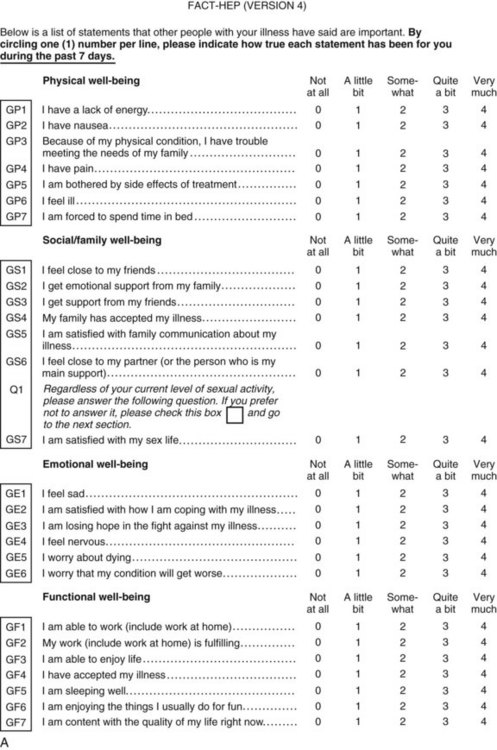
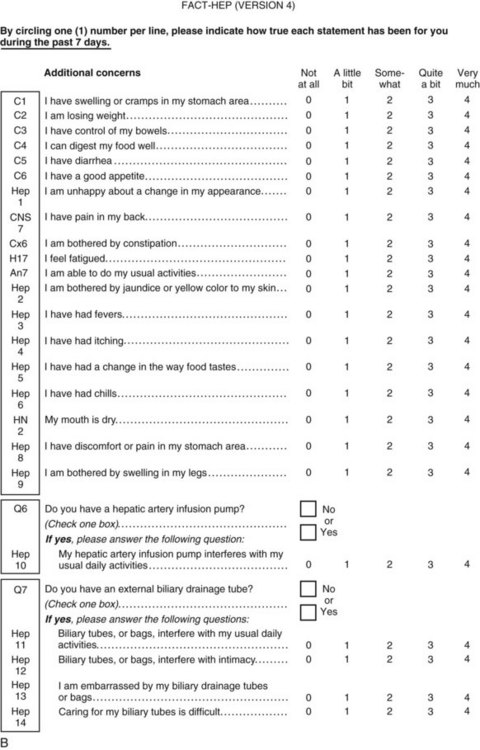
FIGURE 26.1 FACT-HEP QoL questionnaire.
(Courtesy Dr. David Cella at www.FACIT.org, copyright 1987, 1997. Permission for use must be obtained by contacting Dr. David Cella at www.FACIT.org or d-cella@northwestern.edu.)