CHAPTER 2
Proton pump inhibitors
Introduction
Proton pump inhibitors (PPIs) are used clinically in the treatment of acid related disorders, including gastroduodenal (peptic) ulcers, gastroesophageal reflux disease (GERD), nonsteroidal anti-inflammatory (NSAID) induced gastroduodenal ulcers, stress-related ulcer syndrome in critically ill patients, Zollinger-Ellison syndrome (ZES), and as a component of Helicobacter pylori (H. pylori) eradication. Prior to the introduction of PPIs, histamine H2-receptor antagonists (H2RAs) were the mainstay of therapy for these disorders. The introduction of PPIs in the 1980s expanded the therapeutic options and has allowed clinicians to optimize the medical treatment of these acid related disorders.
Mechanism of action, pharmacodynamics, kinetics
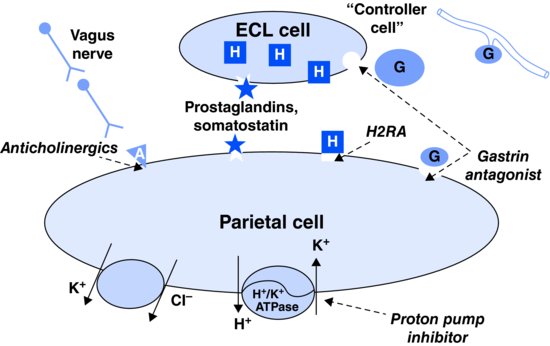
Parietal cells, which comprise ∼85% of the cell population in the stomach, secrete 0.16 M hydrochloric acid (HCl) upon stimulation by acetylcholine, histamine, and gastrin (Figure 2.1). Upon meal stimulation, the parietal cell undergoes intracellular structural changes to increase the surface area of the cell to enable the active transport of H+ ions against a 3 000 000:1 ionic gradient in exchange for K+ (Figure 2.2). With the discovery that the final step in parietal cell acid secretion required an apical surface H+/K+ adenosine triphosphatase (ATPase) enzyme (Figure 2.1), PPIs were developed as specific inhibitors of this ATPase.
Figure 2.1 (A) Electron photomicrograph of parietal cell in the resting (unstimulated) state demonstrating abundant cytoplasmic tubovesicular membranes to which proton pumps – hydrogen potassium ATPase (H+/K+ ATPase) are inserted. (B) Stimulated parietal cell demonstrating translocation of the tubovesicular membranes (containing proton pumps) to the intracellular secretory canalicular membranes, facilitating pump exposure to the highly acidic canalicular lumen.
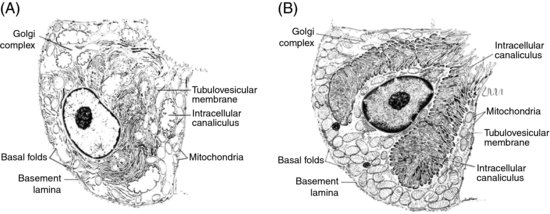
Figure 2.2 Schematic representation of the factors influencing gastric acid secretion by the parietal cell. A number of physiologic mechanisms affect acid secretion: neurocrine (acetylcholine and other neurotransmitters from vagal efferent neurons), paracrine (somatostatin from D-cells and histamine from gastric enterochromaffinlike cells), and endocrine (circulating gastrin) factors. Dashed arrows indicate potential sites of pharmacologic inhibition of acid secretion, either via receptor antagonism or via inhibition of H+/K+ ATPase. A, acetylcholine and other neurotransmitters; EGL, enterochromaffinlike; G, gastrin; H, histamine; PG, prostaglandin; S, somatostatin.
Source: Adapted from MM Wolfe and G Sachs (2000). Reproduced with permission of Elsevier.
The PPIs function as prodrugs that share a common structural motif, a substituted pyridylmethylsulfinyl benzimidazole, but vary in terms of their substitutions, which yield slightly different pKa values. The prodrug is a weak protonatable pyridine that traverses the parietal cell membrane. As the prodrug accumulates in the highly acidic secretory canaliculus, it undergoes an acid catalyzed conversion to a reactive species, the thiophillic sulfenamide. This active moiety then covalently binds to a specific cysteine residue (Cys 813) on the H+/K+ ATPase (via disulfide bond formation) and inactivates it, thus suppressing basal and stimulated gastric acid secretion. The rate of conversion to the active form varies among the PPIs, as activation occurs when the regional pH decreases below the pKa of the specific PPI. Thus, some PPIs may have a slightly faster onset of action, with rabeprazole having the most rapid onset (pKa 5.0), followed by omeprazole, lansoprazole, esomeprazole (pKa 4.0), and finally pantoprazole (pKa 3.9). These pharmacokinetic differences have not proven to be clinically significant.
The PPIs are the most potent inhibitors of gastric acid secretion available when administered correctly, based on their pharmacodynamics. Because acid secretion must be stimulated for maximum efficacy, PPIs should be taken before the first meal of the day. PPIs are most effective when administered after a prolonged fast, when the greatest number of H+/K+ ATPase molecules is present in parietal cells, which is in the morning for most patients. In addition, administration of PPIs should be followed by food ingestion, when the gastric parietal cells are stimulated to secrete acid in response to a meal. Moreover, these drugs should not be used in conjunction with H2RAs, prostaglandins, somatostatin analogs, or other antisecretory agents. Animal studies have demonstrated that the concomitant administration of PPIs and other antisecretory agents markedly reduces the acid inhibitory effects of PPIs. In most individuals, once-daily dosing is sufficient to produce the desired level of acid inhibition. A second dose, if required, should be administered before the evening meal. Importantly, meals should include protein or another stimulant of gastric acid secretion (e.g., coffee). In addition, based on the pharmacokinetics of PPIs, the most effective response occurs with consistent (i.e., daily) dosing, rather than sporadic (i.e., as needed) dosing.
The oral bioavailability of PPIs ranges from 45% (omeprazole) to 85% (lansoprazole). Although PPIs have a circulating T½ of only 1–1.5 hours, the biological T½ of the inhibited complex is ∼24 hours, due to its mechanism of action. Because all the PPIs require accumulation and acid activation, their onset of inhibition is delayed, and after the initial dose, acid secretion continues, but at a reduced level. Subsequently, H+/K+ ATPase enzymes that are recruited to the secretory canaliculus in the parietal cell are then inhibited by additional doses of PPI, further reducing acid secretion. Steady state acid inhibitory properties occur by ∼5 days and inhibit maximal acid output by 66%.
PPIs are principally metabolized by CYP2C19, a member of the hepatic cytochrome P450 family of enzymes, with the exception of lansoprazole, which is mainly metabolized by CYP3A4. It is possible that PPIs may affect the metabolism of other drugs that are metabolized by this family of enzymes, including warfarin, diazepam, phenytoin, digoxin, carbamazepine, and theophylline. Asian populations and the elderly commonly harbor polymorphisms in the CYP2C19 gene, which affects PPI metabolism and has been shown to increase the drugs’ acid inhibitory properties. PPIs are mainly excreted in urine, with the exception of lansoprazole, which is mainly excreted in feces.
Clinical use and dosing
PPIs are widely used and generally considered safe and effective. Six different compounds of proton pump inhibitors currently exist on the market. The specific brand names vary (Table 2.1), depending upon the country of sale, and include omeprazole, lansoprazole, rabeprazole, pantoprazole, esomeprazole, and dexlansoprazole. The first PPI approved for use in the United States was omeprazole, while pantoprazole was the first PPI approved for intravenous use in the USA. With the exception of omeprazole (pregnancy Class C), all PPIs have been categorized as Class B agents.
Table 2.1 Links to proton pump inhibitor trade names
| Dexilant, formerly Kapidex (renamed in the USA to avoid confusion with other medications) | |
| Dexlansoprazole | http://www.takeda.com/news/2010/20100305_3748.html |
| Esomeprazole | http://bddrugs.com/product5.php? idn=5&prev=2&prev1=&prev2= |
| Lansoprazole | http://en.wikipedia.org/wiki/Lansoprazole#Brand_names |
| Omeprazole | http://www.egeneralmedical.com/rxlist00000053.html |
| Pantoprazole | http://bddrugs.com/product5.php?idn=7&prev=&prev1=&prev2= |
| Rabeprazole | http://en.wikipedia.org/wiki/Rabeprazole#Formulations_and_brand_names |
PPIs are used to treat a number of acid-related disorders, including acute gastroduodenal (peptic) ulcer, treatment and prevention of NSAID-associated ulcers, gastroesophageal reflux disease (GERD), medical management of Zollinger-Ellison syndrome prior to definitive surgical treatment, treatment and prevention of GI hemorrhage, stress ulcer bleeding in critically ill patients, and as a component in the treatment of H. pylori eradication. They are also commonly used to treat nonulcer dyspepsia.
Peptic ulcer disease (Table 2.2)
Table 2.2 Recommended proton pump inhibitor doses in active and maintenance therapy of gastroduodenal ulcers* and primary and secondary prevention of NSAID**-induced ulcers
| Proton pump inhibitor | Dose (adult) oral – all administered once daily before breakfast*** |
| Dexlansoprazole | 30–60 mg |
| Esomeprazole | 20–40 mg |
| Lansoprazole | 15–30 mg |
| Omeprazole | 20–40 mg |
| Pantoprazole | 20–40 mg |
| Rabeprazole | 20 mg |
| *Recommended duration of treatment: active duodenal ulcers – treat for 4 weeks, and gastric ulcers – treat for 8 weeks. | |
| **NSAID, nonsteroidal anti-inflammatory drug. | |
| ***Meals should contain protein to enhance parietal cell stimulation. | |
PPIs are the cornerstone of therapy for peptic ulcer disease (PUD) and demonstrate superior efficacy and rate of healing compared to H2RAs in a number of studies. In general, the duration of therapy for acute duodenal ulcers is 4 weeks, and 8 weeks for gastric ulcers. Although the pathogenesis of PUD is often multifactorial and a function of mucosal defense factors and aggressive factors (i.e., H. pylori infection, NSAID use, hypersecretory states), acid secretion plays a central role in ulcer formation, and thus remains the rational target for therapy. While PPIs heal gastroduodenal ulcers more rapidly than H2RAs, no significant differences in ulcer healing have been demonstrated among the various PPIs. A meta-analysis comparing the healing of duodenal ulcers (DU) demonstrated that omeprazole 20 mg every morning for four weeks was superior to both ranitidine 300 mg and cimetidine 800 mg, both administered at bedtime. Similarly, another meta-analysis found that lansoprazole 30 mg every morning healed significantly more ulcers than ranitidine 300 mg and famotidine 40 mg, both administered at bedtime. The pooled healing rates were 60 and 85% for lansoprazole at two and four weeks, respectively, while the corresponding figures for the H2-antagonists were 40 and 75%. Both rabeprazole and pantoprazole have demonstrated superior and accelerated DU healing compared to H2RAs. PPIs also appear to heal gastric ulcers (GU) more rapidly and at a greater rate than H2RAs. For example, a study found that pantoprazole healed 32 and 15% more gastric ulcers at four weeks and eight weeks, respectively, compared to ranitidine. While clearly more effective, as will be discussed, the margin of benefit conferred by PPIs over H2RAs in the healing of ulcers is far smaller than the advantage offered by these agents in the treatment of GERD. Moreover, like H2RAs, the optimal duration of therapy with PPIs should be four and eight weeks of therapy for acute DU and GU, respectively.
NSAID-associated ulcers
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







