Fig. 14.1
The balloon is aligned with the resection plane
3.
The balloon is inflated using distilled water. At this time, the assistant’s maneuver is more important than the endoscopist, since, during this step, it is essential to avoid maximal inflation too quickly. The slow careful dilation is done to prevent perforation and to prevent the balloon being drawn below the ulcer (Fig. 14.2). Dilatation to 15 mm requires a pressure of 8 atmospheres (atm). It takes about 30 s for the balloon to reach a pressure of 3–4 atm. Dilation is performed for approximately 1 min at this pressure, following which the pressure is increased in 1 atm increments over a similar amount of time, until a maximum diameter of 15 mm and pressure of 8 atm is reached. At this point, it is best to withdraw the balloon until it makes contact with the tip of the scope and irrigate the ulcer site with water to visualize the adequacy of dilatation (Fig. 14.3).
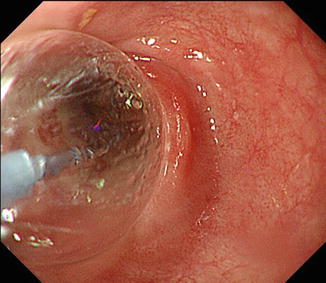
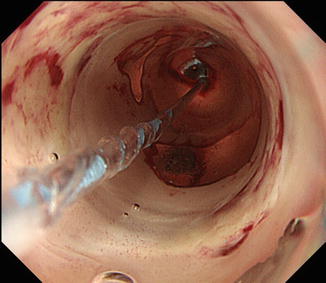
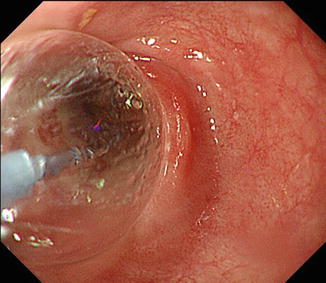
Fig. 14.2
The balloon is slowly pressurized
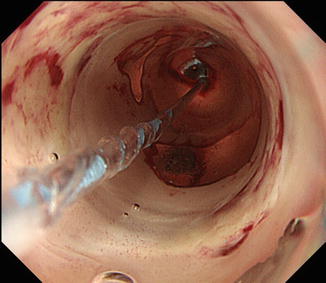
Fig. 14.3
The balloon is pulled slightly back to make close contact with the tip of the scope. It is then irrigated with water to visualize the adequacy of dilation
4.
After dilatation, the ulcer site is inspected to ensure that there are no procedural complications, such as perforation. Bleeding essentially stops naturally and does not usually become a problem (Fig. 14.4).
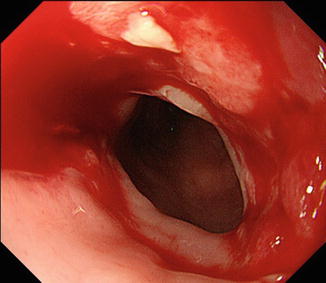
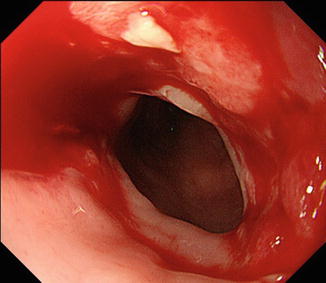
Fig. 14.4
The procedure is completed upon confirmation that there were no procedural complications, such as perforation of the resection plane
EBD is initiated 3–4 days after ESD, and is repeated once a week for semi-circumferential resections and twice a week for circumferential resections. The interval between each EBD is gradually lengthened, and EBD is completed upon confirming that there is complete epithelialization of the entire resection plane, easy scope passage, and absence of dysphagia (Fig. 14.5).
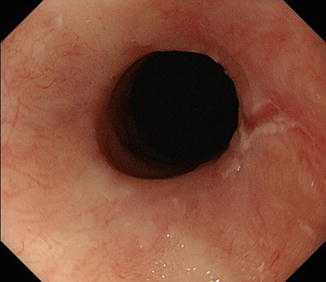
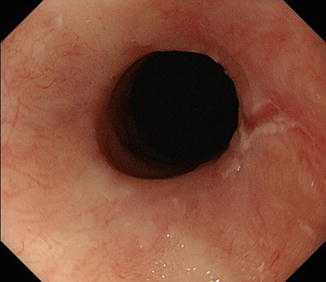
Fig. 14.5
EBD is discontinued upon confirming that there is complete epithelialization of the entire resection plane and easy passage of the scope with no dysphagia
Procedural Complications Associated with EBD
The only case of perforation we experienced with EBD is shown below [10]. ESD was performed on a circumferential lesion (0-IIc, T1a-EP 60 mm) extending from the abdominal to the lower thoracic esophagus, thus requiring a circumferential resection (Fig. 14.6a, b). Four days after ESD, EBD was performed. The resection area had narrowed slightly, and there was resistance to passage of the scope. Thus, dilatation was performed by directly inserting the balloon up to the stricture site from the proximal side of the resection area. This resulted in the tip of the balloon penetrating the esophageal wall, and a large perforation was detected, through which the mediastinum was visible (blue arrow) (Fig. 14.6c). Since closure of the perforation was considered impossible, the patient’s course was observed conservatively in collaboration with the surgical department. Although the patient developed a fever for 2 days, the inflammation subsequently subsided, and no superior mediastinal abscess developed, as seen by computed tomography (CT). Further, since esophageal imaging 1 week later did not show any leakage, balloon dilatation was once again performed 10 days after the perforation, with a balloon diameter of 7 mm. The procedure was performed twice a week, and normal oral intake was possible 2 months later (Fig. 14.6d). In this case, the perforation was caused by not advancing the guidewire when the balloon was advanced from above the resection area. This indicates that it is very important to be extremely careful when performing EBDs, since resection planes that have not epithelialized are extremely soft and the tip of the balloon can penetrate the esophageal wall.
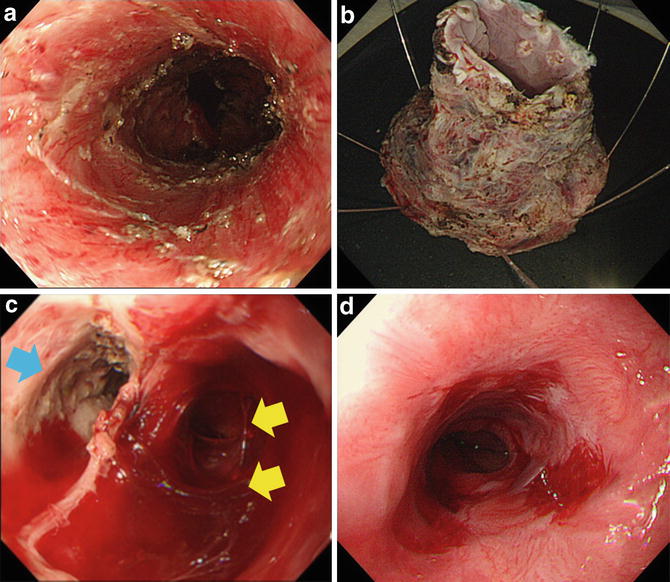
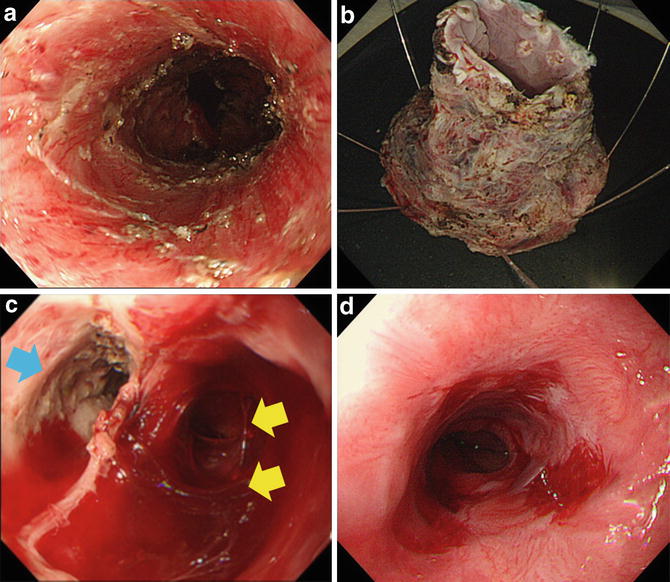
Fig. 14.6
(a) Image taken after circumferential resection of a 6 cm lesion extending from the abdominal esophagus to the lower esophagus. (b). Freshly resected specimen. (c). Giant perforation following balloon dilatation 4 days after ESD. The blue arrow indicates the original esophageal lumen. The yellow arrows indicate the mediastinum observed in the depths of the perforation site. (d) Post-balloon dilatation performed 2 months after ESD. Normal oral intake was possible despite the presence of mild lacerations
Outcome of EBD (Table 14.1)
Table 14.1
Treatment outcome following EBD
EBD group (30 lesions in 29 patients) | ||
|---|---|---|
Circumferential spread | Semi-circumferential dissection: 25 | Circumferential dissection: 3 |
Mean number of dilatations | 6.5 times (1–20) | 12.3 times (5–20) |
There were 30 lesions in 29 patients that required postoperative balloon dilatation at our institution until December 2007. Of these 29 patients, 24 were men and 5 were women, with a mean age of 70 years (range: 49–90). Many of the lesions had ≥ two-thirds circumferential spread, and nearly all lesions exceeded semi-circumferential spread. Three of these were lesions that required full circumferential resection. There were two lesions in the upper thoracic esophagus that did not require semi-circumferential resection, although EBD was required since they were close to the physiological sphincter area. The overall mean number of EBDs performed was 7.1 times (1–20), although differences in the number of dilatations did not depend on the diameter or site of dissection. The mean number of EBDs performed in the 25 semi-circumferential resection lesions was 6.5 times (1–20), and 12.3 times (5–20) in the 3 circumferential resection lesions, demonstrating that dilatation tended to be required more frequently with full circumferential resection. The aforementioned case of perforation was the only complication associated with EBD.
Endoscopic Triamcinolone Injection (ETI)
Local Steroid Injection Protocol
With EBD, normal oral intake became possible in all patients after ESD. However, frequent EBD, the requirement of dilatation over an extended period of time, and the risk of perforation during dilatation are some of the drawbacks of this treatment option. Thus, at our department, we introduced local steroid injection therapy, which had previously been used as post-dilatation treatment for esophageal inflammation or postoperative anastomotic strictures, to prevent strictures after ESD [8]. The protocol and precautions of the procedure are described below.
Steroid
Triamcinolone acetonide (Product name: Kenacort®-A), a synthetic corticosteroid, is used for the procedure (Fig. 14.7). One vial contains 5 ml of a white aqueous suspension (triamcinolone acetonide: 50 mg). Since esophageal inflammation (corrosive esophagitis after using an autoscope) and post-esophageal dilatation are listed as indications for the use of this drug, we selected triamcinolone acetonide for use at our institution.










