Site
Author
Year
n
Delayed bleeding (%)
Reference
Stomach
Oda
2005
1,033
6.0
[8]
Kakushima
2006
383
3.4
[9]
Imagawa
2006
159
0
[10]
Onozato
2006
171
7.6
[11]
Oda
2006
303
0
[12]
Hirasaki
2007
112
4.0
[13]
Jung
2007
552
7.6
[14]
Takizawa
2008
1,083
5.8
[15]
Ono
2008
314
8.3
[16]
Takenaka
2008
306
0.7
[17]
Hoteya
2009
572
4.9
[18]
Isomoto
2009
589
1.7
[19]
Chung
2009
1,000
15.6
[20]
Takizawa
2009
1,382
9.7
[21]
Hotta
2010
703
0.3
[22]
Mannen
2010
478
8.9
[23]
Goto
2010
454
5.7
[24]
Tsuji
2010
398
5.8
[25]
Ahn
2011
833
5.3
[26]
Akasaka
2011
1,188
3.1
[27]
Lee
2011
806
4.2
[28]
Higashiyama
2011
924
3.0
[29]
Okada
2011
647
4.3
[30]
Sugimoto
2012
485
3.7
[31]
Goto
2012
1,814
5.5
[32]
Toyokawa
2012
1,123
5.0
[33]
Table 16.2
The rate of delayed bleeding after ESD for esophagus and colorectum
Site | Author | Year | n | Delayed bleeding (%) | Reference |
|---|---|---|---|---|---|
Esophagus | Fujishiro | 2006 | 58 | 0 | [34] |
Kakushima | 2006 | 30 | 0 | [35] | |
Takizawa | 2007 | 87 | 0 | [36] | |
Yoshinaga | 2008 | 25 | 0 | [37] | |
Ishihara | 2008 | 110 | 0 | [38] | |
Ono | 2009 | 107 | 0 | [39] | |
Hirasawa | 2010 | 58 | 5.2 | [40] | |
Ishii | 2010 | 37 | 0 | [41] | |
Repici | 2010 | 20 | 0 | [42] | |
Tanaka | 2012 | 246 | 1.2 | [43] | |
Isomoto | 2013 | 291 | 0.7 | [5] | |
Kanzaki | 2013 | 48 | 2.1 | [44] | |
Colorectum | Fujishiro | 2007 | 200 | 1.0 | [45] |
Saito | 2007 | 200 | 2.0 | [46] | |
Tanaka | 2007 | 70 | 1.4 | [47] | |
Hurlstone | 2007 | 42 | 2.3 | [48] | |
Onozato | 2007 | 35 | 0 | [49] | |
Tamegai | 2007 | 71 | 0 | [50] | |
Toyonaga | 2009 | 468 | 1.5 | [51] | |
Zhou | 2009 | 74 | 1.3 | [52] | |
Isomoto | 2009 | 292 | 0.7 | [53] | |
Yoshida | 2010 | 119 | 1.6 | [54] | |
Saito | 2010 | 1,111 | 1.5 | [4] | |
Hotta | 2012 | 219 | 2.7 | [55] | |
Hotta | 2012 | 146 | 1.4 | [56] | |
Yoshida | 2013 | 530 | 2.3 | [57] |
How to successfully manage bleeding both during and after ESD will be discussed in this chapter.
Preparation
Before starting training of ESD, pre-procedural, theoretic preparation is necessary. An endoscopist who intends to learn ESD must learn not only about the technique of ESD, but also the basic knowledge of bleeding (e.g. risk factors, incidence, management, etc.), as well as apparatuses such as electrosurgical units, endoscopic knives, and various other devices. The physician should also check all information of ESD patient, such as the past medical history and daily medications, especially anticoagulant agents.
The next steps for trainees are to observe expert endoscopists in action as they perform ESD procedures and assist experts performing the procedure, before beginning themselves. By assisting experienced endoscopists, trainees acquire the skills needed to troubleshoot various situations. Moreover, obtaining expertise in hemostasis before starting ESD is highly recommended since most of the difficulties surrounding the procedure are related to uncontrollable hemorrhage [58].
Instruments
An endoscope with a water jet function (GIF-Q260J, Olympus, Tokyo, Japan) mounted with a soft transparent hood (TOP Co. Ltd., Tokyo, Japan) is mainly used. This helps facilitate placement of the endoscope, especially during tumor dissection. Normal saline has been used as the injection solution for EMR; however, to achieve better lifting of the lesion in order to lessen the risk of perforation and to lessen tissue damage of the resected specimen, a solution containing sodium hyaluronate has been developed [59]. Many groups now use a commercially available solution of 0.4 % sodium hyaluronate (MucoUp, Johnson & Johnson, Tokyo, Japan). These solutions are usually combined with diluted epinephrine, which is used for the prevention of active bleeding.
Various knives can be used in ESD. At our institution, we developed IT knife-2 (KD-611L; Olympus, Tokyo, Japan). The difference between the IT knife (KD-610L; Olympus, Tokyo, Japan) and the IT knife-2 is the attachment of a short, three-prong blade between the needle and the ceramic tip (Fig. 16.1a, b). Drawbacks in cutting performance of the IT knife have been remarkably improved with the IT knife-2, such as cutting difficulty while the endoscope is looking downward and the relatively poor performance of cutting in a lateral direction. Consequently, the operating time using the IT knife-2 is reported to be much shorter than that using the original IT knife [16, 36, 60].
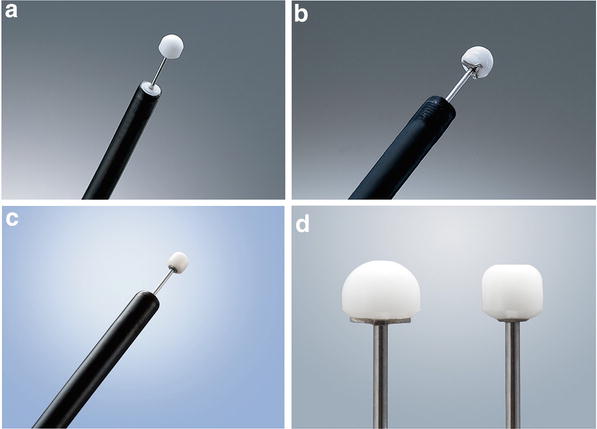
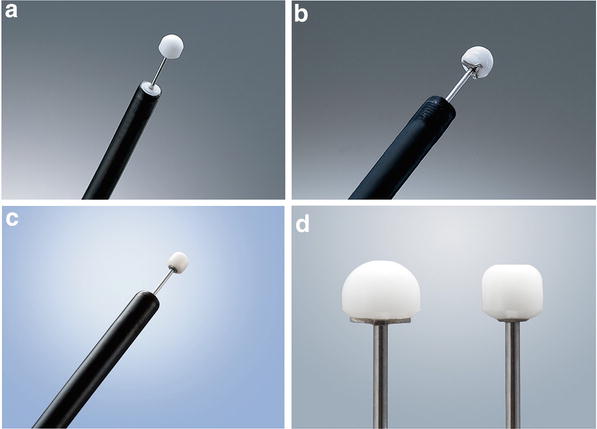
Fig. 16.1
IT knife series. (a) Original IT knife (KD-610L; Olympus, Tokyo, Japan). (b) IT knife 2 (KD-611L; Olympus, Tokyo, Japan). (c) IT knife nano (KD-612L; Olympus, Tokyo, Japan). (d) IT knife 2 and IT knife nano
Since the development of IT knife-2 was mainly for application in the stomach, the insulated tip was too large to be used in the esophagus and colon where the submucosal layer is thinner and the lumen is narrower. To solve these issues, the new IT knife nano (KD-612L; Olympus, Tokyo, Japan) was recently developed, which has a smaller insulated tip (Fig. 16.1c, d). Now, the IT knife-2 is mainly used for gastric ESD, and IT knife nano for esophageal and colonic ESD.
At our institution, the VIO300D (Erbe, Germany) is mainly used as the electrosurgical unit. The instruments and settings are shown in Table 16.3. For hematemesis, we use hot biopsy forceps (Radial jaw, Boston Scientific, Tokyo, Japan) for stomach, and Coagrasper (FD-410LR, Olympus, Tokyo, Japan) (Fig. 16.2) for esophagus and colon. In cases of severe bleeding that could not be stopped by coagulation, endoclips were deployed. Because endoclips interfere with the subsequent resection procedure or dissection, one should dissect more submucosal tissue around the bleeding site in order to better expose the bleeding site before clipping.
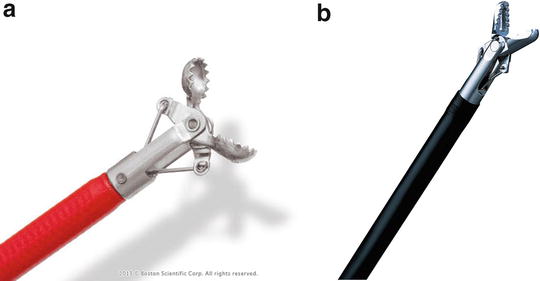
Table 16.3
Instruments and conditions for ESD
Stomach | Esophagus | Colorectum | ||||
|---|---|---|---|---|---|---|
Device | VIO300D | Device | VIO300D | Device | VIO300D | |
Marking | APC | Forced APC, 40 W, 1.8 L/min | APC | Precise APC, E3, 1.8 L/min | – | – |
Precut | Needle knife | Dry cut, E 4, 50 W | Needle knife | Dry cut, E3, 30 W | Dual knife | Endocut Q, E3-D2-I2 |
Mucosal incision | IT-2 | Endocut Q, E3-D1-I2 | IT-nano | Endocut Q, E3-D1-I1 | Dual knife | Endocut Q, E3-D2-I2 |
Submucosal dissection | IT-2 | Swift coag, E5, 100 W | IT-nano | Swift coag, E5, 45 W | IT-nano/Dual knife | Swift coag, E3, 40 W |
Minor oozing | IT-2 | Swift coag, E5, 100 W | IT-nano | Swift coag, E5, 45 W | IT-nano/Dual knife | Swift coag, E3, 40 W |
Major bleeding | Hot biopsy | Soft coag, E6, 100 W | Coagrasper | Soft coag, E6, 80 W | Coagrasper | Soft coag, E5, 80 W |
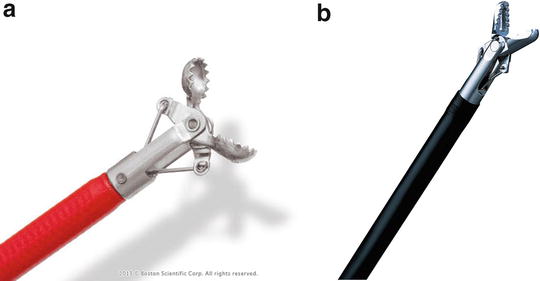
Fig. 16.2
Hemostatic forceps. (a) Hot biopsy forceps (Radial Jaw 4, Boston Scientific, Tokyo, Japan). (b) Coagrasper (FD-410LR, Olympus, Tokyo, Japan)
Bleeding During ESD (Immediate Bleeding)
Bleeding during the procedure is infrequent with EMR techniques, but is quite common and almost unavoidable with ESD. It sometimes requires the procedure to be withheld or aborted; however, with the development of new endoscopic techniques and technology, it now only rarely becomes significant to the extent that requires the procedure to be aborted [8]. Management of immediate bleeding plays a critical role in the successful completion of ESD.
Immediate bleeding was found in 63 of 945 patients (7 %) in a previous report, in which immediate bleeding was defined as the diminution of 2 g/dL in hemoglobin (Hb) between pre-procedure and next-day levels [8]. The rates of significant immediate bleeding in the upper and middle thirds of the stomach are higher than in the lower third (Table 16.4) because of the larger diameter of the submucosal arteries in the upper and middle thirds of the stomach [61].
Table 16.4
Relation between immediate/delayed bleeding and lesion location, size (from Oda et al. [8])
Immediate bleeding | Delayed bleeding | ||||
|---|---|---|---|---|---|
Location | U | 8 % | (14/176) | 1 % | (1/176) |
M | 8 % | (35/431) | 6 % | (27/431) | |
L | 3 % | (14/426)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| |||





