Pouch Configurations
R. John Nicholls
Paris P. Tekkis
Introduction
The only reason for restorative proctocolectomy (ileal pouch-anal anastomosis [IPAA]) is to avoid a permanent ileostomy. A conventional proctocolectomy gives otherwise excellent results. Where there is no medical objection, the choice lies between a restorative and a conventional proctocolectomy and is almost entirely the patient’s wish to make. This decision is possible only if the disadvantages are fully discussed. These include failure and complication rates, total treatment time, the possibility of pouchitis, and the likely functional outcome. A pouch support nurse, stomatherapist, and patient-support group can offer valuable advice, but in the end the patient must decide.
Historical Background
The configuration of the pouch or reservoir is only part of the operation of restorative proctocolectomy. When the operation was first reported by Parks, a three-loop form of reservoir was used. This S-pouch was connected to the anal canal after a mucosectomy by an anastomosis between a point just above the dentate line and a segment of the terminal ileum projecting from the reservoir a few centimeters long. Parks said at the time that his main aim was to avoid incontinence and to do so he favored this form of reconstruction. Although this goal was achieved as reported in the first few publications (1,2,3), the price paid was failure of spontaneous evacuation in at least half of the patients having the procedure. This problem was radiologically shown (4) to be due to the distal ileal segment, which acted as an impedance to outflow. The two-loop reservoir described by Utsunomiya (5) did not have this feature, it being directly joined to the anal canal without any intervening ileum. Evacuation was spontaneous in almost all patients.
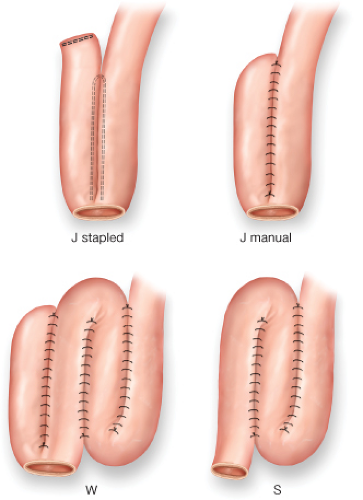
For this reason and also for its ease of construction by linear stapling the two-loop or “J” reservoir has become the most widely used reconstruction. Other configurations have included the “H” reservoir described by Fonkalsrud (6), the Kock, “K” design used with ileoanal anastomosis (IAA), and a four-loop reservoir, the “W” (7) (Fig. 30.1). The last was developed with the intention of achieving lower frequency of defecation, which followed the J reservoir since it was more capacious with an inverse relationship between frequency and capacitance having been demonstrated for straight ileoanal (8), ileal pouch-anal (9), and colonic pouch-anal (10,11) reconstructions.
The general indications for restorative proctocolectomy have been dealt with elsewhere. In considering the specific indication for using a reservoir as opposed to a straight segment of small intestine, there has never been a trial in adult patients comparing no reservoir (straight ileoanal) with a reservoir reconstruction. One of the few pieces of evidence for lower frequency with the latter comes from a nonrandomized comparison by Martin et al. in which 16 patients having a straight ileoanal reconstruction had a frequency of 8 defecations per 24 hours compared with 4 per 24 hours in 14 patients having an ileal reservoir (12). Other evidence comes from physiological studies of patients who have had either a straight or a pouch reconstruction (13) and from patients who have shown an inverse relationship between frequency of defecation and capacitance of the reservoir measured by balloon volumetry (8,9,10).
There are no particular indications other than the surgeon’s preference in choosing which pouch should be used other than the “S” reservoir, which with its evacuation difficulty has almost died out. In current practice, therefore, the J pouch predominates, with a much smaller proportion of patients having a W pouch. The latter is still used in some units, however, and in recent years it may have increased its use following some evidence that long-term function is better (Table 30.2). The length of small intestine used for each is similar and the mobility of the mesentery that determines whether or not there will be some tension on the anastomosis is also similar for both “J” and “W” reservoirs.
Table 30.2 Functional Outcomes by Reservoir Design | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
As long as an ileoanal anastomosis is possible, there is no particular preoperative planning required for the reservoir. The choice of configuration is unaffected by general factors such as the patient’s condition or medication requirements. There are no local anatomical
or pathological factors, which would lead to one or other type being preferred. Thus, the width of the pelvis, mobility of the mesentery, the state of the anal sphincter, and the extensiveness of any adhesions do not influence the choice of reservoir.
or pathological factors, which would lead to one or other type being preferred. Thus, the width of the pelvis, mobility of the mesentery, the state of the anal sphincter, and the extensiveness of any adhesions do not influence the choice of reservoir.
The technique forms only a part of restorative proctocolectomy (IPAA), which has been described in detail in the foregoing sections. Briefly, it involves removal of the colon and the rectum using either an open or laparoscopic technique followed by the construction of an ileal reservoir, which is then joined to the anal canal by an IAA. The IAA can be carried out using a manual or stapled technique.
General Points
The following precautions should be observed:
Antibiotics—Single-dose perioperative antibiotic cover should be used, but if the duration of operation exceeds 3 hours, a second dose of antibiotic is advisable, particularly if the antibiotic has a short half-life. In immunosuppressed patients receiving drugs such as cyclosporin or biological sulfonamides may still have a role in protecting against Pneumocystis carinii pneumonia.
Anti-embolism prophylaxis using subcutaneous heparin, pneumatic compression, and anti-embolism stockings for prophylaxis.
Anesthesia—Blood (usually 4 units) should be crossmatched and available if necessary. If a central venous line is needed for total parenteral nutrition, this should be inserted at the end of the operation. If the operation is carried out by an open technique, the abdominal wound will be an important cause of pain and an epidural anesthetic should be given.
Positioning—The reversed Trendelenburg position with the legs raised (Lloyd-Davies) should be used, thereby allowing access to the anus, and the tip of the coccyx should lie over the end of the operating table to gain adequate exposure of the perineum. Whether an open or laparoscopic technique is used, this position gives excellent access to the abdomen and suitable deployment of surgeon and assistants around the patient.
The bladder is routinely catheterized. It is helpful to insert a proctoscope before starting to drain the bowel of as much liquid feces and flatus as possible.
Surgical Technique
General Considerations of Pouch Construction
There are three principles that should be observed in constructing a reservoir:
Minimal tension in the mesentery
Adequate capacitance of the pouch
Absence of distal ileal segment
To minimize tension, as full a mobilization of the mesentery as possible combined with division of selected mesenteric vessels if necessary should be performed combined with a trial descent. To achieve adequate capacity a minimum length of small bowel of 40 cm is required. Using the apex of a folded pair of loops as the point for the enterostomy to form the IAA will avoid any distal ileal segment.
Mobilization of the Mesentery
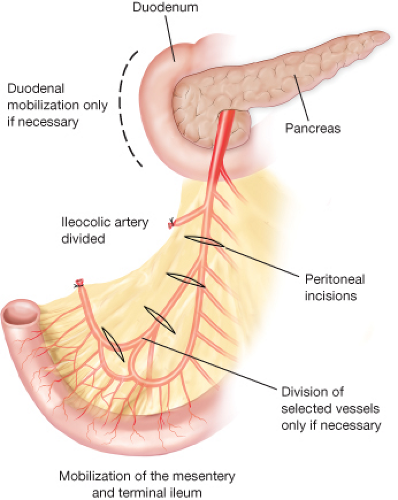
Once the colon and the rectum have been removed, an assessment of the mobility of the small bowel to descend to the pelvis is made by holding the apex of a loop of terminal ileum intended to form part of the IAA down into the pelvis. This most mobile point is around 15 cm from the ileocecal junction. If there is no evidence of tension,
no further mobilization of the mesentery is carried out. If, however, there is some tension, then further mobilization of the mesentery is required. This goal is achieved in three ways (Fig. 30.2):
no further mobilization of the mesentery is carried out. If, however, there is some tension, then further mobilization of the mesentery is required. This goal is achieved in three ways (Fig. 30.2):
Mobilize the mesentery
Perform transverse incisions of the peritoneum
Divide selected vessels if necessary
It may be necessary to mobilize the duodenum using Kocher’s maneuver. The uncinate process of the pancreas can be freed from the origin of the superior mesenteric artery and vein if necessary. Care should be taken to avoid damage to the superior mesenteric vein or its major tributaries. Usually, however, this step is not required. Four or five small transverse cuts made in the peritoneum on each side of the mesentery result in lengthening by 1 or 2 cm.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree