End-to-End, Side-to-End Anastomosis
Marylise Boutros
Anthony M. Vernava III
Sphincter-saving resections for rectal cancer and other benign conditions of the rectum have become standard over the last 20 years, having replaced abdominoperineal resection for many patients. Our experience with low colorectal anastomosis is vast and our understanding of long-term outcomes is increasingly clear. The stapled straight end-to-end anastomosis (EEA) is the standard low colorectal anastomotic technique (1). Although this low anastomosis frees the patient from a colostomy, unfortunately, it has a high rate of anastomotic leak and bowel dysfunction.
Anastomotic leaks after colon resection occur at a rate less than 3%, whereas rectal anastomoses have a reported leak rate of 10–20% (2). This increase in the risk of anastomotic leak is thought to be due to the devascularization ensued by a total mesorectal excision, the technical difficulty of a low pelvic anastomosis, and the impact of neoadjuvant radiation on bowel healing (3,4). The mortality (2–7%) associated with this complication is significant (5).
Several alternate anastomotic approaches have been developed in an attempt to diminish these complications. There are restorative reconstructions, including the colonic J-pouch and transverse coloplasty, which may be used for coloanal anastomoses (discussed elsewhere in this chapter) as well as a low colorectal side-to-end anastomosis. This is a variation on the standard EEA anastomosis.
Contraindications
In order to perform a low colorectal anastomosis, an oncologically sound resection that spares the sphincters must be possible.
Furthermore, any patient undergoing a low colorectal anastomosis must have adequate preoperative continence and sphincter function, as increased stool frequency and diminished continence can result even in the best circumstances.
Similarly all preexisting patient risk factors for anastomotic complications such as anemia, malnutrition, smoking, or cigarette should be corrected and the need for a proximal protective loop ileostomy be considered in all the cases.
Prior to a low colorectal resection, consent should be obtained for a possible permanent colostomy or a temporary diverting ileostomy. The location of both of these stomas should be marked preoperatively while the patient is sitting and standing.
Preoperative mechanical preparation of the bowel is undertaken before resection of the rectum.
General anesthesia is induced. Broad-spectrum antibiotic coverage (7) for prevention of surgical site infections and prophylaxis (8) for deep vein thrombosis (with subcutaneous unfractunated heparin injection and sequential compression devices) is initiated at this time.
A bladder catheter is placed after induction of anesthesia.
Patient Positioning
The patient is placed in the appropriate positioning specific to the operative approach (open, laparoscopic, or robotic). However, despite the approach a few key principles will facilitate fashioning the anastomosis:
The patient is placed in the modified lithotomy (with appropriate stirrups) or split-leg position in Trendelenburg.
After exploratory laparotomy, the small bowel is packed away in the upper abdomen. This positioning gives the surgeon the best access to the pelvis.
Mobilization
The splenic flexure and the distal large bowel are fully mobilized along with the rectum as described elsewhere in this chapter. For there to be enough proximal colon to fashion a tension-free anastomosis, a high ligation of the inferior mesenteric artery and inferior mesenteric vein is usually necessary. Rectal resection with total or partial mesorectal excision, as indicated by the location of the tumor, is performed. The posterior dissection plane is developed in an avascular areolar tissue plane all the way to the pelvic floor. The dissection plane can be followed around the pelvis to the lateral peritoneal attachments. The attachments are incised to release the rectum. For mid to low rectal tumors, the anterior lateral ligaments containing the middle hemorrhoid vessel are divided with electrocautery at the sidewall of the pelvis to remove all of the mesenteric fat.
Bowel Preparation for Anastomosis
The distal resection margin is chosen and the mesorectal fat is circumferentially cleared off. A linear stapler is fired across the rectum; this can be laparoscopically done using an Echelon® (Ethicon, Cincinnati, OH, USA) or Endo GIA® (Ethicon, Cincinnati, OH, USA) or in an open procedure using a number of stapling devices including the Contour curved cutter® (Ethicon, Cincinnati, OH, USA) or TA stapler. It is imperative to ensure that the rectum has been completely stapled and closed (Fig. 16.1).
Operative Technique for the EEA Anastomosis
This technique is the standard method to construct low colorectal anastomoses. Since the advent of the circular end-to-end stapler and the description of the EEA anastomosis
in 1979, this technique has evolved from a double purse-string EEA anastomosis to a double-stapled EEA anastomosis (9,10).
in 1979, this technique has evolved from a double purse-string EEA anastomosis to a double-stapled EEA anastomosis (9,10).
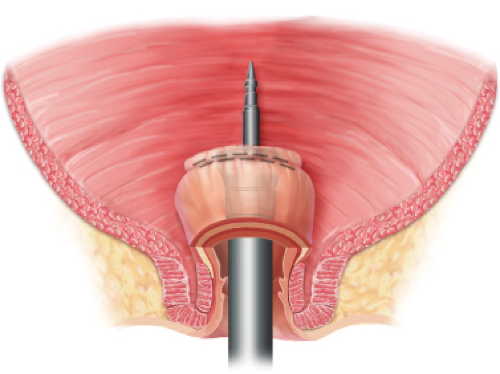 Figure 16.1 Schematic representation of the distal rectal stump with EEA stapler introduced. This is used for both the end-to-end and end-to-side anastomoses. |
The proximal resection margin is chosen in an area that is non-inflamed and free of diverticula. It is imperative at this point to confirm that the proposed proximal resection margin can easily reach the stapled rectal stump without any tension. Then, the remaining mesocolon is divided.
A purse-string clamp is placed at the transection line and the colon is divided just distal to the clamp using a long-handled knife. Next a nonabsorbable, monofilament suture such as 2.0 nylon on a straight needle is threaded through the purse-string clamp and the clamp is removed. Alternatively, the colon is divided at the proximal transaction line using a long-handled knife and a hand-sewn purse-string suture using 2.0 prolene is placed on the cut edge of the bowel. The specimen is removed.
The circular stapler anvil (typically size 28, 29, or 33) is gently introduced into the proximal bowel and secured in place using the purse-string suture.
It is important to ensure that there are no diverticula or mesocolonic tissue on the surface of the bowel where the EEA stapler will be fired.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


