Laparoscopic Medial to Lateral
Toyooki Sonoda
The laparoscopic dissection of the right colon is generally thought to be more straightforward than the transverse colon, left colon, or the rectum. There are two general approaches, one where the colon is mobilized from its lateral attachment first (the lateral approach), and one where the vascular pedicles are initially ligated, followed by colonic mobilization (the medial approach). Both accomplish the same dissection, but advantages to the medial-to-lateral approach include the following:
Early ligation of the vascular pedicles in cancer may theoretically prevent the liberation of tumor cells into the mesenteric circulation during mobilization (the Turnbull “no-touch” technique)
Preservation of the lateral colonic ligament until the end of the mobilization keeps the right colon fixed in place, limiting the need to manipulate a floppy colon
Indications
The most common indications for a laparoscopic right colectomy include malignant neoplasm, benign polyp not amenable to colonoscopic removal, and Crohn’s disease. Uncommon yet possible indications are right-sided diverticulitis, chronic volvulus, hemorrhage, and ischemia.
Contraindications
There are both absolute and relative contraindications to the laparoscopic approach to colectomy. Absolute contraindications include:
Hemodynamic instability
Known history of extensive adhesions from prior surgery
The relative contraindications to laparoscopy depend on each clinical circumstance, and the skills and comfort levels of the surgeon, including
Large tumor size (>8 cm)
Tumor invading other structures
Bowel dilation from obstruction or ileus
Emergency surgery
History of prior surgery
A patient may have had many operations in the past, but the amount of adhesions may not prohibit a subsequent laparoscopic colectomy. For example, even patients who have undergone one or two open ileocolic resections for Crohn’s disease may still be candidates for laparoscopic ileocolectomy. When extensive adhesions are present and a conversion to open surgery is necessary, it is important that the decision to convert is made early in the operation. Omental adhesions to the abdominal wall, even if extensive, can be favorable for the laparoscopic approach; significant intraloop adhesions are usually not as easily managed.
The patient should be prepared for surgery as usual, with attention paid to preoperative comorbidities. Neoplasms should be evaluated with preoperative computed tomographic scan, complete colonoscopy whenever possible, and magnetic resonance imaging or positron emission tomographic scan when appropriate. Patients with Crohn’s disease should undergo colonoscopy and complete imaging of the small intestine using a computed tomographic or magnetic resonance enterography.
Whenever a lesion is present, especially one that may not be visible on the serosal surface, an endoscopic tattoo should be placed using India ink. This maneuver allows for laparoscopic identification of the tumor-bearing segment, and helps eliminate the possibilities of removing an incorrect segment of intestine or resecting a tumor with inadequate lateral margins. The tattoo should be placed in a uniform manner, in multiple quadrants to assure that the tattoo is visible on the serosal surface and not hidden by the mesentery. The author favors a tattoo in three quadrants, distal to the tumor. Placing a tattoo both proximally and distally may lead to confusion if only one area is visible.
The use of mechanical bowel preparation prior to surgery is controversial. Several randomized prospective trials do not show advantages to bowel preparation in terms of anastomotic leaks and wound infections. However, with the laparoscopic approach, the ability to palpate the bowel is limited. If the location of a tumor or polyp cannot be ascertained during laparoscopic surgery, an intraoperative colonoscopy should be performed rather than a blind resection. This, of course, would be difficult in the setting of an unprepared colon. The use of CO2 colonoscopy limits bowel distension during surgery, and this can be performed without any proximal bowel occlusion due to the rapid absorption of intraluminal CO2. If air colonoscopy is used, however, the terminal ileum should be occluded with a bowel grasper to avoid small bowel distension.
Patients undergoing laparoscopic bowel resection should receive appropriate intravenous antibiotics within one hour of skin incision. For a lengthy operation, the antibiotics must be redosed intraoperatively based on their pharmacokinetics. Prophylaxis against deep vein thrombosis should be preoperatively given.
Positioning
A gel pad is placed on the operating table to avoid patient slippage during extreme tilt. Although a laparoscopic right colectomy can be performed in the supine position, the
author prefers to use the modified lithotomy position, with both the arms tucked at the sides. The hip flexion must be kept to a minimum, or the thighs will obstruct the laparoscopic instruments during upper abdominal dissection. The advantages of this positioning are as follows:
author prefers to use the modified lithotomy position, with both the arms tucked at the sides. The hip flexion must be kept to a minimum, or the thighs will obstruct the laparoscopic instruments during upper abdominal dissection. The advantages of this positioning are as follows:
In a difficult right colectomy, the surgeon or assistant can stand between the legs and help with retraction through an additional port
When a lesion (or tattoo) is difficult to identify, an intraoperative colonoscopy can be performed
In cases of ileal Crohn’s disease, there could be an occult ileosigmoid fistula requiring sigmoid colon resection
Technique
Port Placement
The camera port is placed in a periumbilical position. Whether it is placed superior or inferior to the umbilicus is based on the body habitus and location of the umbilicus. The camera port is best placed at the “top of the dome” when the abdomen is insufflated; in most patients, this could be in the infraumbilical position. However, when the umbilicus is located low in the abdomen (as a result of obesity and in some males), the camera port is best placed in the supraumbilical position. In the majority of cases, this periumbilical port wound is extended around the umbilicus for exteriorization of the colon, resection, and anastomosis.
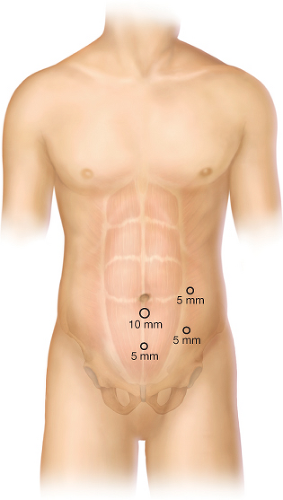
The port placement is illustrated in Figure 3.1. We favor the blunt Hasson technique (10 mm or 12 mm) for the camera port. The surgeon begins the operation from the left side of the patient using the left lower quadrant and suprapubic ports. The assistant stands to the right of the surgeon, holding the camera and using the left upper port. A monitor near the right shoulder of the patient is used by both operators. After vascular ligation and medial-to-lateral retromesenteric dissection, the surgeon moves to the right of the assistant, using the two left-sided ports, for the hepatic flexure takedown and lateral ligament mobilization. The assistant helps through the suprapubic port.
Operative Steps
The following are the general operative steps in a medial-to-lateral laparoscopic right hemicolectomy:
Isolation and division of the ileocolic pedicle
Isolation and division of the right branch of the middle colic vessels
Separation of the right colon and mesentery from the retroperitoneal fascia in a medial-to-lateral direction
Dissection of the gastrocolic ligament, takedown of the hepatic flexure and lateral ligament
Dissection of the ileum and mesentery from the retroperitoneum
Division of the bowel proximally and distally
Anastomosis
Ileocolic Pedicle
The patient is placed in a slight Trendelenburg position. The omentum is lifted above the transverse colon, and the distal ileum is moved into the pelvis. The patient is tilted (airplaned) steeply with the right side up, and the small bowel loops are swept to the left of the midline.
The operation starts with the isolation of the ileocolic pedicle. The ileocolic artery is a proximal branch of the superior mesenteric artery that courses just inferior to the third portion of the duodenum. Therefore, the identification of the duodenal sweep through the mesentery as the transverse colon is superiorly retracted is an important initial step in identifying the ileocolic pedicle. Ample tension on this vessel is critical
in distinguishing it from the superior mesenteric vessels. With traction on the ileocecal region in an anterolateral direction, the ileocolic artery will be seen “bowstringing” through the mesentery (Fig. 3.2). The right colic artery arises from the ileocolic pedicle to supply the hepatic flexure about 90% of the time, and does not need to be separately ligated. In a minority of cases, it will branch from the superior mesenteric artery, superior to the ileocolic pedicle, and will need ligation. Distal in its course, near the ileocecal junction, the ileocolic artery becomes the ileal branch (and accessory ileal branch), which can bleed if injured. Therefore, the dissection of the ileocolic artery should start in the avascular plane between the superior mesenteric vessels and the ileal branch.
in distinguishing it from the superior mesenteric vessels. With traction on the ileocecal region in an anterolateral direction, the ileocolic artery will be seen “bowstringing” through the mesentery (Fig. 3.2). The right colic artery arises from the ileocolic pedicle to supply the hepatic flexure about 90% of the time, and does not need to be separately ligated. In a minority of cases, it will branch from the superior mesenteric artery, superior to the ileocolic pedicle, and will need ligation. Distal in its course, near the ileocecal junction, the ileocolic artery becomes the ileal branch (and accessory ileal branch), which can bleed if injured. Therefore, the dissection of the ileocolic artery should start in the avascular plane between the superior mesenteric vessels and the ileal branch.
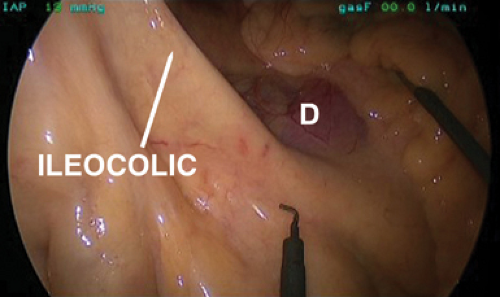 Figure 3.2 The ileocolic pedicle identified through the right colon mesentery. The duodenum (D) should be identified, and the pedicle should travel clearly to the ileocecal junction. |
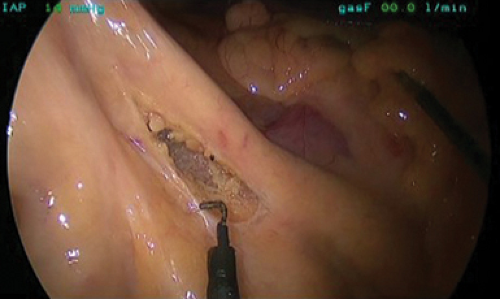
A wide window is made in the peritoneum inferior to the ileocolic pedicle as the retroperitoneal structures are gently swept away in a posterior direction (Fig. 3.3). A mesenteric window is then made on the superior aspect of the ileocolic pedicle, and the pedicle should be isolated adequately to allow for easy vessel division. The surgeon should clearly identify the duodenum to avoid injury (Fig. 3.4).
The division of the ileocolic pedicle can be performed using vessel sealing energy devices, laparoscopic staplers, or clips. The level of division of this vessel will depend on the surgical indication. For malignancy, this pedicle should be proximally divided so as to maximize the lymph node harvest (Fig. 3.5). In cases of Crohn’s disease where the mesentery may be thickened, the vessel is divided where it is soft (usually more proximal than distal).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree