Fig. 15.1
Incision and drainage of an acute pilonidal abscess. An incision is made parallel to the midline at least 1 cm laterally. A small ellipse of skin is removed to prevent the wound edges from sealing and the abscess reforming. Packing is avoided
Packing the wound is avoided as it interferes with drainage and healing.
Sitz baths or a handheld shower is used two to three times daily to clean the wound.
Antibiotics are only necessary in patients with diabetes, prosthetic implants, diseases leading to the patient being immunocompromised, and significant cellulitis.
Wound checks are done every 1–2 weeks and include shaving all hair within 2 in. of the entire gluteal cleft (on both sides of the gluteal cleft for 2 in.).
After healing, recurrence occurs in 50 % and presents as another abscess or a chronic pilonidal sinus.
Chronic Pilonidal Sinus
Chronic pilonidal sinuses have no acute inflammation and may have primary and secondary visualized openings. The sinus tract connects the openings.
Treatment is nonoperative or operative depending on the patient’s preference and extent of disease.
Nonsurgical Approach
Hair Removal
Shaving alone has been advocated as an alternative to surgery. Though studies looking at shaving have demonstrated healing, but flaws exist in these studies. Shaving can improve rates of pilonidal sinus healing.
Hair removal may be an effective therapy in chronic pilonidal sinus disease, but the duration of shaving to prevent recurrence is unknown. Shaving should be continued at least until complete healing has occurred.
Laser depilation of the natal cleft may also aid in healing a pilonidal sinus.
Surgical Approaches
Many approaches have been advocated when performing surgery for pilonidal disease including incisional and excisional, with or without primary closure of the resultant wound.
Wide excisional techniques have fallen out of favor, and minimal surgical procedures are preferred.
Midline Excision
The most common operation is midline en bloc excision with or without primary closure of the entire sinus.
Studies suggest that excision with primary closure decreases healing time; however, closing the wound may lead to increased wound complications and recurrence of the pilonidal disease. Prophylactic antibiotics are not necessary.
Compared to past recommendations, limited excision is currently favored as it creates smaller wounds.
Unroofing and Secondary Healing
Unroofing the sinus and curettage leaves a smaller wound. Unroofing is associated with half the healing time of wound excision, but still requires dressing changes and wound care.
Marsupialization of the skin edges to the fibrous tract may decrease the wound surface.
Hair removal is an important adjunct for healing.
Bascom’s Chronic Abscess Curettage and Midline Pit Excision (Bascom I)
The Bascom technique focuses on changing the conditions of the gluteal cleft versus excising a large amount of normal tissue in the diseased area (Fig. 15.2a–b).
Fig. 15.2
The Bascom procedure: (a) A generous vertically oriented incision is made through the abscess cavity 1 cm off the midline. The wound is curettaged to remove the hair and debris. The fibrous sinus tract or abscess wall is left in place. The connecting tracts to the midline pits are identified, and the overlying skin is undermined so that they drain to the site of the incision. The midline pits are excised using a small diamond-shaped incision to remove each of them. (b) The undermined flap of skin is tacked down and the pit excision sites closed
Meticulous shaving is performed weekly either at the doctor’s office or by a trained family member or friend until the wound is healed.
Karydakis Procedure (Advancing Flap; Fig. 15.3)
Fig. 15.3
The Karydakis procedure. The upper portion of the figure illustrates the elliptical incision that is parallel and 1 cm from the midline. The skin and gluteal fat containing the pilonidal sinus is excised down to the sacral fascia. The lower portion of the figure shows that the subcutaneous flap which is mobilized such that it can be advanced across the midline to the opposite side. The flap is sutured to the sacral fascia and the skin is closed. The incision will be lateral to the cleft
A drain is always placed at the upper end of the wound for 2–3 days. Antibiotics are not routinely used.
The goals as shown in Fig. 15.3 involve eccentrically excising the diseased midline tissue. The surgical wound is laterally displaced out of the midline gluteal cleft.
Studies show that this procedure is successful with a low complication and recurrence rate. This procedure should be considered for recurrent or complex cases.
Recurrent or Complex Pilonidal Sinus
Patients who have failed conservative measures or standard surgical procedures may require excision of the pilonidal sinus combined with a flap closure and modification of the midline natal cleft.
Surgical Approaches
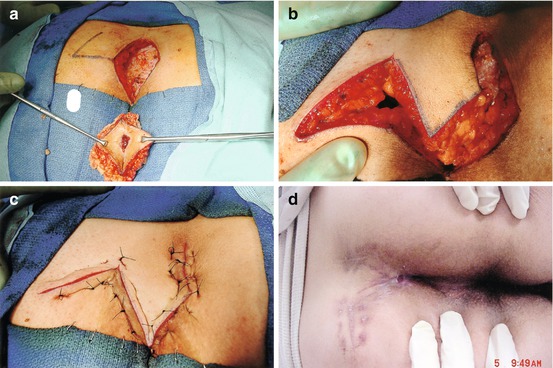
Rhomboid Flap
The rhomboid flap (also called Limberg) is a cutaneous rotational flap used to fill the soft tissue defect (Fig. 15.4a–d).