Chapter 30 Pelvic Ultrasonography and Sonohysterography
INTRODUCTION
Ultrasonography is an invaluable diagnostic tool for the assessment of uterine and pelvic pathology.1 The use of both transabdominal and transvaginal ultrasonography has become widespread because it is a safe, noninvasive, and readily available tool in the office setting. For evaluation of uterine cavity abnormalities, the diagnostic accuracy of ultrasonography is improved considerably by injecting normal saline solution into the uterine cavity during a procedure referred to as sonohysterography. For many conditions and complaints, ultrasonography has become one of the standard first steps in the diagnostic evaluation.
PRINCIPLES OF ULTRASONOGRAPHY
Ultrasound Equipment Parameters
Ultrasound Modes
A recent technologic advance, termed three-dimensional (3D) ultrasonography, uses computer software to combine multiple B-mode images in successive planes into a three-dimensional image that displays volume. If multiple volume images are shown in rapid succession, a motion video is obtained, which is sometimes referred to as 4D ultrasonography, because it shows three dimensions over time.2
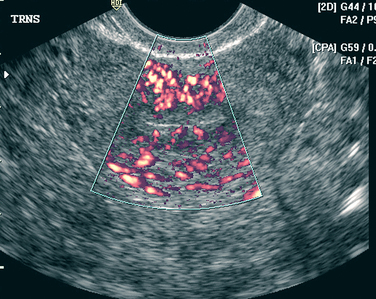
An additional ultrasound approach used clinically is termed color flow Doppler ultrasonography. For this approach, a standard B-mode image is overlaid with colors derived from Doppler sounds, which represent the speed and direction of blood flowing through vessels (Fig. 30-1).
Frequency
Ultrasound frequencies used in gynecology can range from 1.6 to 10 MHz but are more commonly between 3 and 7.5 MHz. These frequencies are much higher than audible sound frequencies, which are less than 20,000 Hz. For ultrasound, lower frequency sound waves are better able to penetrate the body’s tissues more deeply.3 Conversely, higher frequency sound waves give better resolution but penetrate tissue less deeply.
The frequency of most ultrasound probes can be automatically changed by adjusting the depth of the focal zone corresponding to the structure being studied. Ideally, the highest frequency that can penetrate the depth to be studied should be utilized.4
Dynamic Range
Dynamic range is the range between the weakest and the strongest echoes displayed and is expressed in decibels (dB). A broad dynamic range results in the most favorable image characteristics. To minimize artifacts, the dynamic range should be set lower for cystic structures and higher for solid structures.5
APPROACHES
Ultrasonography Versus Sonohysterography
Transvaginal ultrasonography is the first step in evaluating the uterus, ovaries, and tubes. When a symmetric and regular endometrial stripe can be clearly imaged, the uterine cavity can be determined to be normal and endometrial thickness can be accurately determined. In contrast, when the endometrial stripe is irregular or poorly delineated, transvaginal ultrasonography alone has limited usefulness in evaluating the nature and location of endometrial cavity pathology.6–10 In these cases, sonohysterography greatly enhances the ability to visualize lesions that project into the uterine cavity.
Sonohysterography enhances the diagnostic accuracy of transvaginal ultrasonography by filling the endometrial cavity with fluid (usually normal saline solution) via a transcervical catheter.11 First described by Nannini in 1981 as echohysteroscopy, this technique is also referred to as saline infusion sonography.12 Sonohysterography is a simple, accurate way to detect intrauterine masses that will ultimately be evaluated histologically to differentiate endometrial polyps, submucosal leiomyomas, and endometrial carcinoma.13 This technique has several advantages over X-ray hysterosalpingography, including less pain, less cost, and no exposure to ionizing radiation.
INDICATIONS
Transvaginal ultrasound with or without sonohysterography is often one of the first diagnostic steps in the evaluation of a wide spectrum of gynecologic and obstetric conditions that can result from or cause anatomic alterations of the reproductive organs (Table 30-1). The excellent diagnostic accuracy, minimal invasiveness, and relative cost-effectiveness of these techniques have led to their widespread acceptance.
Table 30-1 Clinical Indications for Ultrasonography and Sonohysterography
| Ultrasonography | Sonohysterography | |
|---|---|---|
| Pelvic mass | X | |
| Pelvic pain | X | |
| Pelvic inflammatory disease | X | |
| Lost intrauterine device | X | |
| Infertility | X | X |
| Recurrent pregnancy loss | X | X |
| Abnormal uterine bleeding | X | X |
| To evaluate indistinct endometrium | X | |
| To evaluate thickened endometrium | X | |
| To monitor tamoxifen therapy | X | |
| To predict depth of endometrial cancer invasion | X | |
| Uterine leiomyomata | ||
| Intramural and pedunculated | X | |
| Submucosal and intracavitary | X | |
| Intraoperative sonohysterography | X | |
| To disperse intrauterine adhesions | X | |
Pelvic Mass
Ovarian Masses: Functional, Benign, or Malignant
Certain sonographic characteristics have been found to be strongly associated with malignancy. An ovarian mass is more likely to be malignant when ultrasonography reveals:
These criteria are used in combination with measurements of serum CA 125 for the risk of malignancy index.14 For indeterminate cases, color flow Doppler ultrasonography may also be helpful. It has been demonstrated that ovarian malignancy is more likely if a solid element of the mass demonstrates central blood flow.15
Ovarian Torsion
The sonographic findings for ovarian torsion include a cystic, solid, or complex mass that is frequently found in the midline superior to the uterus.16 This mass, which represents an enlarged ovary, will often have cystic follicles visible along the periphery and a markedly thickened wall. Increased peritoneal fluid is common.
Uterine Leiomyomas
Uterine leiomyomas are the most common indication for hysterectomy in the United States. Although approximately 25% of women will have symptomatic uterine leiomyomas, the cumulative incidence of leiomyomas by age 50 is nearly 70% for white women and more than 80% for black women.17
The classic sonographic appearance of a uterine leiomyoma is a spherical hypoechoic or hyperechoic area contiguous with the uterine wall.18 In some cases, calcification of leiomyomas results in irregular high-amplitude echoes. In many cases, it is difficult with transvaginal ultrasonography alone to determine whether a leiomyoma is intramural, submucosal, or intracavitary in location.
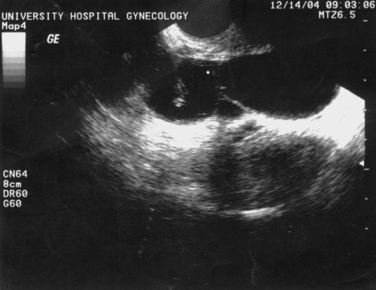
Sonohysterography can accurately identify the size, location, and depth of uterine leiomyomata (Fig. 30-2).19 This information helps predict surgical resectability, the best access for surgery (abdominal versus hysteroscopic), and the duration of surgery.
For surgical planning, uterine leiomyomas are classified into three types:
Class 3 leiomyomas are the least amenable to successful resection and are associated with significantly more complications, including uterine perforation, fluid overload, and incomplete resection.20
Pelvic Pain
Pelvic pain is a common gynecologic complaint, accounting for 10% of gynecologic office visits, 40% of laparoscopies, and 15% of hysterectomies in the Untied States.21 Ultrasonography is an important part of the initial workup for patients who present with pelvic pain to identify anatomic causes. In nonpregnant women, ultrasonography can sometimes identify causes, such as hemorrhagic ovarian cysts, ovarian torsion, tubo-ovarian abscesses, or degenerating uterine leiomyoma.
Pelvic Inflammatory Disease
Pelvic ultrasonography can be extremely helpful for the evaluation of women with a clinical diagnosis of pelvic inflammatory disease.22 In most patients, ultrasonography will be normal, because normal and inflamed fallopian tubes are not sonographically distinct. Some patients will have acute or chronic abnormalities that are sonographically visible, such as a pyosalpinx, hydrosalpinx, tubo-ovarian abscess, or tubo-ovarian complex (Fig. 30-3).
Abnormal Uterine Bleeding
Premenopausal Women
Transvaginal ultrasonography is a useful diagnostic test in the premenopausal woman who presents with abnormal bleeding. The vast majority of premenopausal bleeding is the result of anovulatory uterine bleeding. Other common causes include submucosal leiomyoma and endometrial polyps, which can be detected by ultrasonography with sensitivity of approximately 94% and 80%, respectively.23 In women with abnormal bleeding after an abortion or delivery, ultrasonography can sometimes determine the cause of abnormal bleeding to be retained products of conception.24,25 Endometrial cancer is an uncommon cause of bleeding in women younger than age 40.
Endometrial thickness is not very discriminatory in premenopausal women. This is in contrast to postmenopausal women, in whom endometrial thickness greater than 5mm is cause for concern. During a normal menstrual cycle, endometrial thickness normally varies from 5 to 12mm.26,27 Sonohysterography can be extremely helpful in these cases.
Postmenopausal Women
Evaluation of abnormal uterine bleeding in postmenopausal women is extremely important to exclude endometrial cancer, because almost 10% will ultimately be found to have a malignancy.28 Endometrial cancer occurs in 1 to 2 per 1000 postmenopausal women per year and is one of the most common cancers in the female, exceeded in frequency only by cancers of the breast, colon, and lung. Thus, all postmenopausal women with abnormal uterine bleeding should undergo a thorough evaluation.
Evaluation of Abnormal Uterine Bleeding
Suction sampling devices are useful for detecting global disease but frequently are inadequate for detecting disease localized to a focal area or a polyp. Studies demonstrate that 15% or less of the endometrial cavity is sampled using suction devices.29 Although sampling with a suction device will provide adequate tissue for pathologic evaluation in as many as 97% of cases, carcinoma confined to endometrial polyps and localized tumors will be missed more than 15% of the time.30 For this reason, many clinicians advocate sonographic evaluation of the endometrium before endometrial biopsy to exclude focal lesions.
Ultrasonography Versus Sonohysterography
Ultrasonography and sonohysterography are sensitive noninvasive methods for detecting focal intrauterine lesions, which usually indicate carcinoma, hyperplasia, polyps, and submucosal uterine fibroids.31–36 The incidence of polyps and submucosal uterine fibroids in symptomatic premenopausal women is 33% and 21%, respectively.37 If ultrasonography or sonohysterography reveals a focal lesion, this should be evaluated with a hysteroscopy/D&C rather than with a blind endometrial biopsy, because ultrasonography cannot accurately identify the nature of the lesion.
Several studies have suggested that in postmenopausal women, endometrial thickness up to 5 mm makes endometrial pathology (i.e., endometrial hyperplasia or carcinoma) extremely unlikely, and some clinicians will therefore omit an endometrial biopsy.38 This cutoff is only useful in postmenopausal women who are not taking postmenopausal hormones such as estrogen or tamoxifen. It is also important to remember that using sonographic thickness of the endometrium to exclude endometrial carcinoma in postmenopausal women with bleeding is not 100% accurate regardless of the cutoff used.
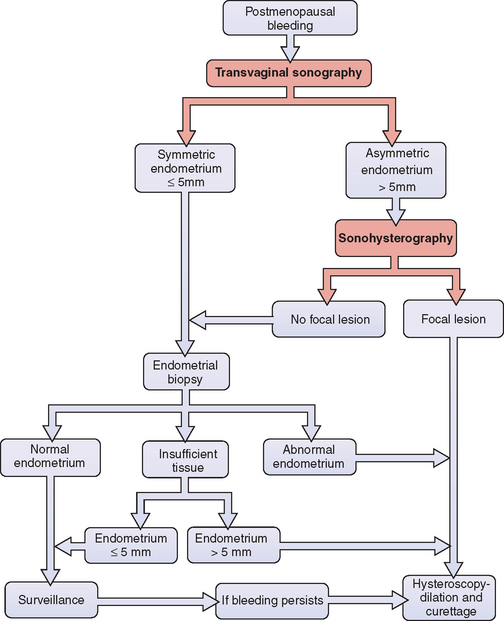
How accurate is endometrial thickness in predicting carcinoma? Meta-analyses indicated that carcinoma will be found in approximately one third of postmenopausal women with bleeding whose endometrial thickness is greater than 5mm.39 When the endometrium is equal to or less than 5mm, only 2% to 7% will subsequently be found to have carcinoma.39,40 Reducing the cutoff to 4mm will decrease the risk of carcinoma to 1.2%.41 Because endometrial carcinoma is a curable disease when discovered early, most clinicians will perform an initial endometrial biopsy in postmenopausal women with bleeding, regardless of endometrial thickness (Fig. 30-4). If the biopsy of a patient with an endometrial thickness of 5mm or less returns as “quantity not sufficient for diagnosis,” continued surveillance is a reasonable approach.
Sonohysterography
Sonohysterography is much more effective than transvaginal ultrasound alone to detect endometrial pathology in women with abnormal uterine bleeding and thickened endometrium. In addition to clearly demonstrating the location of intracavitary lesions, sonohysterography allows for differentiation of isolated submucosal defects from more diffuse endometrial thickening.19,42–44 One study of 199 postmenopausal women with abnormal bleeding found that whereas only 7% were found to have endometrial abnormalities on transvaginal ultrasound, more than 34% had abnormalities detected by sonohysterogram.45
In the past, the initial step in the evaluation of a woman with postmenopausal bleeding was an office endometrial biopsy. However, this procedure is notoriously inaccurate in the presence of focal endometrial pathology. In one study, 148 postmenopausal women with abnormal bleeding underwent aspiration endometrial biopsy, followed by sonohysterography whenever the endometrial thickness was greater than 5mm.46 Sonohysterography discovered 45 focal lesions in 81 women, 5 of which were determined to be malignancies by hysteroscopy. The initial endometrial biopsy missed 41 of these focal lesions and 3 of the 5 malignancies. The take-home message is that a blind endometrial biopsy should be avoided in women determined to have focal lesions because they often miss the pathology.
Sonohysterography is as accurate as hysteroscopy for the detection of focally growing lesions, with sensitivities for both of approximately 96%.47 However, neither modality can reliably discriminate between benign and malignant focal lesions. For this reason, histologic tissue evaluation is required whenever intrauterine pathology is discovered.
The evaluation of postmenopausal women with abnormal bleeding should utilize a combination of transvaginal ultrasonography, sonohysterography, or office endometrial biopsy when indicated, and hysteroscopy for women found to have focal lesions or abnormal biopsies (see Fig. 30-4). Utilizing ultrasonography before endometrial biopsy will avoid this uncomfortable test in women found to have focal lesions because they require a directed biopsy instead. This combination of sonohysterography and endometrial biopsy has been found to have a sensitivity of 97%, a specificity of 70%, a positive predictive value of 82%, and a negative predictive value of 94%.46
Breast Cancer Patients Receiving Tamoxifen
Tamoxifen, a selective estrogen receptor modulator, is a commonly used adjunctive therapy for women with breast cancer. Although tamoxifen acts as an estrogen antagonist in the breast, it acts as an estrogen agonist in the genital tract and is associated with endometrial hyperplasia and carcinoma. Patients taking tamoxifen have a 27% risk of developing endometrial polyps, a 9% risk of endometrial hyperplasia, and a rate of endometrial cancer two to three times higher than that of age-matched women.48,49
Neither transvaginal ultrasonography nor sonohysterography are effective screening tools in women using tamoxifen because of tamoxifen-induced subepithelial stromal hypertrophy.50–52 As a result of this abnormality, there is a poor correlation between ultrasonographic measurements of endometrial thickness and abnormal endometrial proliferation or endometrial carcinoma.53–55 Women taking tamoxifen should be monitored for symptoms of endometrial hyperplasia or cancer (e.g., abnormal uterine bleeding) and undergo a gynecologic examination at least yearly.56 However, because ultrasonographic screening has not been found to be effective, it is not recommended.
When a women taking tamoxifen experiences abnormal uterine bleeding, sonohysterography appears to be the most appropriate next step.57 Surgery can be avoided in approximately 14% of women who will be found to have normal endometrium with or without subendothelial cysts. The remainder of women will have focal lesions and should undergo hysteroscopically directed biopsies, because a blind endometrial biopsy in the office will often miss lesions.57
Screening of Asymptomatic Women
Premenopausal Women
Some clinicians recommend screening asymptomatic women with transvaginal ultrasonography, sonohysterography, or endometrial biopsy.58 One study found that approximately 10% of asymptomatic premenopausal women have uterine polyps and 1% have intracavitary fibroids, compared to 33% and 21% of symptomatic women, respectively.59 However, it is uncertain how much of this pathology is actually associated with health risks and how much will regress spontaneously.60 The concern is that such screening is likely to lead to some unnecessary surgical intervention. Until more information is available, universal screening is not recommended.61
Postmenopausal Women
Transvaginal ultrasound has not been shown to be a useful screening test in asymptomatic postmenopausal women regardless of their use of hormone treatment. One study reported that more than 35% of asymptomatic postmenopausal women have focal endometrial pathology by sonohysterography.45 Although the incidence of endometrial pathology in postmenopausal women with bleeding is relatively high, the incidence of life-threatening focal endometrial lesions in asymptomatic women is likely to be low.61 More importantly, the discriminatory value of endometrial thickness is lost in these asymptomatic women. One study of 448 postmenopausal women, half of whom were receiving estrogen replacement therapy, found that although endometrial thickness less than 5 mm was highly predictive of normal endometrium (negative predictive value, 99%), endometrial thickness greater than 5 mm was unlikely to indicate pathology (positive predictive value, 9%).60 A study of 1926 asymptomatic postmenopausal women showed similar results using a 6 mm threshold for endometrial thickness.63 Screening asymptomatic postmenopausal women is not currently recommended.
Endometrial Carcinoma
Detecting Endometrial Carcinoma
Sonography and sonohysterography can detect abnormalities of the endometrium but cannot accurately distinguish between malignant and benign lesions. With transvaginal ultrasonography, endometrial carcinoma usually appears to be either diffusely or partially echogenic. With sonohysterography, endometrial carcinoma appears as irregularly thickened endometrium or a discrete mass, but is indistinguishable from endometrial hyperplasia.11,42 A poorly distensible endometrial cavity noted during sonohysterography can be a sign of endometrial cancer.64 In the case of polyps, Doppler flow ultrasonography is of little help in distinguishing between the majority of benign polyps and those that are malignant.65
Predicting Depth of Invasion
Histology, tumor grade, depth of myometrial invasion, and tumor size are well known prognostic factors for lymph node metastasis by endometrial cancer but are difficult to predict preoperatively.66,67 Magnetic resonance imaging is effective in predicting the depth of myometrial invasion and endometrial cancer tumor size but is expensive and is not universally available. An alternative approach is sonohysterography to determine the depth of endometrial invasion; patients with deeply invasive disease can be referred to a gynecologic oncologist.
After endometrial carcinoma has been diagnosed histologically on biopsy, sonohysterography has been suggested as a way to accurately determine the degree of myometrial invasion.68 In a small study of 19 endometrial adenocarcinoma patients, sonohysterography performed before hysterectomy was able to predict the exact depth of myometrial invasion in 15 (94%) cases, suggesting a potential role for this technique in preoperative staging of endometrial carcinoma. More studies are necessary before widespread application of this approach.
Risk of Disbursing Malignant Cells
There is a concern that procedures that distend the uterus with fluid media (i.e., hysteroscopy, hysterosalpingography, and sonohysterography) could flush malignant endometrial cells into uterine vessels or through the tubes into the peritoneal cavity, thus adversely affecting the prognosis for patients with endometrial carcinoma. One study of hysterograms in patients with endometrial cancer found no correlation between intravasation of contrast medium into lymphatics and veins and subsequent 5-year survival rates.69 A sonohysterogram study of women with stage I endometrial carcinoma showed that infusion of 10 to 20mL of saline solution resulted in saline spillage from the fallopian tubes in 5 of 14 patients; in 1 patient this fluid contained malignant cells.70 These findings suggest that sonohysterography might have a small risk of cancer dissemination, although the prognostic significance of flushing endometrial cancer cells in the peritoneal cavity remains uncertain. Additional studies are warranted.
Infertility and Recurrent Pregnancy Loss
Initial Evaluation
Transvaginal ultrasonography, with sonohysterography when indicated, is a useful diagnostic procedure for the initial evaluation of infertile patients.71 Congenital and acquired uterine pathology is present in up to 10% of infertile couples and 15% to 55% of those with recurrent pregnancy loss. Pathologic conditions of the uterus that can be detected with ultrasonography and sonohysterography include müllerian and diethylstilbestrol-related anomalies, uterine fibroids, endometrial polyps, and Asherman’s syndrome. Other fertility-related conditions that can be detected include hydrosalpinges (see Fig. 30-3) and polycystic ovaries (Fig. 30-5).
Sonohysterography can be used to thoroughly evaluate the endometrial cavity and has been shown to be as accurate as diagnostic hysteroscopy in detecting pathology. In a study of 72 infertile women, 11% were found to have cavitary lesions with both HSG and hysteroscopy; there was no statistical difference in pregnancy outcome between these two techniques for uterine evaluation.72
Recurrent Pregnancy Loss
The diagnosis and surgical correction of uterine defects associated with recurrent pregnancy loss increases the rate of full-term delivery. Anatomic disorders, including congenital müllerian anomalies and acquired defects such as uterine leiomyomata and uterine synechiae, account for 15% to 55% of recurrent pregnancy loss.73
Prior to the development of ultrasonography, HSG was the diagnostic test of choice for uterine anomalies. However, HSG is not effective in assessing the outer uterine contour, and thus cannot accurately discriminate between a septate and a bicornuate uterus.73,74 In the case of uterus didelphys with a complete vaginal septum covering one of the two cervical openings, cannulation of only one cervical canal during HSG can lead to the misdiagnosis of a unicornuate uterus.75
Transvaginal ultrasonography is more accurate than HSG in diagnosing müllerian anomalies, because it can detect structures not visible externally, such as noncommunicating uterine horns, and can determine both the internal and external contours of the uterus.76 An important function of ultrasonography is to differentiate between a uterine septum and a bicornuate uterus (Fig. 30-6). The diagnosis of bicornuate uterus is made in the presence of fundal notch deeper than 1 cm, diverging endometrial cavities, and fundal broadening of the intracavitary tissue, which is typically thick and isoechoic relative to the rest of the myometrium.77 A uterine septum is usually thinner and hypoechoic because it tends to be more fibrous. However, hypoechogenicity is not diagnostic, because the septum can contain both fibrous and muscular elements.78
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree