Gastroesophageal reflux disease (GERD) is one of the most common digestive diseases in the Western world, with typical symptoms, such as heartburn, regurgitation, or retrosternal pain, reported by 15% to 20% of the general population. The pathophysiology of GERD is multifactorial. Our understanding of these factors has significantly improved in recent years, with increased understanding of the acid pocket and hiatal hernia and how these factors interact. Although our insight has significantly increased over the past years, more studies are required to better understand symptom generation in GERD, especially in patients with therapy-resistant symptoms.
Key points
- •
The high-pressure zone at the esophagogastric junction is generated by the lower esophageal sphincter (LES) and the crural diaphragm.
- •
Transient LES relaxations are prolonged relaxations of the LES and are the main mechanism underlying gastroesophageal reflux.
- •
The acid pocket is the source of postprandial acid refluxate; the position of the acid pocket relative to the diaphragm is a major determinant of the acidity of the refluxate.
- •
Especially in patients with nonerosive reflux disease, increased permeability and dilated intercellular spaces may contribute to symptom generation.
Introduction
Although reflux of gastric contents into the esophagus is a physiologic phenomenon, increased exposure or increased perception of the refluxate may cause troublesome symptoms and/or complications, referred to as gastroesophageal reflux disease (GERD). GERD is one of the most common digestive diseases in the Western world, with typical symptoms, such as heartburn, regurgitation, or retrosternal pain, reported by 15% to 20% of the general population. Most patients have mild to moderate complaints, but increased exposure of the esophageal epithelium to noxious gastric contents may lead to complications, such as erosive esophagitis, Barrett esophagus, peptic strictures, and even esophageal carcinoma. The different phenotypes of GERD range from nonerosive reflux disease (NERD), through reflux esophagitis and Barrett esophagus; but most patients have no abnormalities on endoscopic examination. Clearly, symptoms related to GERD have to be related to reflux events. This relationship depends on the presence of pathologic acid exposure during 24-hour pH-metry and a positive association between symptoms and esophageal reflux episodes. In the absence of these features, patients are rather considered to suffer from functional heartburn, a functional disorder that does not belong to the GERD spectrum.
Given the high prevalence of GERD, understanding of the pathophysiology is of great importance in order to efficiently treat our patients. In this article, the authors review the major mechanisms involved in gastroesophageal reflux.
Introduction
Although reflux of gastric contents into the esophagus is a physiologic phenomenon, increased exposure or increased perception of the refluxate may cause troublesome symptoms and/or complications, referred to as gastroesophageal reflux disease (GERD). GERD is one of the most common digestive diseases in the Western world, with typical symptoms, such as heartburn, regurgitation, or retrosternal pain, reported by 15% to 20% of the general population. Most patients have mild to moderate complaints, but increased exposure of the esophageal epithelium to noxious gastric contents may lead to complications, such as erosive esophagitis, Barrett esophagus, peptic strictures, and even esophageal carcinoma. The different phenotypes of GERD range from nonerosive reflux disease (NERD), through reflux esophagitis and Barrett esophagus; but most patients have no abnormalities on endoscopic examination. Clearly, symptoms related to GERD have to be related to reflux events. This relationship depends on the presence of pathologic acid exposure during 24-hour pH-metry and a positive association between symptoms and esophageal reflux episodes. In the absence of these features, patients are rather considered to suffer from functional heartburn, a functional disorder that does not belong to the GERD spectrum.
Given the high prevalence of GERD, understanding of the pathophysiology is of great importance in order to efficiently treat our patients. In this article, the authors review the major mechanisms involved in gastroesophageal reflux.
The esophagogastric junction
The junction between the esophagus and stomach is a highly specialized region, composed of the lower esophageal sphincter (LES) and crural diaphragm. Together these structures have to reassure that a bolus of food can enter into the stomach. Conversely, reflux of gastric contents across the esophagogastric junction (EGJ) into the esophagus should be prevented, with the exception of a retrograde flow of gastric contents during vomiting or venting of accumulated air during belching.
The LES is a specialized thickened region of the circular muscle layer of the distal esophagus, extending over an axial distance of 3 to 4 cm. By generating a myogenic tonic resting pressure higher than the intragastric pressure, the LES provides sufficient protection against the pressure gradient between the stomach and the intrathoracic esophagus. However, during straining and inspiration, this gradient increases, requiring an additional compensatory mechanism. This task is fulfilled by the crural diaphragm, which is considered the second sphincteric component of the EGJ. The crural diaphragm forms a canal through which the esophagus enters the abdomen and is anchored to the LES by the phrenoesophageal ligament. Since the two components are anatomically superimposed, contraction of the striated muscle of the crural diaphragm during inspiration or straining exerts pressure on the LES, leading to a dynamic and powerful increase in EGJ pressure. Hence, the LES and crural diaphragm are considered the internal and external sphincter of the EGJ acting in concert to prevent gastroesophageal reflux. Under normal conditions, the EGJ fulfills this task very efficiently, except during transient LES relaxations (TLESRs) and when both sphincters (LES and crural diaphragm) are anatomically separated as in patients with a hiatal hernia.
TLESRs
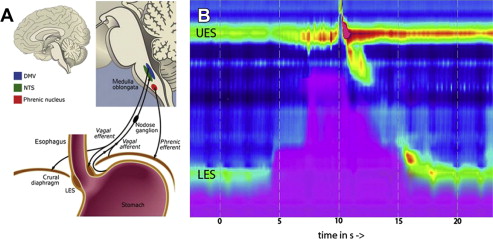
TLESRs are the predominant mechanisms underlying gastroesophageal reflux, both in normal subjects and in patients with GERD. A TLESR is a vago-vagally mediated motor pattern triggered by the activation of vagal afferents in the cardia of the stomach by various stimuli, of which gastric distension is the most important. In response to gastric distention, vagal afferents are activated triggering neurons in the dorsal motor nucleus of the vagus nerve to initiate the specific motor pattern underlying TLESRs ( Fig. 1 ). TLESRs are characterized by a rapid relaxation of the LES, esophageal shortening, and the inhibition of the crural diaphragm, thought to be the physiologic mechanism by which the stomach vents gas. The frequency of TLESRs in patients with GERD is not different from that of normal subjects. However, the occurrence of acid reflux during a TLESR is twice as high in patients with GERD, especially in those with a hiatal hernia compared with healthy controls. The potential explanation for this observation is discussed later.
Hiatal Hernia
In healthy people, the distal part of the lower esophageal sphincter is located in the abdomen and the crural diaphragm is superimposed, leading to a synergistic high pressure zone. In the presence of a hiatal hernia, the capacity of the EGJ to prevent reflux is hampered, mainly because the stomach has migrated more proximal through the diaphragmatic hiatus into the mediastinum separating the high-pressure zones of the LES and the crural diaphragm. In addition, the hiatal sac may function as a reservoir from which fluid can re-reflux into the esophagus after swallowing or during periods of low sphincter pressure.
A hiatal hernia is associated with more severe erosive esophagitis and Barrett esophagus. This increase in esophageal injury is caused by a prolonged acid exposure time, which in its turn results from a larger number of reflux episodes in patients with hiatal hernia than in those without, and a prolonged acid clearance time. In contrast to earlier thoughts, a hiatal hernia is a dynamic entity. A recent study clearly showed that a hiatal hernia can be intermittent as a result of axial movement of the LES through the diaphragmatic hiatus. Most intriguingly, the rate of reflux episodes is almost doubled when the hiatal hernia is present compared with periods when the hiatal hernia is absent, further illustrating the importance of hiatal hernia in GERD. The increase in reflux episodes in patients with a hiatal hernia is mainly explained by the observation that, in addition to TLESRs, other mechanisms come into play. Indeed, half of the reflux episodes in patients with GERD with a hiatal hernia occur during swallowing or straining. Moreover, during spatial separation, the rate of acid reflux episodes during a TLESR is doubled compared with the rate without spatial separation, most likely because of the alteration of the position of the gastric acid pocket.
Acid Pocket
Most reflux episodes occur after a meal, when the stomach is filled with food, known to trigger TLESRs. In contrast to the thought that meal ingestion buffers gastric acid, acid reflux episodes occur even in the early postprandial period. Fletcher and colleagues elegantly showed that gastric acid floats on top of the meal acting as a reservoir from which acid can enter the esophagus during episodes of opening of the EGJ. Using a gradual pull-through pH-metry, they discovered a highly acidic zone of approximately 2 cm near the EGJ in the postprandial state. This gastric acid pocket accounted for the lower pH of the refluxate compared with the gastric postprandial pH.
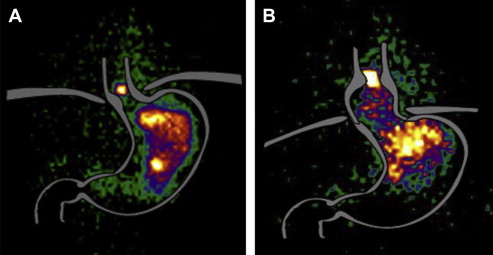
Recently, the existence of the acid pocket was confirmed using scintigraphy in both healthy subjects and patients with GERD. Patients with GERD have larger acid pockets, whereas the proximal extent of the acid pocket is closer to the LES in patients than in healthy subjects. Most importantly, Beaumont and colleagues demonstrated that the major risk factor for acid reflux is the presence of a hiatal hernia and the position of the acid pocket relative to the diaphragm ( Fig. 2 ). Clearly, if the acid pocket extends into the hiatal opening or is located above the diaphragm, the pocket is the major source of refluxate, resulting in a 5-fold increased risk of having acid reflux. Moreover, in patients with a large hiatal hernia it was demonstrated that the hiatal sac can function as a reservoir from which fluid can re-reflux into the esophagus during swallowing and straining. This finding explains the increased risk to have acidic gastroesophageal reflux during a TLESR, when the LES relaxes after swallowing or when LES pressure is low in patients with a hiatal hernia.
Prokinetic agents, such as azithromycin, increase proximal tone and promote gastric emptying. Because of this prokinetic effect, azithromycin displaces the acid pocket to a more distal location in patients with GERD with a small hiatal hernia. This more distally located acid pocket leads to less frequent postprandial acid reflux episodes compared with placebo. An alternative approach to prokinetics is the use of alginates. Alginates are natural polysaccharide polymers that, after contact with gastric acid, precipitate into a low-density viscous gel or raft of near-neutral pH in a matter of seconds. This alginate-antacid raft formed after ingestion colocalizes with the postprandial acid pocket and displaces it below the diaphragm, resulting in significant suppression of postprandial acid reflux. Hence, the acid pocket is considered an interesting target for treatment, mainly because it represents the reservoir from which reflux seems to occur.
Positive Pressure Gradient and Obesity
Retrograde flow across the EGJ requires a positive pressure gradient between the stomach and the distal esophagus. It is well accepted that abdominal straining, for example, induces reflux if the generated pressures is higher that the EGJ pressure. In line with this, ambulatory manometric recordings in patients with GERD indeed reveal that straining occurs at the onset of 31% of acid reflux episodes. Obesity, on the other hand, leads to a chronically increased pressure gradient and has been abundantly demonstrated as a risk factor for GERD. In fact, the rising prevalence of GERD has, in part, been attributed to the rapidly increasing prevalence of obesity. In a recent study, Lee and colleagues demonstrated that central obesity causes partial hiatus herniation and short-segment acid reflux, providing a plausible explanation for the high incidence of inflammation and metaplasia and occurrence of neoplasia at the EGJ. This finding explains how obesity increases the risk of reflux symptoms, prolonged esophageal acid exposure, esophagitis, and Barrett esophagus, further emphasizing that increased abdominal pressure is a pivotal mechanistic factor.
Gastric Motility
Delayed gastric emptying is observed more often in patients with GERD compared with healthy volunteers as demonstrated in a recent systematic review by Penagini and Bravi. However, a relationship between delayed gastric emptying and increased esophageal acid exposure has not been convincingly demonstrated. Moreover, dyspepsia, regurgitation, or dysphagia, symptoms associated with delayed gastric emptying, have no differentiating value in patients with GERD. Taken together, these data suggest that impaired gastric emptying is not a major factor in the pathophysiology of GERD.
Esophageal Clearance
When refluxate reaches the esophagus, clearance is mainly mediated by esophageal peristalsis, triggered by mechanoreceptors in the esophageal lumen, and gravity accounting for approximately 95%. Subsequently, salivary bicarbonate further contributes to acid clearance by neutralizing the acid and normalizing esophageal pH. Obviously, rapid clearance of acid from the esophagus is crucial because prolonged clearance is associated with the development of esophagitis and Barrett metaplasia. In line, impaired refluxate clearance caused by the supine position, a lack in secondary peristalsis, and reduced saliva production during sleep explains the increased severity of erosive esophagitis observed in cases of nocturnal reflux. Similarly, prolonged esophageal clearance in esophageal motility disorders, such as in weak or absent peristalsis, carries an increased risk to develop esophagitis and reflux symptoms.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





