The prevalence of gastroesophageal reflux disease (GERD) symptoms increased approximately 50% until the mid-1990s, when it plateaued. The incidence of complications related to GERD including hospitalization, esophageal strictures, esophageal adenocarcinoma, and mortality also increased during that time period, but the increase in esophageal adenocarcinoma has since slowed, and the incidence of strictures has decreased since the mid-1990s. GERD is responsible for the greatest direct costs in the United States of any gastrointestinal disease, and most of those expenditures are for pharmacotherapy. Risk factors for GERD include obesity, poor diet, lack of physical activity, consumption of tobacco and alcohol, and respiratory diseases.
Key points
- •
Frequent GERD symptoms are encountered in 20% of North Americans.
- •
The prevalence of GERD symptoms rose, and then plateaued in the mid-1990s.
- •
GERD incurs the highest annual direct costs of all digestive diseases in the United States.
- •
Pharmaceutical cost is responsible for most of the direct cost of GERD management.
- •
Risk factors for GERD include obesity, poor diet, lack of leisure physical activity, consumption of tobacco and alcohol, and respiratory disease.
Introduction
Gastroesophageal reflux disease (GERD) is a condition that develops when the reflux of gastric contents causes troublesome symptoms or complications. GERD is responsible for some of the most common symptoms leading to presentation for medical care. The prevalence of GERD symptoms and the incidence of some of its complications have risen strikingly over the last few decades, leading to substantial economic impact. There are several potential explanations for these rising trends.
Introduction
Gastroesophageal reflux disease (GERD) is a condition that develops when the reflux of gastric contents causes troublesome symptoms or complications. GERD is responsible for some of the most common symptoms leading to presentation for medical care. The prevalence of GERD symptoms and the incidence of some of its complications have risen strikingly over the last few decades, leading to substantial economic impact. There are several potential explanations for these rising trends.
Trends in the prevalence of GERD and incidence of its complications
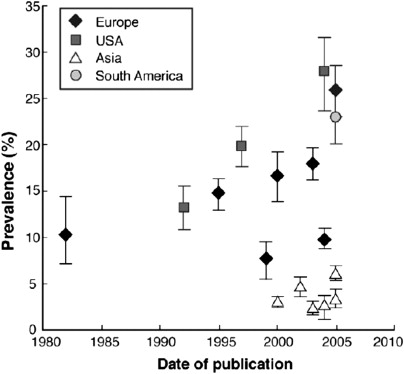
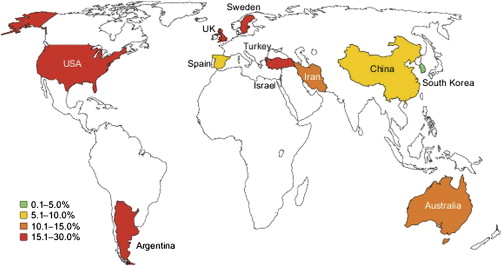
Symptoms of GERD seem to be more common now than 25 years ago. In systematic reviews of population-based studies, El-Serag and colleagues found that the prevalence of at least weekly symptoms of GERD rose approximately 50% until 1995, and that the prevalence has remained relatively constant since then ( Fig. 1 ). The weighted-mean prevalence of at least weekly GERD symptoms is greatest in North America (19.8%), lowest in East Asia (5.2%), and intermediate in Europe and the Middle East (15.2% and 14.4%, respectively) ( Fig. 2 ). The rate of increase in the prevalence of symptoms seems to be similar across all geographic regions studied.
The source studies for that systematic review were often limited because they did not account for the use of acid-reducing medications, which would be expected to mask GERD symptoms; because the use of such medications has increased, the true prevalence of GERD (including treated and untreated) may be greater than the estimates previously mentioned. In addition, the estimates were based primarily on studies of separate samples of populations obtained at different time points. One exception is the HUNT study, which administered surveys longitudinally to the same population over time; residents of a Norwegian county answered the questions between 1995 and 1997, and the same questions again between 2006 and 2009. The prevalence of at least weekly GERD symptoms increased from 12% to 17% during that time period. GERD symptoms became more common in men and women, and in all age groups.
The incidence of complications of GERD also seems to have risen, but may have plateaued or even decreased since the mid-1990s. The proportion of hospitalizations in the US Veterans Affairs health care system with a primary or secondary discharge diagnosis of GERD increased fourfold between 1970 and 1996. Mortality directly related to GERD is very rare, but analysis of US death certificates demonstrated an increase from 1 death per 1 million individuals per year to 2.1 per 1 million between 1979 and 1992. In two community hospitals, the incidence of new esophageal strictures increased from 1986 to 1993, then decreased from 1994 to 2001, coinciding with a large increase in prescriptions for proton pump inhibitors (PPIs). In the US Veterans Affairs health care system, the incidence of new esophageal strictures decreased 12% as a proportion of all upper endoscopies from 1998 to 2003, and the 1-year incidence rate of recurrent strictures decreased 36%. Similarly, within the US Medicare system, the proportion of upper endoscopies with a stricture declined 11% between 1992 and 2000, and the incidence of recurrent strictures decreased 30%, coinciding with the introduction of PPIs.
The most feared complication of GERD is esophageal adenocarcinoma, a cancer that historically had been extremely rare. The cancer is fivefold as common in individuals with chronic GERD symptoms compared with those without GERD. In 1991, a seminal study by Blot and colleagues reported an alarming doubling of the incidence of esophageal adenocarcinoma from 1976 to 1987. The incidence of esophageal adenocarcinoma thereafter climbed to sevenfold the baseline incidence, and most recently occurs in the general US population in 2.6 per 100,000 patient-years. World-wide, the incidence of esophageal adenocarcinoma has risen in most industrialized countries where there is a majority white population. Despite the dramatic relative increase in the incidence of esophageal adenocarcinoma, it remains a rare disease in absolute terms. Indeed, even in men with chronic GERD symptoms, the incidence of colorectal cancer is likely threefold the incidence of esophageal adenocarcinoma, and women with GERD symptoms likely have an incidence of esophageal adenocarcinoma that is similar to the incidence of breast cancer in men. Furthermore, the rising incidence may be reaching a plateau, because the increase in incidence has slowed in the United States since around 1997. The plateauing of the incidence of esophageal adenocarcinoma might be in part related to the advent of PPIs.
Just as the incidence of esophageal adenocarcinoma has risen, there has been a dramatic rise in the incidence of diagnosed cases of Barrett’s esophagus, the premalignant lesion associated with esophageal adenocarcinoma. For example, in a Dutch primary care database, the incidence of newly diagnosed cases of Barrett’s esophagus rose from 11 per 100,000 patients in 1996 to 23 per 100,000 in 2003. Similarly, in a large integrated US health care system, the incidence of diagnosed cases of Barrett’s esophagus rose from 15 per 100,000 patient-years in 1998 to 24 per 100,000 in 2006. In the same population, the prevalence of diagnosed Barrett’s esophagus rose from less than 10 per 100,000 individuals in 1994 to 131 per 100,000 in 2006, with no sign of plateauing. These figures need to be interpreted with caution because estimating the changing incidence of Barrett’s esophagus is more challenging than estimating the changing incidence of esophageal adenocarcinoma. Changes in the incidence of diagnosed Barrett’s esophagus can be strongly influenced by changing patterns in the practice of upper endoscopy, both in terms of who gets referred for the procedure and which endoscopic and histologic findings are recognized as Barrett’s esophagus. Hence, the proportion of individuals with Barrett’s esophagus who are diagnosed with Barrett’s esophagus has likely been increasing over the last few decades. Indeed, population-based studies of individuals invited to undergo upper endoscopy for research indicate that the true prevalence of Barrett’s esophagus is much greater than suggested by the previously mentioned clinical studies, and at least 1300 per 100,000. Therefore, it is unclear whether the incidence of Barrett’s esophagus has truly been changing.
The economic impact of GERD
To assess the economic impact of GERD, one must consider direct and indirect costs. Direct health care costs include those incurred during office visits, diagnostic testing, treatment, and hospital admissions. Indirect costs include those from missed work because of symptoms or clinic visits, diminished productivity while at work, and impairment in performing daily activities.
Direct Health Care Costs
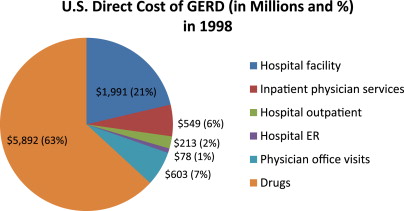
In a report using data from the late 1990s, GERD was found to be the digestive disease with the highest annual direct cost in the United States accounting for $9.3 billion. A breakdown of the components of the direct cost is shown in Fig. 3 . Pharmaceutical costs were responsible for most of the direct costs (63% or $5.9 billion). Hospital inpatient admissions ($2.5 billion), physician office visits ($603 million), hospital outpatient visits ($213 million), and hospital emergency visits ($78 million) made up the remainder of the cost. In 2004, the direct costs of GERD were estimated to be even greater ($12.1 billion).
Ambulatory care costs
When listed as a primary diagnosis, symptoms of GERD result in 4.6 million office encounters in the United States annually, and increases to 9.1 million visits annually if one includes visits in which a GERD diagnosis was listed as one of the top three diagnoses for the encounter. Ambulatory care use in the United States for GERD has been up-trending in recent decades; between 1975 and 2004, the rate of ambulatory care visits with any diagnostic listing of GERD increased approximately 2000%. GERD is the most frequently first-listed digestive system condition at ambulatory care visits, constituting 17.5% of all gastrointestinal diagnoses. Total ambulatory care costs, consisting of physician fees for office visits and any extra charges for procedures performed in offices, was estimated to be $1.4 billion in 2004. This was the second highest contributor to total ambulatory care costs from digestive diseases.
Inpatient care costs
Gastroesophageal reflux (4.4 million) was the most common gastrointestinal discharge diagnosis among any listed diagnoses from hospital admissions based on an analysis of the 2009 US Nationwide Inpatient Sample of the Healthcare Cost and Utilization Project. GERD was not commonly listed as the principal discharge diagnosis (13th digestive disease as principal discharge diagnoses) and resulted in a relatively short length of hospital stay (median, 2 days); nevertheless, primary GERD inpatient admissions were estimated to cost more than $380 million annually. GERD-related inpatient costs account for approximately 30% of all direct costs associated with GERD treatment.
Diagnostic procedure costs
Diagnosis of GERD can usually be made based on patient history or an empiric trial of acid suppression; however, diagnostic procedures are available if a clear diagnosis continues to be in question. Table 1 lists relevant procedure reimbursement ranges based on Medicare data in 2012. Nearly 7 million esophagogastroduodenoscopies (EGDs) are performed annually in the United States in adults, and 20% to 30% are performed for the indication of reflux symptoms or GERD. Using data from the Clinical Outcomes Research Initiative’s National Endoscopic Database from 2005 to 2010, Peery and colleagues reported that 23.9% of EGDs listed reflux symptoms as an indication, and 1.2% and 5.1% listed Barrett’s esophagus screening and surveillance, respectively, as indications for the procedure. Prevalence and cost information of upper endoscopies in 2009 was estimated using the Thompson Reuters MarketScan commercial (Thompson Reuters, New York, NY), Medicare, and Medicaid databases, and the total outpatient cost in the United States was found to be around $12.3 billion for upper endoscopies. Assuming only 20% of these are done for indication of GERD, the direct annual cost to society of EGDs in patients with GERD can be estimated at more than $2 billion.
| Procedure | Minimum Price (Facility) | Maximum Price (Nonfacility) |
|---|---|---|
| Diagnostic EGD | $353 | $917 |
| EGD with biopsy | $353 | $917 |
| Bravo pH | $74 | $667 |
| Ambulatory esophageal intraluminal impedance monitoring | $45 | $261 |
| Esophageal manometry | $59 | $240 |
Pharmaceutical costs
Studies have shown that pharmaceutical costs were responsible for most of the direct health care costs from GERD. In 2004, PPI sales in the United States were in excess of $10 billion and two of the top five selling drugs in the United States were PPIs. Of the 10 costliest prescription drugs from retail pharmacies for digestive diseases according to the 2004 Verispan database of retail pharmacy sales, the top five were PPIs. They constituted 50.7% of total number of prescriptions for digestive diseases and 77.3% of total costs. Pharmacotherapy for GERD includes brand-name, generic, and over-the-counter antireflux medications that rank near the top of their respective lists in terms of expenditure ( Fig. 4 ). Any effort to substantially reduce the financial burden of GERD must be aimed at reducing the costs of medical therapy.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





