CHAPTER 18
Parenteral and enteral nutrition feeding formulas
Introduction
This chapter will provide guidelines for the general use of enteral nutrition (EN) and total parenteral nutrition as a form of nutrition support (NS) in hospitalized patients. Readers are directed to the American Society for Parenteral and Enteral Nutrition (ASPEN) guidelines for more discussion of management of critically ill, severely malnourished or pediatric patients.
Indications for nutrition support
Nutrition support is indicated when patients are unable to ingest sufficient calories and nutrients for a prolonged period of time to prevent the adverse consequences of malnutrition. Unfortunately the precise definitions of “sufficient” and “prolonged” are unclear. Several studies suggest that in most noncritically ill patients, without pre-existing malnutrition, NS does not improve outcomes unless the patient has failed to meet their macronutrient needs for 7–10 days. Prior to beginning any form of NS it is necessary to calculate energy requirements and macronutrient needs. In severely malnourished patients (e.g., low body mass index, >10% weight loss) early consultation with a nutrition support service is recommended.
Energy and macronutrient requirements
Energy requirements: Many formulas exist for calculating energy expenditure. A simple estimate of total daily energy requirements in hospitalized patients can be calculated based on body mass index (BMI) (Table 18.1). Hypocaloric feeding may benefit obese patients during critical illness.
Table 18.1 Estimated energy requirements for hospitalized patients based on body mass index
| BMI (kg/m2) | Energy requirements (kcal/kg/day) |
| < 15 | 35–40 |
| 15–19 | 30–35 |
| 20–29 | 20–25 |
| >30 | 15–20* |
| These values are recommended for critically-ill patients and all obese patients; add 20% of total calories in estimating energy requirements in noncritically-ill patients. | |
| *The lower range within each BMI category should be considered in insulin-resistant or critically ill patients to decrease the risk of hyperglycemia and infection associated with overfeeding. | |
| Source: Adapted from Klein (2002). Reproduced with permission of Elsevier. | |
Protein
Human proteins are composed of amino acids, which may be divided into essential, non-essential or conditionally-essential amino acids. 15–20% of total protein requirements should be in the form of essential amino acids. Individual protein requirements are affected by several factors, such as the amount of nonprotein calories provided, exogenous losses (e.g., chylothorax, surgical drains) and nutritional status. In patients with output from drains, the protein content of the fluid should be measured. Protein needs are affected by caloric supply, and during hypocaloric feeding, generous amounts of protein (≥2.0–2.5g/kg ideal body weight/day) are needed. Protein requirements for several clinical conditions are summarized in Table 18.2.
Table 18.2 Recommended daily protein intake
| Protein requirements | |
| Clinical condition | (grams / kg IBW/day) |
| Normal | 0.75 |
| Metabolic “stress” | 1.0–1.5 |
| Hemodialysis | 1.2–1.4 |
| Peritoneal dialysis | 1.3–1.5 |
| Continuous dialysis | 1.7–2.0 |
| IBW=ideal body weight. Males: 50 kg + 2.3 kg for each inch over 5 feet. Females: 45.5 kg + 2.3 kg for each inch over 5 feet. | |
| Additional protein requirements are needed to compensate for excess protein loss in specific patient populations, such as patients with burn injuries, external drains and protein-losing enteropathy or nephropathy. Lower protein intake may be necessary in patients with chronic renal insufficiency not treated by dialysis. | |
| Source: Adapted from Klein (2002). Reproduced with permission of Elsevier. | |
Carbohydrate
There is no dietary requirement for carbohydrate because glucose can be synthesized from precursors including amino acids. Patients with liver or renal failure may require intravenous carbohydrate during prolonged fasting or metabolic stress to prevent hypoglycemia.
Lipids
Dietary lipids are composed mainly of triglycerides: long-chain triglycerides (LCTs), which contain fatty acids that are > 12 carbons in length, or medium-chain triglycerides (MCTs), which are 6 to 12 carbons in length.
Linoleic acid (C18:2, n-6) should constitute at least 2% and linolenic acid (C18:3, n-6,9, 12) at least 0.5% of the daily caloric intake to prevent essential fatty-acid deficiency (EFAD). The plasma pattern of increased triene-tetraene ratio (>0.4) can be used to detect EFAD.
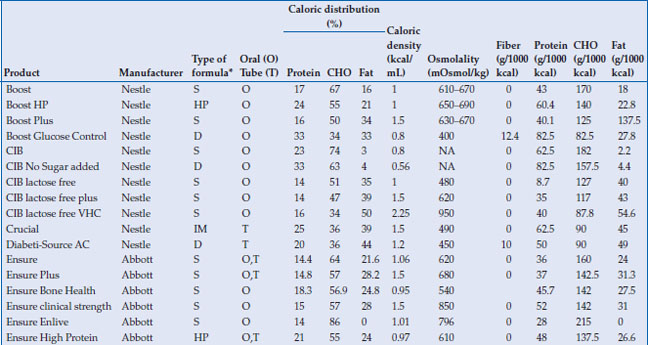
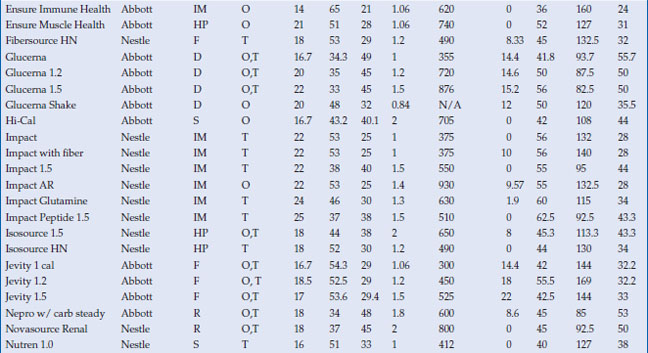
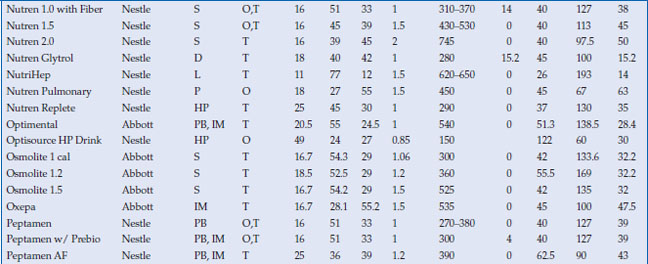
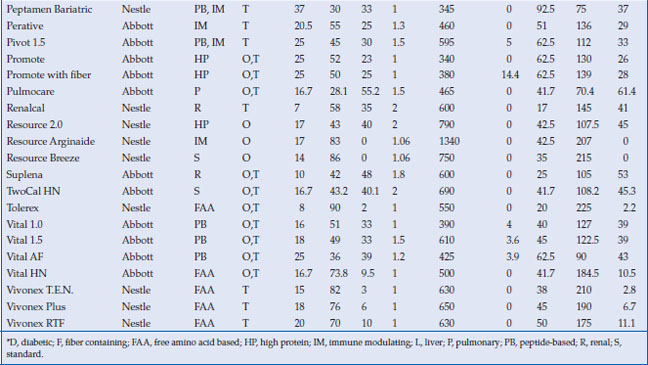
Enteral liquid feeding formulations
Formulas can be divided into four general categories: elemental formulas, semi-elemental formulas, intact-protein (polymeric) formulas, and disease-specific formulas (Table 18.3). Formula choice should be based on nutrient requirements and tolerance.
Table 18.3 Standard enteral feeding formulas
Elemental formulas
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






