Parastomal Repair: Open Techniques
Terry C. Hicks
The Background Paragraph
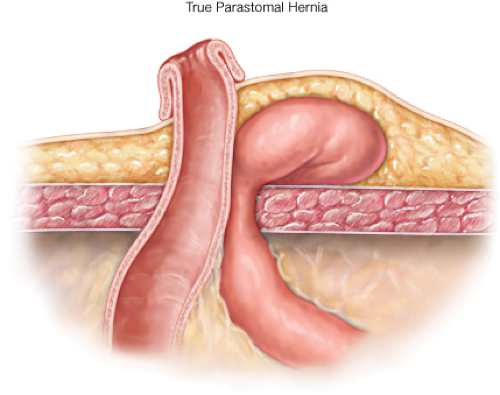
Parastomal hernia describes a hernia beside a stoma, which may be clinically diagnosed by palpating a bulge adjacent to the stoma and confirmed by CT scan, which demonstrates intraabdominal contents protruding along an ostomy (1).
Absolute indications for Parastomal hernia repair include patients with obstruction or incarceration with strangulation. Relative indications for repair include difficulty with appliance management, pain, cosmesis, and patients who have difficulty with irrigation. Multiple risk factors associated with the development of parastomal hernias have been identified. Patient specific factors include obesity, advanced age, malnutrition, chronic respiratory disorders that are associated with increased intra-abdominal pressure, immunosuppression, and wound infection. Other suggested factors include stoma placement outside the rectus muscle and creation of an excessively large fascial opening.
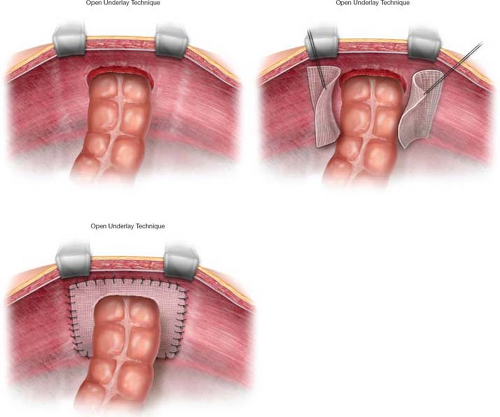
Open techniques for parastomal hernia repair include direct local tissue repair, relocating the intestinal stoma with the closure of the primary aperture, and application of prosthetic material around the stoma at different levels upon or within the abdominal wall. This chapter will discuss these three open surgical approaches.
Once the patient has completed an appropriate preoperative medical clearance, consideration should be given to a standard bowel preparation. Although recent literature has suggested that standard bowel prep is not mandatory, it is the author’s preference as the cleansed colon is technically easier to manipulate when it does not have a significant
fecal load. For those patients who can tolerate an oral preparation, an iso-osmotic lavage prep is suggested (polyethylene glycol solution). An appropriate broad-spectrum antibiotic should be administered intravenously, within 1 hour prior to the initial incision. As with other abdominal operations, routine venous thrombosis prophylaxis is utilized. The consent form should include information concerning the utilization of prosthetic materials in the management of the repair, as well as a clear discussion of alternatives, and reasonable clinical expectations.
fecal load. For those patients who can tolerate an oral preparation, an iso-osmotic lavage prep is suggested (polyethylene glycol solution). An appropriate broad-spectrum antibiotic should be administered intravenously, within 1 hour prior to the initial incision. As with other abdominal operations, routine venous thrombosis prophylaxis is utilized. The consent form should include information concerning the utilization of prosthetic materials in the management of the repair, as well as a clear discussion of alternatives, and reasonable clinical expectations.
After adequate general anesthesia has been obtained, the patient is placed in the lithotomy or supine position with the extremities appropriately padded. The utilization of an oral gastric tube and urinary bladder catheter are routine. The patient may need some rotational adjustment to provide the best exposure to the ostomy site.
Operative Technique
Direct Fascial Repair
An arched incision is made through the skin around the hernia site. With careful retraction, the hernia sac is excised, the contents reduced, and the peritoneum suture closed. The edges of the fascial defect are then approximated with a series of interrupted, nonabsorbable sutures to reduce the opening to two finger breadths. The subcutaneous space may be drained if there is more than a small amount of bleeding during the procedure (Figs. 44.1 and 44.2).
Relocation of Stoma
Preoperative marking of a new stoma site in another abdominal quadrant is important. This is usually the side opposite to the current site. After skin preparation and patient positioning, the existing ostomy is carefully isolated from the abdominal wall, and the stomal lumen is sutured closed or stapled to prevent any contamination of the field.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree