Chapter 59 Pancreatic cancer
Duodenal adenocarcinomas
Overview
The first case of duodenal adenocarcinoma was described by Hamburger in 1746 (Hamburger, 1775). In the United States, approximately 5000 patients are diagnosed with small bowel cancer every year, and 1000 of them have duodenal adenocarcinoma (Howe et al, 1999). Duodenal adenocarcinomas are rare tumors that account for approximately 0.3% of all gastrointestinal (GI) malignancies (Spira et al, 1977). Despite the duodenum representing only about 10% of the length of the small bowel, duodenal adenocarcinomas comprise 25% to 45% of small bowel tumors (Alwmark et al, 1980; Sohn et al, 1998); up to half occur near the ampulla of Vater, which explains why some studies group them with other periampullary cancers (Joesting et al, 1981). The incidence of small bowel cancers is estimated to be 1.4 per 100,000, with duodenal adenocarcinoma in approximately 0.17 per 100,000 (DiSario et al, 1994). Other malignant tumors such as carcinoid, gastrointestinal (GI) stromal tumor, lymphoma, and sarcoma can also occur in the duodenum but are far less common there than in the rest of the small intestine.
Presentation
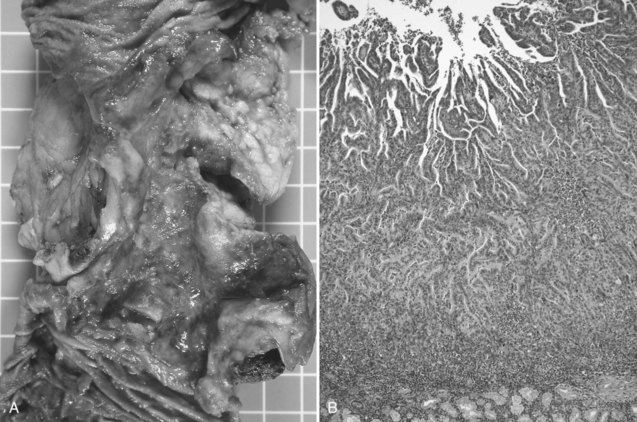
Duodenal adenocarcinoma has a slight male predominance. The median age at presentation is in the sixth and seventh decades of life (DiSario et al, 1994; Rose et al, 1996). Approximately half of the patients with duodenal adenocarcinoma are initially seen with symptoms of abdominal pain or gastric outlet obstruction: nausea, vomiting, early satiety, and anorexia. Duodenal cancers often present as circumferential napkin-ring type lesions (Fig. 59.1). However, patients can also be seen with bleeding, melena, or jaundice. Bauer and colleagues (1994) noted a 21% incidence of a palpable mass on physical exam. A small proportion of patients are asymptomatic; the lesion is identified during the workup of an unrelated medical problem or as a result of screening for familiar adenomatous polyposis (FAP).
Evaluation
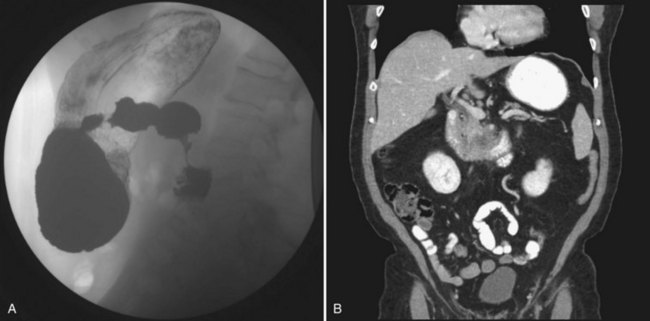
The evaluation of any duodenal mass must assess for possible metastases and for resectability of the lesion (see Chapters 16 and 17). Depending on the patient’s presenting symptoms, the initial study that identifies the lesion will vary (see Fig. 59.1). Radiologic findings highly suggestive of malignancy include central necrosis or an intraluminal exophytic mass or intramural mass with ulceration (Fig. 59.2). Patients will need either a computed tomography scan or magnetic resonance imaging to assess resectability and rule out metastatic disease. For the tumor to be considered potentially resectable, there should be no evidence of major vascular encasement, distant lymphadenopathy, or distant metastases (e.g., liver, peritoneum, lung). If patients undergo upper GI endoscopy, the lesion can be biopsied at that time. Additionally, if a segmental resection is being considered, an upper GI series is helpful, and the relationship of the tumor to the ampulla should be evaluated by endoscopy.
Risk Factors
The biology of duodenal adenocarcinoma is poorly understood. An adenoma-to-carcinoma sequence similar to that seen in colon cancer has been suggested. In various series of endoscopically resected adenomas, the incidence of malignancy varied from 10% to 42%, with villous adenomas being at higher risk for malignant transformation (Seifert et al, 1992; Witteman et al, 1993). Carcinoma in situ can be adequately treated with a local submucosal excision; however, it is generally impossible to know the maximal depth of invasion of the entire lesion before resection, and a more extensive procedure should be performed for any patient with invasive carcinoma (Bjork et al, 1990).
Patients with FAP are at significant risk for duodenal or ampullary adenomas, with an incidence as high as 88% (Church et al, 1992), and they have an increased relative risk of duodenal cancer of 330 compared with the general population (Offerhaus et al, 1992). Groves and colleagues (2002)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree