Chapter 103 Pancreatic and duodenal injuries
Evolution of the Approach to Pancreatic Trauma
A patient with blunt pancreatic injury was first reported in the Lancet as early as 1827, by Tavers. Although several survivors were subsequently reported after ligation and excision of exteriorized penetrating pancreatic wounds (Otis, 1876), the major advance in the operative treatment came in 1923, when Walton described distal pancreatectomy (see Chapter 62A, Chapter 62B ) as the treatment of choice for pancreatic transection. The dramatic reduction in mortality among patients with pancreatic injuries—from 56% in World War II, mostly due to associated injuries, to 22% in the Korean War—was more a result of improvements in general perioperative care than of specific technical innovations (Sako et al, 1955).
In the final decades of the last century, advances in medical imaging and in surgical technique converged to improve the care of patients with pancreatic trauma. The most important of these was computerized tomography (CT) of the abdomen (see Chapter 16), which for the first time allowed detailed visualization of the pancreas (Udekwu et al, 1996). This enabled surgeons to diagnose hitherto unrecognized pancreatic injuries and to drain peripancreatic fluid collections without the need for a laparotomy.
At approximately the same time, the introduction of endoscopic retrograde cholangiopancreatography (ERCP; see Chapter 18) provided a minimally invasive approach to diagnose leakage from the pancreatic duct after trauma (Buccimazza et al, 2006; Gupta et al, 2004; Lin et al, 2004; Wind et al, 1999; Wong et al, 2002). By contrast, the role of magnetic resonance cholangiopancreatography (MRCP; see Chapter 17) in the evaluation of the injured pancreatic duct remains to be defined (Bhasin et al, 2009; Fulcher et al, 2000).
The presumed adverse effect of pancreatic enzymes on the suture lines of duodenal repairs in patients with injuries to both organs led to the development of the Berne duodenal diverticulization, essentially a Bilroth II gastrectomy combined with biliary diversion (Berne et al, 1968, 1974), to preemptively divert gastric secretions around the repaired duodenum. Later, Jordan introduced the pyloric exclusion procedure (Vaughan et al, 1977), which achieves the same result but with a much simpler operation. Because of its conceptual elegance and technical simplicity, pyloric exclusion rapidly became the buzzword of PDC trauma in the 1990s. This led to very liberal use of the procedure in reported series (Feliciano et al, 1987); however, pyloric exclusion has never been subjected to a prospective randomized trial, and most attempts to compare it retrospectively to simple duodenal repair have demonstrated increased morbidity without benefit (DuBose et al, 2008; Seamon et al, 2007).
Resection of the entire PDC (see Chapter 62A, Chapter 62B ), which is routinely done in elective pancreatic surgery, is very rarely needed in the trauma situation. When complete disruption of the head of the pancreas and surrounding duodenal loop leaves the surgeon with no other choice, a so-called trauma Whipple (TW) may be necessary, but only as a last resort to save an exsanguinating patient. When necessary, the procedure is performed in a staged fashion with resection during the original operation and reconstruction 24 to 48 hours later (Subramanian et al, 2007). This is a reflection of the move toward damage control surgery, the most important paradigm shift in trauma surgery in the last two decades of the last century (Hoey & Schwab, 2002).
Distal pancreatectomy remains the mainstay of treatment of patients with major ductal disruption (Balasegaram & Lumpur, 1976; Heitsch et al, 1976); however, reports of successful stenting of the injured pancreatic duct via ERCP (Lin et al, 2006, 2007) suggest that this minimally invasive intervention may evolve into a safe management option in selected patients. Pancreatic trauma continues to tax the judgment and operative skills of experienced surgeons, even as sophisticated, minimally invasive diagnostic and therapeutic adjuncts continue to evolve.
Surgical Anatomy of the Pancreas and Duodenum: A Trauma Surgeon’s Perspective (See Chapters 1A and 1B)
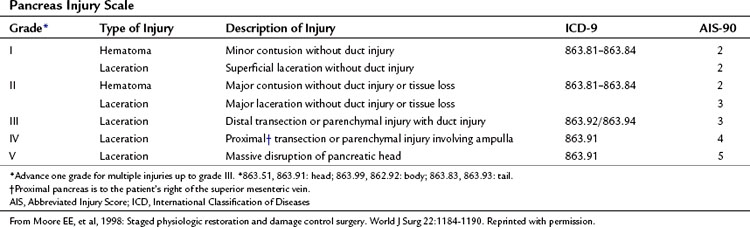
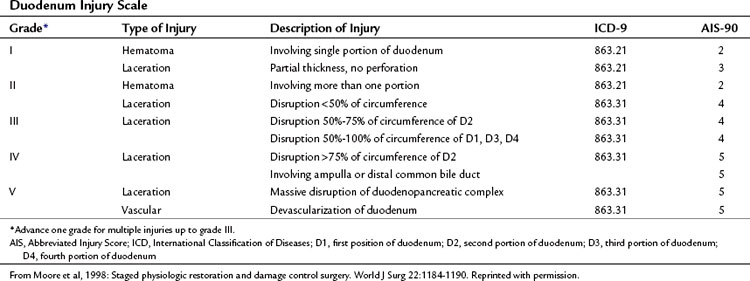
The organ injury scales for the pancreas and duodenum, developed by the American Association for the Surgery of Trauma (AAST) (Tables 103.1 and 103.2; Moore et al, 1990) are used for grading injuries of these two organs. Unfortunately, these scales do not acknowledge the fundamental anatomic differences between the pancreatic body and tail and the PDC, and therefore their clinical usefulness is limited.
For practical purposes, trauma to the pancreas ranges from superficial injuries that require only drainage (Feliciano, 1989) to ductal disruption that mandates a distal pancreatectomy. Low-grade injuries to the duodenum can be repaired the same as any other penetrating injury to the gut; however, high-grade duodenal injuries, and especially those that combine duodenal and pancreatic trauma, require a different approach because of the high risk and unforgiving nature of a duodenal leak. Injuries that destroy the PDC or disrupt the ampulla are rare and carry very high mortality rates because of associated trauma to adjacent major vascular structures. This perspective on pancreatic anatomy forms the basis for a detailed discussion of the management of pancreatic injuries in the forthcoming sections.
Diagnosis of Pancreatic and Duodenal Trauma
Hemodynamically stable patients with injuries to the pancreas and/or duodenum may exhibit only subtle signs because of the retroperitoneal location of these organs. Patients with a history of acceleration/deceleration injury; forceful anterior compression of the abdomen, such as from kicks or handlebar injuries; and lower thoracic and upper lumbar vertebra fractures are at increased risk. A seatbelt sign across the upper and middle abdomen should suggest the possibility of serious intraabdominal injury (Velmahos et al, 1999); however, the physical examination can be remarkably benign: abdominal pain and peritoneal signs sometimes take days to develop. For all of these reasons, a high index of suspicion is essential to avoid missing an injury (Wright & Stanski, 2000).
Routine laboratory tests are not particularly helpful. Obviously, patients with elevations in white blood cell count, amylase, or lipase require further investigation. Unfortunately, many patients are seen with normal values. In fact, as many as 35% of patients with a pancreatic transection have normal amylase levels (Adamson et al, 2003; Jones, 1985; Sriussadaporn, 1994; Takishima et al, 1997).
On abdominal CT scan, injury to the duodenum is usually obvious; however, the initial CT findings of pancreatic injury may be quite subtle (Akhrass et al, 1997; Bradley et al, 1998; Canty & Weinman, 2001; Ilahi et al, 2002) even with a study using thin slices of the pancreatic area. If a definitive diagnosis is not possible, a repeat CT scan 8 to 12 hours later allows time for retroperitoneal edema as a result of leakage of pancreatic secretions, which better delineates the injury. Fluid in the lesser sac, pancreatic hematomas, and pancreatic lacerations all suggest the diagnosis (Subramanian et al, 2007).
Unfortunately, the abdominal CT scan cannot reliably diagnose a laceration of the main pancreatic duct, unless a complete pancreatic transection is visible (Bradley et al, 1998). ERCP (see Chapter 18) is an excellent test for that purpose and can also be used to stent lacerated ducts in selected patients (Bhasin et al, 2009; Silviera et al, 2009); however, the procedure itself has the potential to cause pancreatitis (Cotton et al, 2009; Silviera et al, 2009) and is generally indicated only when diagnosis of a lacerated duct will change the management of the injury. The role of MRCP in the management of pancreatic trauma remains to be determined (Gillams et al, 2006).
Operative Management of Injuries to the Body and Tail of the Pancreas (See Chapter 62A, Chapter 62B )
In assessing the body and tail of the pancreas, the key question that the surgeon must address is whether a pancreatic duct injury is present (Bach & Frey, 1971; Bradley et al, 1998; Tyburski et al, 2001; Voeller et al, 1991). Unless there is an obvious complete transection, it is difficult to diagnose a duct injury by simple inspection. The integrity of the duct can be interrogated by intraoperative imaging, either by amputating the tail and cannulating the distal duct or by cannulating the gallbladder and injecting contrast into the common bile duct. Both these options are cumbersome and do not have high success rates (Berni et al, 1982).
A transduodenal pancreatogram is mentioned here only to be condemned, because it converts a pancreatic injury into a pancreaticoduodenal (PD) injury. Intraoperative ERCP, first reported in 1986, is another option, if it can be organized expeditiously (Laraja et al, 1986). The more practic option in the middle of the night is to simply proceed with empiric distal pancreatectomy, whenever a deep laceration is in the vicinity of the main pancreatic duct, or a large hematoma is found in the center of the gland. An alternative option for nonbleeding pancreatic injuries, particularly in the face of multiple associated injuries, is closed suction drainage of the lesser sac. Patton and colleagues (1997) demonstrated excellent results by simple drainage, regardless of the location of the injury. A disruption of the capsule should be drained without attempting to repair it. Drainage of an injured main pancreatic duct is an effective solution, but it often results in a high output pancreatic fistula, so distal pancreatectomy may be a better option.
The trauma literature of the 1970s and 1980s is replete with descriptions of pancreas-preserving techniques for complete pancreatic transections (Frey, 1982
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree