Pancreas Cancer: Clinical Management
John P. Hoffman
Christopher G. Willett
Steven J. Cohen
Surgical Considerations in the Management of Pancreatic Adenocarcinoma
The clinical management of pancreatic cancer has undergone many fundamental changes since the 1970s. During that decade, few patients were offered any hope after diagnosis. Since then, however, we have seen major improvements in the safety of surgical resection, the quality of radiation therapy, and the efficacy of systemic therapy. Still, the majority of patients diagnosed with pancreatic adenocarcinoma succumb to the disease.
Once an image (transcutaneous ultrasound, computed tomography [CT] scan, or magnetic resonance imaging) shows an abnormal mass or dilatation of pancreatic and/or bile ducts (from a single stricture), the possibility of a pancreatic cancer should be recognized. From this point on, controversy exists at nearly every step in the process from suspicion of cancer to its proof to its treatment (Fig. 28.1A and B).
If jaundice is associated with a mass in the pancreatic head, the issue of biliary stent placement arises. For many years, surgeons have argued that the majority of mass lesions causing jaundice will be malignant, that inserting a needle into the tumor from the peritoneal cavity may cause tumor seeding, and that preoperative biliary stenting increases the perioperative morbidity and mortality (1,2,3). Counterarguments would bring up rare lesions such as lymphoma and localized pancreatitis, which can be successfully treated without resection. Furthermore, semiurgent resection solves the problem of obstructive jaundice and therefore obviates the need for preoperative stent placement. Those that provide adjuvant treatment given prior to resection (neoadjuvant therapy) require biopsy proof that the lesion is an adenocarcinoma before providing the therapy. Because neoadjuvant therapy requires a period of at least 2 to 3 months prior to surgery, biliary stenting is also usually necessary for such an approach. Although it has been shown to be problematic in some neoadjuvant series, others had few complications if the stents were changed frequently (4,5). Now that biopsies are more easily obtained by endoscopic ultrasonography and the biopsy needle does not traverse the peritoneal cavity, more surgeons are requesting preoperative biopsies, even when no neoadjuvant therapy is planned. Although pancreatic resection for masses not proven to be neoplastic has been recommended for decades in surgical teachings, the present climate of litigation promotes at least an attempt at preoperative tumor confirmation. Even with state-of-the-art ultrasonic endoscopic biopsy techniques, the fibrosis and inflammatory reaction surrounding many pancreatic adenocarcinomas may render even multiple needle biopsy attempts unsuccessful. Thus, many patients will have resections without preoperative and intraoperative biopsy confirmation of cancer.
The presence of a solid mass increases the probability of cancer. However, several forms of pancreatitis (focal pancreatitis, lymphocytoplasmic sclerosing pancreatitis, chronic pancreatitis) can present as a mass. In addition, pancreatic lymphoma, metastatic lesions, and pancreatic endocrine lesions can also present as pancreatic masses. Each may have a different treatment algorithm (see Chapter 25).
Classically, pancreatic adenocarcinoma in the head of the pancreas will demonstrate obstruction of both pancreatic and bile ducts (double duct sign). Sometimes one or the other duct will be strictured without a visible surrounding mass. These stenoses may be assessed cytologically by endoscopically mediated brushings. Endoscopic ultrasonography may show the presence of a small associated mass not well seen by other imaging modalities. Kalady et al. studied a large series of such patients in an era prior to use of endoscopic ultrasound (6). They found that tumor location (head vs. other), a history of no prior pancreatitis, and an endoscopic retrograde cholangiopancreatography showing no fibrotic changes in pancreatic duct side branches correlated with a 94% chance of a diagnosis of pancreatic cancer. The double duct sign had a positive predictive value of only 65% and a negative predictive value of 87.6% (6). It is therefore rational to proceed with resection in such cases, even after multiple preoperative and intraoperative attempts at biopsy confirmation have failed. However, the patients and their families must be made fully aware of the possible untoward consequences, both with resection (operative complications and the possibility of benign findings) and with observation (continued growth of a malignant lesion).
Cystic Masses
Cystic masses form another controversial category, both from a diagnostic and a treatment perspective. Treatment is, of course, based on an estimate of the future behavior of any given lesion. Formerly, lesions were grouped by imaging characteristics into serous and mucinous lesions. Now we have a spectrum from a small, microcystic lesion to a large either single or complex cyst. We can now measure many cytologic and molecular features of the fluid and cell walls. However, there is not unanimity of opinion as to when to resect these lesions. Allen et al. from Memorial Sloan-Kettering Cancer Center have a large database of patients with cystic lesions of the pancreas who have been either observed or operated on based on radiographic and clinical criteria (size <3 cm, no solid component, no septations, and no pain) (7). This was a retrospective review of what surgeons
decided at this institution. The study is ongoing, but preliminary reporting indicates that there are cysts <3 cm in diameter, without symptoms, solid components, or septations that are safe to observe. Many others have been in the process of assessing endoscopically obtained cyst fluid for the discovery of tissue fragments or molecular markers of malignancy (8,9,10).
decided at this institution. The study is ongoing, but preliminary reporting indicates that there are cysts <3 cm in diameter, without symptoms, solid components, or septations that are safe to observe. Many others have been in the process of assessing endoscopically obtained cyst fluid for the discovery of tissue fragments or molecular markers of malignancy (8,9,10).
Once a lesion is either proven or highly suspected to be pancreatic adenocarcinoma, issues of importance in the therapy are resectability, the conduct of the resection, and adjuvant therapy. The latter is largely covered in the subsequent sections from the perspectives of radiation therapy and chemotherapy.
Resectability
Definitions of what constitutes a lesion that may be removed with safety and a reasonable probability of prolonged postoperative survival have varied since the 1970s. When surgical resection was the only method of therapy, only those lesions that were small, well away from the superior mesenteric vessels, and free of gross nodal metastases held any chance for meaningful prolonged postoperative survival. With the advent of somewhat effective adjuvant therapy, larger lesions and those impinging on the mesenteric vessels and involving regional lymph nodes can now be safely removed and occasionally achieve significant postoperative survival (11).
The 1970s definition of a resectable cancer was that of a lesion without distant or regional nodal spread and one that was not abutting the superior mesenteric vessels. An intraoperative test for resectability was the easy passage of a clamp beneath the neck of the pancreas overlying the superior mesenteric vein. Current imaging criteria for resectability include lack of distant metastases and the same lack of involvement of the superior mesenteric vein, as well as a clear fat plane surrounding the superior mesenteric artery (SMA). With the demonstration of chemotherapy and radiation therapy effects on these tumors, many have used this adjuvant therapy in a preoperative sequence, allowing for marginfree resections of more locally advanced pancreatic cancers (12). These locally advanced cancers are defined as borderline resectable lesions (Table 28.1). Those lesions that are considered never to be resectable, even with successful preoperative adjuvant therapy, are called locally unresectable (Table 28.1). These terms have been poorly delineated in the literature, such that the conscientious readers must be cautious as to the effects of treatment until they understand the extent of the lesions being discussed.
Table 28.1 Three resectability categories for localized pancreatic adenocarcinoma | |
|---|---|
|
Laparoscopy performed as a separate preoperative procedure or done immediately prior to a planned resection may occasionally discover distant metastases not seen on imaging studies. Opinion and data differ as to its indications (13,14). As imaging becomes more discriminative and tumors become smaller, the indications for staging laparoscopy will diminish. For more advanced lesions and those arising in the tail or body of the pancreas (usually discovered at a later stage), most authors would advise preoperative laparoscopy. The scope of the procedure may also vary, from an inspection of the peritoneal surfaces only to laparoscopic liver ultrasound and dissection within the lesser omental bursa and excisional biopsy of distant nodes. See Chapter 26 for a full discussion of these issues.
Surgical Procedures
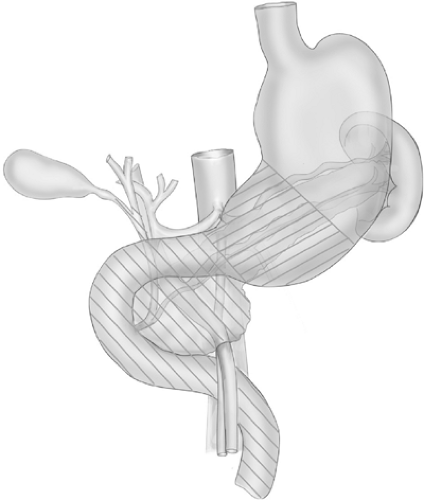
The procedures usually performed for pancreatic cancer are pancreatoduodenectomy with or without resection of the gastric antrum and pylorus (Whipple or Kausch-Whipple procedure), distal pancreatectomy, and total pancreatectomy (Fig. 28.2). The primary indications for each procedure are the location and extent of the cancer. There have been multiple trials comparing the pylorus-preserving and antrectomy operations, but there were no strong differences in tumor control or quality of life found.
Some surgeons stress a complete dissection of tissue surrounding the SMA, whereas the majority leaves some adjacent tissue and the nerve plexi around it. There have been several surgical trials of “radical” versus “standard” lymph node and soft tissue dissection (15,16,17). However, the definition of what peripancreatic lymphatic and soft tissue should be included in the “standard” dissection varies. Even the smallest pancreatic
adenocarcinomas will not have widely free surgical margins because of the close proximity of the pancreatic head and uncinate process to the superior mesenteric vessels. Thus, it is rational to dissect at least all tissue from the tumor edge to the nearest side of the superior mesenteric vessels, and to resect all lymph nodes within 5 to 6 cm of the tumor.
adenocarcinomas will not have widely free surgical margins because of the close proximity of the pancreatic head and uncinate process to the superior mesenteric vessels. Thus, it is rational to dissect at least all tissue from the tumor edge to the nearest side of the superior mesenteric vessels, and to resect all lymph nodes within 5 to 6 cm of the tumor.
What adjacent organs or tissues may be resected along with a pancreatic cancer and what is the expectation of disease control? Direct invasion of a cancer into the colon, mesocolon, adrenal gland, stomach, small bowel, or superior mesenteric vein does not render that cancer unresectable or incurable (18). However, resection of liver metastases along with primary cancers is not associated with long-term survival.
Complications of Surgery
Other than the usual morbidity and mortality of major abdominal surgery, pancreatic resection has its unique complications. Whenever the pancreas is divided, its reconnection to either the small bowel or stomach is sometimes tenuous. The incidence of leakage from the pancreatic anastomosis is increased with a soft pancreas and a small pancreatic duct, and in hospitals where the surgery is not performed frequently (19,20). There are many definitions of leakage at the pancreatic anastomosis (21). Therefore, its incidence is unclear. However, the most serious complications of intraabdominal hemorrhage and infection are usually associated with leakage at the pancreatic anastomosis. Fortunately, this is an unusual occurrence in experienced hands.
Palliative Surgery
Palliative surgery may be emergency or elective. Often, ulceration in the stomach or duodenum by a cancer may occur. This is more common after chemotherapy and/or radiation therapy have shrunken the cancer and left a hemorrhaging vessel. Usually, these vessels can be controlled with embolization by the interventional radiologist, but occasionally the tumor and vessel need to be excised. The operation performed in these circumstances is usually an R2 resection (where gross tumor is left behind). Although this type of procedure is not recommended unless it is the only option to immediately save a life, it has occasionally been associated with long survival in a patient with a cancer sensitive to chemotherapy.
The more common emergency surgery for these tumors is bypass of an obstructed duodenum by gastrojejunostomy (22). Although most patients with peritoneal metastases from pancreatic cancer will eventually develop small bowel obstruction, it is unusual for the surgeon to be able to help them because the metastases are frequently diffuse.
Elective palliative surgery will be either to alleviate or prevent future biliary or duodenal obstruction. This would usually be in the setting of a planned resection where distant metastases were discovered, thus rendering resection irrational. Because the patient’s abdominal cavity is already exposed, a bypass of the bile duct and duodenum can be performed without any extra incision. A prospective, randomized trial showed that approximately 20% of these patients will go on to have duodenal obstruction before death if no prophylactic bypass is done (23). However, most surgeons would use nonoperative means to bypass biliary or duodenal obstructions in patients with metastatic disease proven before exploratory celiotomy.
Patency of bile duct or duodenum can be accomplished by means of stents by the gastroenterologists or interventional radiologists. There have been a number of trials comparing biliary stents with surgical bypass (24). Most of these show that surgical procedures necessitate more hospitalization initially but less eventually, and produce much longer palliation without the need for stent change. Even the larger metal stents will need attention every 4 to 6 months. As this technology advances, there will probably be little need for open surgical palliative procedures. However, laparoscopically performed bypasses will probably be more competitive.
Radiation Therapy in the Treatment of Pancreatic Adenocarcinoma
Adjuvant Therapy
After resection of pancreatic cancer, local recurrence occurs in 50% to 90% of patients (25,26,27,28). Forty to 90% of patients develop distant metastases, most commonly in the liver and/or peritoneum. For this reason, adjuvant radiation therapy, chemotherapy, and combined radiation and chemotherapy have been studied in an effort to improve patient outcomes (Table 28.2). However, despite multiple trials, a definitive role for adjuvant therapy for resected pancreatic cancer has not been established.
Prospective Trials
The Gastrointestinal Tumor Study Group (GITSG) conducted the first prospective trial of adjuvant chemoradiotherapy for patients with resected pancreatic cancer and negative surgical margins (29). These patients were randomized to external beam radiation therapy (ERBT) to 40 Gy delivered in split-course fashion with concurrent 5-fluorouracil (5-FU) 500 mg/m2 given as an intravenous bolus on the first 3 and last 3 days of
radiation, followed by maintenance 5-FU for 2 years or until disease progression, or to observation only. This trial was stopped early secondary to slow accrual (43 patients over 8 years) and a positive interim analysis, which found that patients treated on the chemoradiotherapy arm had a positive survival benefit. Patients who received chemoradiotherapy had a longer median survival (21 months vs. 11 months) and a higher 2-year survival (43% vs. 19%). An additional 30 patients were then enrolled to receive adjuvant chemoradiation (30). These additional patients confirmed the survival outcomes seen in the original trial with median survival of 18 months and a 2-year survival of 46%. The GITSG trial was criticized for many reasons: only 9% of patients received the 2-year maintenance chemotherapy, the radiation dose was low, the number of patients was small, there was slow accrual, there was an unusually poor survival for the surgical control group, 25% of patients did not begin adjuvant therapy until more than 10 weeks after resection, and 32% of the original treatment arm had violations of the scheduled radiation therapy. Nevertheless, this trial resulted in chemoradiation therapy being accepted as appropriate adjuvant therapy in the United States.
radiation, followed by maintenance 5-FU for 2 years or until disease progression, or to observation only. This trial was stopped early secondary to slow accrual (43 patients over 8 years) and a positive interim analysis, which found that patients treated on the chemoradiotherapy arm had a positive survival benefit. Patients who received chemoradiotherapy had a longer median survival (21 months vs. 11 months) and a higher 2-year survival (43% vs. 19%). An additional 30 patients were then enrolled to receive adjuvant chemoradiation (30). These additional patients confirmed the survival outcomes seen in the original trial with median survival of 18 months and a 2-year survival of 46%. The GITSG trial was criticized for many reasons: only 9% of patients received the 2-year maintenance chemotherapy, the radiation dose was low, the number of patients was small, there was slow accrual, there was an unusually poor survival for the surgical control group, 25% of patients did not begin adjuvant therapy until more than 10 weeks after resection, and 32% of the original treatment arm had violations of the scheduled radiation therapy. Nevertheless, this trial resulted in chemoradiation therapy being accepted as appropriate adjuvant therapy in the United States.
Table 28.2 Prospective, Randomized Trials for Adjuvant Therapy for Pancreatic Cancer | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
A second study sponsored by the European Organization for Research and Treatment of Cancer sought to confirm the findings of the original GITSG study (31). In this trial, 218 patients with resected pancreas or periampullary cancers were randomly assigned to receive 40 Gy of EBRT in a split-dose fashion with concurrent continuous infusional 5-FU (25 mg/kg/day) or observation alone. This study showed no significant improvement (p = 0.208) in median survival (24 months vs. 19 months) or 2-year survival (51% vs. 41%). Interestingly, only 114 of the patients enrolled on trial had pancreatic cancer, the remaining patients had ampullary tumors. Subset analysis of the patients with primary pancreatic tumors showed a 2-year survival of 34% for treated patients versus 26% for the control group (p = 0.099). Criticisms of this trial are that there was no maintenance chemotherapy given in the treatment arm, patients with positive surgical margins were allowed on trial with no prospective assessment, the radiation dose was low, there were low numbers of patients, and 20% of patients assigned to treatment never received treatment.
The European Study Group for Pancreatic Cancer (ESPAC) then conducted the largest trial evaluating adjuvant therapy for pancreatic cancer, ESPAC-1 (32). Treating physicians were allowed to enroll their patients onto one of three parallel randomized studies:
Chemoradiation versus no chemoradiation (n = 69): Chemoradiation was 20 Gy over 2 weeks with 5-FU 500 mg/m2 on days 1 to 3, and then repeated after a 2-week break.
Chemotherapy versus no chemotherapy (n = 192): Chemotherapy was bolus 5-FU (425 mg/m2) and leucovorin (20 mg/m2) given daily for 5 days every 28 days for 6 months.
A 2 × 2 factorial design of 289 patients enrolled on chemoradiotherapy (n = 73), chemotherapy (n = 75), chemoradiotherapy with maintenance chemotherapy (n = 72), or observation (n = 69).
The data from the treatment groups from all three parallel trials were then pooled for analysis. There was no survival
difference between the 175 patients who received adjuvant chemoradiation and the 178 patients who did not receive therapy (median survival 15.5 months vs. 16.1 months, p = 0.24). There was, however, a survival benefit found for the patients who received adjuvant chemotherapy (n = 238) compared to those who did not (n = 235) (median survival 19.7 months vs. 14 months, p = 0.0005). On further follow-up of the 289 patients selected to the 2 × 2 factorial design trial, the 5-year survival rate for the patients who received chemotherapy was 21% versus 8% for those who did not (33).
difference between the 175 patients who received adjuvant chemoradiation and the 178 patients who did not receive therapy (median survival 15.5 months vs. 16.1 months, p = 0.24). There was, however, a survival benefit found for the patients who received adjuvant chemotherapy (n = 238) compared to those who did not (n = 235) (median survival 19.7 months vs. 14 months, p = 0.0005). On further follow-up of the 289 patients selected to the 2 × 2 factorial design trial, the 5-year survival rate for the patients who received chemotherapy was 21% versus 8% for those who did not (33).
Like its predecessors, the ESPAC-1 trial had many criticisms:
Physicians and patients were allowed to choose which of the three parallel trials to enroll in, creating bias.
Patients could receive “background” chemoradiation or chemotherapy if decided by their physician. Approximately one-third of the patients enrolled on the chemotherapy versus no chemotherapy trial received “background” chemoradiation therapy or chemotherapy.
The radiation therapy was given in a split-dose fashion, with the treating physician judging the final treatment dose (40 Gy vs. 60 Gy).
In addition, there were no uniform guidelines for radiation therapy administration across participating centers and no central quality assurance review. The investigators of this trial concluded that (a) there was no benefit from adjuvant chemoradiation therapy, and (b) there was a benefit to adjuvant chemotherapy.
Recently, a meta-analysis of randomized adjuvant therapy trials for pancreatic cancer reported an improved outcome of patients with resected tumors with positive margins receiving postoperative radiation therapy and chemotherapy (34). It was recommended that further study of chemoradiation be pursued in this subset of patients.
Single Institution Experiences
Reports of single-institution experiences with adjuvant therapy for pancreatic cancer have provided support to the benefit of adjuvant therapy. The largest of these series is from The Johns Hopkins Medical Institutions, where investigators reported the results of a retrospective analysis of 174 patients who were treated by one of the following approaches: (a) EBRT (40–45 Gy) with two 3-day courses of 5-FU at the beginning and end of radiation, followed by weekly bolus 5-FU (500 mg/m2) for 4 months (n = 99); (b) EBRT (50.4–57.6 Gy) to the pancreatic bed plus prophylactic hepatic irradiation (23.4–27 Gy) given with infusional 5-FU (200 mg/m2/day) plus leucovorin (5 mg/m2/day) for 5 of 7 days of the week for 4 months (n = 21); or (c) no therapy (n = 53) (35). Patients who received adjuvant chemoradiation had a median survival of 20 months compared to 14 months for patients who were not treated. Two-year survival was 44% and 30%, respectively. There was no survival advantage to the more intensive adjuvant therapy. A follow-up report from this group of 616 patients with resected pancreatic cancer found adjuvant chemoradiation treatment as a strong predictor of outcome, with a hazard ratio of 0.5 (36).
In addition to the Johns Hopkins series, a few small series from the Mayo Clinic and the University of Pennsylvania have also reported survival benefit to adjuvant chemoradiation therapy (37,38). In these series, the EBRT dosed in a range of 45 to 54 Gy in combination with 5-FU–based therapy yielded a superior 5-year survival compared to no therapy (17% vs. 4% and 43% vs. 35%, respectively). A series of Medicare patients from the Surveillance, Epidemiology, and End Results database has found an improved median and 3-year survival for patients who received adjuvant chemoradiation therapy over those who did not (29 months vs. 12.5 months, 45% vs. 30%, respectively) (39). However, it must be noted that in these retrospective analyses, there is a possible bias toward the treatment of better-risk patients.
Data with the highest seen survival after adjuvant therapy for pancreatic cancer come from a phase II trial done at Virginia Mason University (40). Results from 43 of 53 enrolled patients on this study were reported in 2003. These patients were treated with EBRT to 50 Gy, with concurrent chemotherapy of 5-FU 200 mg/m2/day continuous infusion, cisplatin 30 mg/m2 weekly, and IFN-α 3 million units subcutaneously every other day. After completion of chemoradiation, patients received 5-FU 200 mg/m2/day continuous infusion on weeks 10 through 15 and 18 through 23. The median survival, 2-year overall survival, and 5-year overall survival were 44 months, 58%, and 45%, respectively. With these encouraging data came significant toxicity, with 70% of patients experiencing grade 3 toxicities, and 42% of patients requiring hospitalization. The American College of Surgeons Oncology Group has recently completed a larger, multicenter, phase II trial of 100 patients to further investigate this regimen.
Current Trials
There are several ongoing large clinical trials that are attempting to further clarify the role of adjuvant therapy for pancreatic cancer. The first is Radiation Therapy Oncology Group (RTOG) and GI Intergroup Trial 9704. This is a phase III study of 519 patients with resected pancreatic cancer randomized to either 3 weeks of continuous infusional 5-FU at 250 mg/m2/day, followed by chemoradiation (50.4 Gy in 1.8-Gy daily fractions with continuous infusional 5-FU at 250 mg/m2/day) and then two 4-week courses of continuous infusional 5-FU at 250 mg/m2/day with 2 weeks rest between courses to begin 3 to 5 weeks after completion of chemoradiation, or three weekly doses of gemcitabine at 1,000 mg/m2/week, followed by the same 5-FU–based chemoradiation as in the first arm and then 3 months of gemcitabine 1,000 mg/m2 given weekly 3 of every 4 weeks. Accrual to this trial has been completed. In Europe and Australia, ESPAC-3 has enrolled more than 500 patients of a planned 990. Originally, this study was to randomized patients with resected pancreatic cancer into one of three arms: 5-FU (425 mg/m2) and leucovorin (20 mg/m2) given daily for 5 days every 28 days for 6 months, gemcitabine (1,000 mg/m2) given weekly over 30 minutes for 3 of 4 weeks for 6 months, or observation. However, with the release of the matured ESPAC-1 data confirming a survival benefit to chemotherapy over observation, the observation arm has now been dropped from this trial. Notably, radiation therapy has been excluded from this trial.
Neoadjuvant Therapy
Even after undergoing curative resection for pancreatic cancer, 80% to 85% of patients will recur. In addition, positive margins or nodal disease increases this rate of recurrence to 90% (41,42). The concept of preresectional radiation therapy for these cancers arose in the early 1980s (43,44). Chemotherapy was added to the radiation therapy in the late 1980s (45,46). The use of neoadjuvant chemoradiation offers another possible way to improve on these figures for several reasons:
Approximately 25% of patients do not receive adjuvant therapy in a timely manner after surgery or do not receive it at all (36,47).
Given the high recurrence rates after surgical resection, pancreatic cancer is likely a systemic disease at the time of
diagnosis in 80% to 85% of patients who appear to have resectable disease (48,49), and with neoadjuvant therapy, 20% to 40% of patients will be spared the morbidity of resection because their metastatic disease becomes clinically apparent (50).
Preoperative therapy could theoretically be less toxic and more effective because the chemotherapy and radiation would be given without the postsurgical issues of small bowel in the radiation field and decreased oxygenation and decreased drug delivery to the remaining tumor bed (51).
Many patients with borderline resectable and occasional patients with unresectable lesions may be able to be downstaged to allow for surgical resection.
Other putative but unproven advantages are the preservation of function of stomach and small bowel spared from irradiation and the decreased frequency of pancreatojejunostomy leaks (19).
Indications for preoperative adjuvant therapy vary from the clearly resectable to the borderline resectable patient. The primary proponents for preoperative therapy for clearly resectable lesions have been the pancreatic surgeons at the MD Anderson Cancer Center. Because of the previous theoretical advantages to preoperative adjuvant therapy sequencing, they prefer to use it in any patient with a biopsy-proven pancreatic adenocarcinoma. They have performed several serial phase II studies of different preoperative regimens (50). The diseasefree and overall survival rates from these regimens rival any reports from postoperative adjuvant therapy trials. However, no phase III trials of preoperative versus postoperative sequencing have been conducted. Superior results may be obtained in any phase II trial simply by patient selection. Although we have many prognostic indicators for any given cancer (size, differentiation, depth of invasion, venous or arterial abutment or invasion, presence and number of nodal metastases, type of tumor, CA19–9 status), there are undoubtedly others not yet discovered. Thus, the question of the value of any sort of neoadjuvant therapy (as opposed to postoperative adjuvant therapy) will remain unanswered until phase III testing is done.
Another indication for preoperative adjuvant therapy is in the patient with borderline resectable pancreatic cancer because such a lesion would not be able to be resected with clear margins without the preoperative therapy. In a review of patients treated at one institution by either preoperative or postoperative chemoradiotherapy, Pingpank et al. showed that preoperative therapy led to more clear surgical margins and fewer multiply positive margins than did postoperative adjuvant therapy (12). The group treated with postoperative adjuvant therapy was actually a more favorable group with respect to tumor size and resectability status. Eventually, however, this setting for preoperative therapy will probably also need to be studied in phase III trials.
Before too much progress can be made in this group of patients with borderline resectable cancers, we need to develop and adopt a complex grading system of imaging parameters that could be correlated to clinical outcomes in order to determine specific prognostic factors for each imaging characteristic (52).
5-Fluorouracil–Based Regimens
Small initial studies of neoadjuvant radiation with and without continuous infusion 5-FU established the tolerability of this regimen, but showed no improvement in survival or resectability for these patients (43,44,53,54,55). For this reason, further studies were done increasing the radiation dose, with different chemotherapy regimens, and with intraoperative radiation therapy (IORT) at the time of surgery.
The Eastern Cooperative Oncology Group (ECOG) treated 53 patients with potentially resectable pancreatic cancer with 5-FU 1,000 mg/m2/day continuous infusion on days 2 to 5 and 29 to 32 of radiation, mitomycin 10 mg/m2 on day 2, and EBRT to 50.4 Gy4. Nine (17%) of the treated patients developed either local progression of disease or distant metastases and were not surgical candidates, 11 patients (21%) had metastatic disease at surgery, and complete resection was possible in 24 of the 41 patients taken to surgery. For the patients who underwent resection, the median survival was 16 months, and 10 months for the entire group. The poor survival for the patients who did undergo resection was likely due to 3 of the patients having positive peritoneal cytology, 4 having lymph node metastases, 13 having close surgical margins, and 4 needing resection of the superior mesenteric vein. In addition, more than 50% of the treated patients required hospitalization due to treatment toxicity.
At MD Anderson Cancer Center, multiple trials of neoadjuvant 5-FU–based chemoradiation have been performed. The first trial treated 28 patients with 5-FU 300 mg/m2/day continuous infusion with concurrent EBRT to 50.4 Gy over 5.5 weeks (55). Patients who underwent surgical resection also received intraoperative radiation therapy. Twenty-five percent of patients had evidence of metastatic disease on preoperative restaging. Fifteen percent had metastatic disease that was found on laparoscopy. For the patients that underwent surgery, median survival was 18 months, and 41% had a pathological partial response to therapy. However, 33% of patients treated on this study required hospitalization for gastrointestinal toxicity from therapy. For this reason, the next trials from this group focused on rapid fractionation EBRT. A prospective trial of 35 patients treated with EBRT to 30 Gy (3 Gy per fraction for 10 fractions) with concurrent 5-FU 300 mg/m2/day continuous infusion found grade 3 nausea and vomiting in only 9% of patients with no grade 4 toxicities (56). Twenty-seven patients were taken to surgery and 20 patients underwent resection and IORT to 10 to 15 Gy. Locoregional recurrence occurred in only 2 of the 20 resected patients. Median survival for patients who underwent surgery was 25 months with a 3-year survival of 23%.
Gemcitabine-Based Regimens
Several phase I studies have attempted to use the radiosensitization effects and the improved efficacy in advanced pancreatic cancer of gemcitabine in the neoadjuvant setting. A phase I study of twice-weekly gemcitabine in combination with EBRT to 50.4 Gy in 28 fractions for patients with localized pancreatic cancer found a maximum tolerated dose (MTD) of 50 mg/m2 twice a week (57). Another phase I study used full-dose gemcitabine in combination with EBRT (58). The gemcitabine was given as 1,000 mg/m2 over 30 minutes on days 1, 8, and 15 of a 28-day cycle. Radiation therapy was directed at the primary tumor alone at a starting radiation dose of 24 Gy in 1.6-Gy fractions. The MTD of the radiation was 36 Gy in 2.4-Gy fractions. The dose-limiting toxicities were vomiting and gastroduodenal ulceration. The phase II trial of this regimen enrolled 41 patients with resectable or locally advanced pancreatic cancer. Eight of the 32 evaluable patients for toxicity showed grade 3 gastrointestinal toxicity, grade 3 fatigue, and one unexplained death (59). Survival data are not yet available. Another trial of weekly gemcitabine at a dose of 400 mg/m2 for seven doses plus concurrent ERBT to 30 Gy in 10 fractions over 2 weeks, beginning 3 days after first gemcitabine dose, has had preliminary results reported (60). Of the 86 patients treated, all received the total dose of radiation, but only 45%
received the full dose of gemcitabine. Forty-three percent of patients were hospitalized prior to surgery. However, 86% of patients went to laparotomy, with 73% undergoing a successful tumor resection, and 59% of tumor specimens had >50% tumor necrosis. The median survival was 37 months.
received the full dose of gemcitabine. Forty-three percent of patients were hospitalized prior to surgery. However, 86% of patients went to laparotomy, with 73% undergoing a successful tumor resection, and 59% of tumor specimens had >50% tumor necrosis. The median survival was 37 months.
Gemcitabine has also been studied in combination with other chemotherapy agents and EBRT in the neoadjuvant setting. A phase I study of 19 patients with pancreatic cancer evaluated the MTD of cisplatin when given with gemcitabine at 1,000 mg/m2 weekly with EBRT to 36 Gy given in 2.4-Gy fractions (61). Cisplatin was given on days 1 and 15 following gemcitabine. The MTD of cisplatin was 40 mg/m2. Another trial by the MD Anderson Cancer Center group evaluated a treatment schedule of gemcitabine 750 mg/m2 and cisplatin 30 mg/m2 given every 14 days for four treatments, followed by four weekly doses of gemcitabine at 400 mg/m2 concurrent with 30 Gy of EBRT given as 3-Gy fractions over 2 weeks, beginning 2 days after the first dose of gemcitabine (62). Preliminary results from 37 patients showed 67% underwent resection, with 70% of the pathological specimens showing necrosis of >50% of the tumor. This regimen, however, had significant toxicity, with 62% of patients requiring hospitalization, most due to biliary stent occlusion.
Taxane-Based Regimens
In radiobiological models, paclitaxel may result in enhanced radiosensitization through (a) synchronization of tumor cells at G2/M, a relatively radiosensitive phase of cell cycle; and (b) tumor reoxygenation after apoptotic clearance of paclitaxel-damaged cells. Pisters et al. from MD Anderson Cancer Center examined the use of paclitaxel as a radiation sensitizer in the neoadjuvant setting for pancreatic cancer (63). In this trial, 35 patients received paclitaxel 60 mg/m2 weekly with concurrent EBRT to 30 Gy. Eighty percent underwent resection with 21% of pathology specimens showing >50% tumor necrosis. The 3-year survival for the patients who underwent preoperative therapy and resection was 28%. Hospitalization was required in 11% of patients for toxicity, primarily involving nausea and vomiting. These preliminary data show an increased toxicity without a significant improvement compared to histologic response rate or overall survival for this paclitaxel-based regimen.
Targeted Therapies/Future Directions
Future directions for neoadjuvant therapy include the incorporation of novel, targeted agents with ERBT alone or with chemoradiation, and newer radiation therapy techniques. The use of targeted therapies is based on impressive phase II data combining targeted agents with chemotherapy in the metastatic pancreatic cancer setting. A phase II trial of the vascular endothelial growth factor (VEGF) inhibitor, bevacizumab, in combination with gemcitabine for patients with advanced pancreatic cancer (64) has shown a response rate of 27% compared to 5.6% historically for gemcitabine alone (65), and a 1-year survival of 53% compared to <20%, respectively. A phase II trial of an epidermal growth factor receptor (EGFR) inhibitor, cetuximab, in combination with gemcitabine for patients with advanced pancreatic cancer has shown a 1-year survival of 33% (66). In addition, a randomized controlled phase III trial of gemcitabine ± erlotinib, another EGFR inhibitor, has shown a 23.5% increase in overall survival with the addition of erlotinib compared to gemcitabine alone (67). No trials of these agents in the neoadjuvant setting have yet been reported, but preliminary results are available in the locally advanced setting. The use of intraoperative radiation therapy technique and three-dimensional conformal radiation therapy is further discussed in the locally advanced section.
Unfortunately, there are few randomized studies comparing different chemotherapy partners for radiation therapy in pancreatic cancer. In addition, results regarding resectability are difficult to compare due to differing definitions of unresectable disease. Recent efforts by the ECOG to compare gemcitabine with 5-FU–based radiation programs for potentially resectable patients (E1200) and gemcitabine alone with gemcitabine and radiation therapy (E4201) for unresectable disease both closed due to poor accrual. A small study randomized 34 patients with locally advanced disease to receive radiation therapy with either weekly gemcitabine 600 mg/m2 (n = 18) or 3 days of bolus 5-FU every 2 weeks (n = 16) (68). Although median survival favored gemcitabine (14.5 m vs. 7.1 m, p = 0.027), the small sample size and significant toxicity limits firm conclusions. Thus, either 5-FU or gemcitabine (but not both) can be administered with radiation therapy for locally advanced disease or as preoperative therapy. However, the impact on the natural history of the disease is unclear and patient prognosis, if not rendered resectable, is uniformly fatal. Thus, the study of new compounds with radiation therapy is critical. A phase I study of bevacizumab with capecitabine and radiation in locally advanced pancreatic cancer documented a response rate of 20% with 4 patients able to undergo a margin negative resection. However, 4 patients had more than or equal to a grade 3 gastrointestinal ulceration with bleeding or perforation (69). An RTOG phase II study of this regimen recently reached its accrual goal. In preclinical pancreatic cancer models, cetuximab with gemcitabine and radiation resulted in greater growth inhibition than either therapy alone both in vitro and in vivo (70). In head and neck cancer, the addition of cetuximab to radiation therapy significantly improves both locoregional control and survival (71). Thus, several investigations of cetuximab with concurrent radiation therapy are underway in pancreatic cancer, including a German study of cetuximab with gemcitabine and IMRT (72) and an adjuvant ECOG study of capecitabine with cetuximab and radiation therapy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree