CHAPTER 124 Other Diseases of the Colon and Rectum
LYMPHOCYTIC AND COLLAGENOUS COLITIS
BACKGROUND
The term collagenous colitis was used first in 1976 by Lindstrom to describe the findings in a middle-aged woman with chronic diarrhea in whom evaluation was normal except for colonic biopsies that showed a thickened band of subepithelial collagen and increased lymphocytes in the lamina propria.1 Histologically, the subepithelial collagen deposits resembled those in the small intestine of patients with collagenous sprue. The term microscopic colitis was used first in 1980 by Read and associates, who detailed a group of patients with chronic idiopathic diarrhea, a subset of which had a normal-appearing colon at colonoscopy but abnormal histopathology on biopsy.2 Subsequent review showed that most of these patients had collagenous colitis, but some had increased lymphocytes in the lamina propria in the absence of a thickened collagen band. The term lymphocytic colitis was proposed in 1989 by Lazenby and associates3 as a more-specific histopathologic diagnosis to distinguish this entity from patterns of microscopic colitis in which other cellular elements such as eosinophils, mast cells, or neutrophils predominate.
EPIDEMIOLOGY
Collagenous and lymphocytic colitis occur most commonly between ages 50 and 70 years. Both have a strong female predominance and frequent association with arthritis, celiac disease, and autoimmune disorders. In a large population-based study in Spain, the demographic features of collagenous and lymphocytic colitis were similar: The disorders were found in 9.5 of every 100 patients with chronic watery diarrhea and normal-appearing mucosa on colonoscopy, of whom 61% had lymphocytic colitis; the incidence rates in the general population of lymphocytic colitis and collagenous colitis were 3.1/100,000 and 1.1/100,000, respectively.4 This latter observation contrasts strikingly with published reports of more than 400 cases of collagenous colitis compared with more than 60 cases of lymphocytic colitis, a finding that suggests there may be a publication bias to explain the discrepancy. The overall mean annual incidence of both colitides was 4.2 per 100,000 inhabitants in Spain, similar to the rates from an epidemiologic study conducted in Sweden5 but lower than the 8.6 cases for 100,000 person years in the United States.6 Although the incidence of these microscopic colitides clearly is higher in older age groups, both entities have been reported in children and teenagers, in whom the clinical presentation is similar to that of adults.
PATHOLOGY
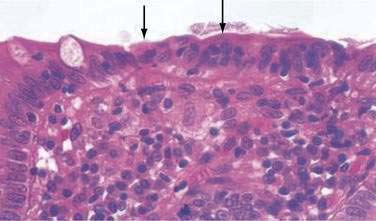
In both collagenous and lymphocytic colitis, there is a modest increase of mononuclear cells within the lamina propria and between crypt epithelial cells, consisting mainly of CD8+ T lymphocytes, plasma cells, and macrophages.3 There may be flattening of the surface epithelial cells, a mild decrease in the number of goblet cells, hyperplasia of Paneth cells, and an increased number of intraepithelial lymphocytes (Fig. 124-1). Neutrophils are not prominent, and cryptitis and crypt distortion are unusual.
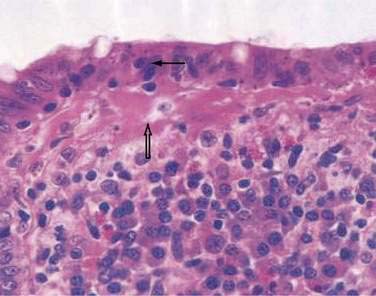
In collagenous colitis, there is a thickened subepithelial collagen layer, which may be continuous or patchy (Fig. 124-2). In normal colon, the width of this collagen band is less than 4 to 5 µm and consists predominantly of type IV collagen, whereas in collagenous colitis, it is greater than 10 µm, averages 20 to 60 µm,7 and is composed of type VI collagen and tenascin as well as lesser amounts of types I and III collagen. Tenascin is a glycoprotein that is a marker of matrix remodeling and is a product of intestinal subepithelial myofibroblasts.8 These changes are absent in lymphocytic colitis and suggest that the two main forms of microscopic colitis should be considered as separate disease entities.
Although inflammatory changes occur diffusely throughout the colon in collagenous colitis, the characteristic collagen band thickening is highly variable, occurring in the cecum and transverse colon in more than 80% of cases and in the rectum in less than 30% of cases. Although involvement of the left colon appears to be less intense than involvement of the right colon, multiple biopsies of the left colon taken above the rectosigmoid during flexible sigmoidoscopy are sufficient to make the diagnosis in approximately 90% of cases.7 The diagnosis of collagenous colitis requires both mucosal inflammation and a thickened collagen band; artifact resulting from poor orientation can give the mistaken appearance of a thickened basement membrane. It has been suggested that tenascin immunohistochemistry be used as a routine test in the diagnosis of microscopic colitis.8
ETIOLOGY AND PATHOGENESIS
The cause(s) of collagenous and lymphocytic colitis is (are) unknown. The most widely held hypothesis is that they are inflammatory disorders arising from epithelial immune responses to intraluminal dietary or bacterial contents. This hypothesis is supported by the regression of inflammation following diversion of the fecal stream and recurrence of inflammation following restoration of intestinal continuity in three patients.9 The identity of the inciting antigenic factors is uncertain, although medications,10,11 bile salts, toxins, and infectious agents12 have been postulated.
The strong association of rheumatologic diseases with microscopic colitis has raised the possibility that nonsteroidal anti-inflammatory drugs (NSAIDs) might play an etiologic role. One well-controlled study13 found that chronic NSAID use occurred more frequently in patients with collagenous colitis than in age- and gender-matched controls (61% vs. 13%; P < 0.02), a finding confirmed by a case-control study.10 One postulated mechanism by which NSAIDs might damage the colon is by increasing colonic permeability to allow luminal antigens to enter the lamina propria and promote inflammation. Other medications implicated include selective serotonin reuptake inhibitors (SSRIs), specifically sertraline, for collagenous colitis; and SSRIs, beta-blockers, statins, and bisphosphonates for lymphocytic colitis.10 Because many patients with collagenous or lymphocytic colitis have not used these medications, and because use of these drugs in older adults is common but these disorders are uncommon, other causes have been invoked, including genetic susceptibility. Genetic susceptibility is supported by the finding that 12% of patients with microscopic colitis have a family history of inflammatory bowel disease (IBD).11
Approximately 20% to 30% of patients with celiac disease have been reported to have lymphocytic colitis, raising the possibility of similar pathogenetic mechanisms.14 In one study, 40% of patients with collagenous colitis had small intestinal biopsies that were compatible with celiac disease,15 although in another study, the frequency of celiac disease was only 2% of 45 patients with collagenous colitis16 and 9% of 199 patients with lymphocytic colitis.11 Furthermore, patients with microscopic colitis do not respond to a gluten-free diet, and neither collagenous nor lymphocytic colitis is associated with human leukocyte antigens (HLAs) B8 and DR3, as is celiac disease. Finally, CD8+ T intraepithelial cells are predominant in both collagenous and lymphocytic colitis, in contrast to celiac disease, in which CD3 and CD8 predominate.
Because autoimmune disorders such as arthritis and thyroid abnormalities have been described in patients with collagenous and lymphocytic colitis,11 there have been continued efforts to associate microscopic colitis with various autoimmune HLA haplotypes and serum markers. One small study showed that HLA-A1 antigens were expressed with increased frequency in lymphocytic but not collagenous colitis,17 and another study showed similar abnormal expressions of HLA-DR antigens by mucosal epithelial cells in both conditions.18 Whether such abnormalities are the cause or the result of these disorders is unknown. Another study found similarities in HLA-DQ loci between patients with celiac disease and patients with either collagenous or lymphocytic colitis.19 Although gluten is not the inciting antigen in microscopic colitis, similar immune mechanisms may be involved in celiac disease and microscopic colitis.
The pathogenesis of the increased collagen band in collagenous colitis is unclear. Initially, it had been assumed that collagen synthesis is increased,1 but colonic biopsies from patients with the disease showed decreased levels of interstitial collagenase, suggesting that reduced matrix degradation might contribute to the accumulation of matrix proteins.20
The mechanism of diarrhea in microscopic colitis is related to the severity of inflammation and not the extent or thickness of the collagen band. Perfusion studies have demonstrated defective active and passive absorption of sodium and chloride and reduced chloride-bicarbonate exchange in the colon21; two of six subjects had coexisting abnormalities of small intestinal fluid and electrolyte absorption. Other investigations have correlated colonic fluid absorption with the severity of inflammation.22 A potential role for soluble mediators is suggested by a report that diarrhea was resolved by a histamine H1 antagonist in a patient with microscopic colitis characterized by increased numbers of mast cells.23 It has been suggested that bile acid malabsorption might contribute to diarrhea in patients with collagenous colitis and that treatment with a bile acid-binding resin such as cholestyramine might lead to a reduction in diarrhea. Bile acids are unlikely to cause the histologic changes observed in collagenous colitis, however, and a reduction in diarrhea with cholestyramine was not associated with a decrease in colitis. Successful treatment of collagenous colitis with budesonide, however, was associated with increased bile acid absorption and normalization of the 75SeHCAT (selenium-75–labeled homocholyltaurine) test for bile acid malabsorption.24
CLINICAL AND LABORATORY FEATURES
Patients with collagenous and lymphocytic colitis usually present with chronic watery diarrhea, with an average of eight stools each day ranging in volume from 300 to 1700 g per 24 hours21 and associated with occasional fecal incontinence and abdominal cramps. Symptoms decrease with fasting.5 Nausea, weight loss, and fecal urgency are variably present. Diarrhea generally is long-standing, lasting from months to years, with a fluctuating course of remissions and exacerbations. In one series of 172 patients, the median time from the onset of symptoms to diagnosis was 11 months,16 whereas in another smaller series, the median time to diagnosis was 5.4 years.25 Physical examination usually is unremarkable, and blood is not detected in the stool. Routine laboratory studies also are normal.
Examination of fresh stools showed fecal leukocytes in 55% of 116 patients with collagenous colitis.16 Mild steatorrhea, mild anemia, low serum vitamin B12 levels, and hypoalbuminemia have been reported in varying numbers of patients and are not characteristic. Autoimmune markers that have been identified in patients with collagenous colitis include antinuclear antibodies (in up to 50%), perinuclear antineutrophil cytoplasmic antibodies (pANCAs) (in 14%), rheumatoid factor, and increased C3 and C4 complement levels,22 but none of these markers is of diagnostic value.
Colonoscopic examination usually is normal. Nonspecific abnormalities including patchy edema, erythema, friability, and an abnormal vascular pattern were reported in one study,26 whereas mucosal lacerations in the ascending and transverse colons have been reported in a few patients with collagenous colitis.27
TREATMENT
There have been few controlled trials of treatment for either collagenous or lymphocytic colitis, and therapy is largely empiric. Evaluation of therapy is difficult, because both disorders usually exhibit a relapsing and remitting course over many years. No single agent works in all cases.28
About one third of patients respond to antidiarrheal agents, such as loperamide or diphenoxylate with atropine, as well as bulking agents such as psyllium or methylcellulose; clinical response is not associated with improvement of inflammation or collagen thickness. In an open-label trial of bismuth subsalicylate (eight chewable tablets per day for eight weeks) in 12 patients, diarrhea resolved and stool weight was reduced within two weeks; in nine patients colitis resolved with disappearance of the collagen band thickening.29 Over a seven- to 28-month follow-up, nine patients remained well, two were well but required retreatment, and one had persistent diarrhea. Both collagenous and lymphocytic colitis responded similarly, and there were no side effects of treatment; a subsequent controlled trial by the same investigators published only in abstract form confirmed these findings. Although the basis for its efficacy is unknown, bismuth subsalicylate possesses antidiarrheal, antibacterial, and anti-inflammatory properties; bismuth enemas have been reported to be effective in ulcerative colitis and chronic pouchitis.30
Other treatment trials for collagenous and lymphocytic colitis have studied 5-aminosalicylate (mesalamine) compounds, glucocorticoids, and bile acid resins, alone or in combination; these agents appear to improve diarrhea and inflammation in some, but certainly not all, patients.28 Although glucocorticoids given by either the oral or the rectal route provide symptomatic improvement and decrease inflammation in more than 80% of cases, relapse usually occurs quickly after the drug is stopped.5,31 Moreover, long-term use of glucocorticoids has undesirable effects, especially in older patients. Other immunosuppressants, such as azathioprine and 6-mercaptopurine, have been reported to be effective, but there are no sizable studies using these agents.29,32
Budesonide has been reported to be highly effective over a six- to eight-week period in three placebo-controlled trials in patients with collagenous colitis.33–35 Budesonide is a topically acting synthetic corticosteroid with both a high receptor-binding affinity in the mucosa and a high first-pass effect in the liver. In view of its proven efficacy, budesonide should be considered over 5-aminosalicylates or bile acid resins in patients who do not respond to antidiarrheal agents and bismuth subsalicylate.36,37
The only report of surgery for collagenous colitis involved nine patients who underwent ileostomy for disabling refractory collagenous colitis, after which all had symptomatic and histologic remission.28 In patients in whom intestinal continuity was restored, the disease recurred, and of three patients who underwent proctocolectomy with ileal pouch-anal anastomosis, problematic diarrhea occurred. Ileostomy should be considered only as a last resort, but it appears to be effective in patients with disabling and refractory symptoms.
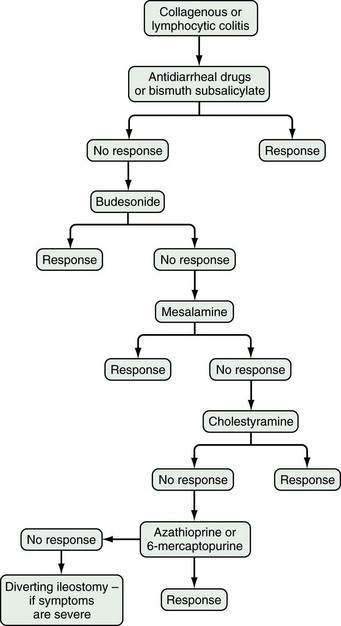
Based on available data, the treatment algorithm shown in Figure 124-3 is proposed.
DIVERSION COLITIS
BACKGROUND AND EPIDEMIOLOGY
Diversion colitis is an inflammatory process that occurs in the diverted segment of colon and rectum after surgical diversion of the fecal stream. The entity was first reported in 1981 by Glotzer and colleagues in 10 patients who had undergone ileostomy or colostomy for various indications other than IBD.38 Since then, diversion colitis has been found in patients who have undergone surgical diversion for many indications, although it has been reported to occur more commonly in patients with IBD (87%) than in those with noninflammatory conditions (28%).39,40 The prevalence of diversion colitis has been underestimated because many patients are asymptomatic, even though histologic changes are likely to occur in diverted segments of the colon within months of surgical diversion.
PATHOLOGY
A spectrum of histologic changes has been described in diversion colitis, ranging from lymphoid follicular hyperplasia and mixed mononuclear and neutrophilic infiltration to severe inflammation with crypt abscesses, mucin granulomas, and Paneth cell metaplasia41,42; however, large ulcers and transmural changes are absent and crypt architecture generally is preserved. Endoscopic findings include erythema, friability, nodularity, edema, aphthous ulcerations, exudates, and frank bleeding, as in idiopathic IBD. After extended periods following diversion, inflammatory pseudopolyps and strictures can develop.
PATHOGENESIS
Diversion colitis appears to be caused largely by luminal nutrient deficiency of the colonic epithelium. The principal nutrient substrates of the colonocytes are luminal short-chain fatty acids (SCFAs), which are metabolic products of carbohydrate and peptide fermentation by anaerobic bacteria.43,44 Roediger demonstrated that SCFAs are the major and preferred energy source for colonic epithelium and that the distal colon is more dependent on SCFAs for its metabolic needs than is the proximal colon.45 Butyrate supplies the bulk of oxidative energy to the distal colon, and acetate, glutamine, and ketones provide alternative sources of energy. Harig and associates demonstrated that the excluded segments of colon contain negligible amounts of SCFAs and that infusion of glucose results in no appreciable anaerobic fermentation.46 The number of obligate anaerobes is reduced in the excluded colon, consistent with reduced production of SCFAs.47 Further support for the SCFA nutrient deficiency hypothesis is from the report that instillation of enemas containing SCFAs resulted in disappearance of endoscopic changes within four to six weeks in four patients with diversion colitis, although resolution of histologic abnormalities was slower and incomplete.46
Although SCFA deficiency has been widely accepted as the cause of diversion colitis, other observations suggest that this might not be the entire etiologic explanation. First, studies in children indicate that SCFA enemas are not universally successful in treating diversion colitis.48 Second, in germ-free rodents with surgical diversion and in patients receiving long-term parenteral nutrition or elimination diets (circumstances in which luminal SCFA concentrations are low), mucosal atrophy occurs rather than inflammation.49 Third, inflammation does not occur in urinary colon conduits from which the fecal stream has been diverted, and urine does not contain measurable SCFAs.50 Finally, in a prospective, randomized, double-blind study of 13 patients with diversion colitis, butyrate enemas given for 14 days provided no improvement in either endoscopic or histologic parameters.51 In a subsequent study by the same group, administration of SCFAs did not affect the bacterial population in the excluded colon.52 Other luminal elements besides SCFA deficiency are likely to play a role, but the nature of such factors is unknown.
DIAGNOSIS
The diagnosis of diversion colitis is based on the clinical picture, endoscopic findings, and histology. Diagnosis is relatively straightforward in a patient without preexisting IBD, and stool specimens for C. difficile toxin,53 ova and parasites, and cultures usually are adequate to exclude other etiologies.
In patients with a preoperative diagnosis of Crohn’s disease, diversion colitis must be distinguished from recurrent IBD. Colonoscopic findings such as linear ulcers and possibly strictures are said to favor Crohn’s disease, as do transmural inflammation, marked crypt architectural abnormalities, and epithelioid granulomas.39 Lymphoid hyperplasia occurs in both disorders but tends to be more prominent in diversion colitis.54 If rectal involvement with Crohn’s disease is absent before diversion, rectal inflammation is more likely to be caused by diversion than Crohn’s disease.2,39,55
TREATMENT
The preferred treatment of diversion colitis is surgical restoration of colonic continuity, which rapidly reverses symptoms and histologic changes. If symptoms are moderate to severe and reanastomosis is not feasible, SCFA enemas in a volume of 60 mL and containing a mixture of 60 mmol/L of acetate, 30 mmol/L of propionate, and 40 mmol/L of butyrate with 22 mmol/L of sodium chloride per liter are administered through the anus or mucous fistula twice daily for four weeks and then decreased to once or twice weekly.46 Such preparations are not commercially available and must be formulated by compounding pharmacies, making it the most expensive of the nonsurgical options.56 There are anecdotal reports that 5-aminosalicylate and hydrocortisone retention enemas are effective as well.57 Because they are available commercially, these agents are considered first-line therapies for most patients. One report suggested that intraluminal irrigation with soluble and insoluble fiber solutions improved endoscopic and histologic abnormalities and might be useful to reduce inflammation before surgical restoration of bowel continuity.58
NONSPECIFIC COLONIC ULCERS
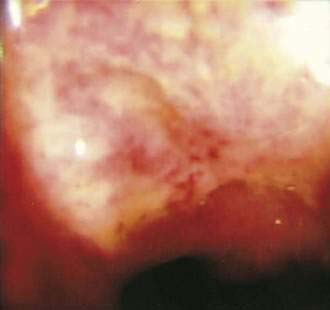
Benign nonspecific ulcers of the colon are uncommon. The most recent large review of the literature encompassed 127 patients and indicated that such nonspecific ulcers occur at any age, with a peak incidence in the 4th and 5th decades and a slight female predominance.59 Most of these ulcers occur in the proximal colon, virtually all are solitary and located on the antimesenteric side of the colon, and most are round and sharply demarcated from relatively normal surrounding mucosa (Fig. 124-4).59,60 Histologically, there is nonspecific acute and chronic inflammation.59
PATHOGENESIS
The causes of nonspecific colonic ulcers are unknown. Potential etiologies that have been suggested, albeit with little or no supporting evidence, include ischemia and cecal diverticulosis. Correlations with the use of drugs such as glucocorticoids, NSAIDs,61,62 oral contraceptives, and oxyphenbutazone have been suggested, but cause has not been established and these drugs have not been implicated in most of the ulcer cases reported. It is likely that no single causative agent explains all cases. There have been reports of associations of nonspecific colon ulcers with chronic renal failure and renal transplantation,63 Churg-Strauss syndrome,64 Wegener’s granulomatosis,65 Behçet’s disease, essential mixed cryoglobulinemia,66 and systemic lupus erythematosus. Perhaps a mechanism common to all exists, but none has yet been identified.
CLINICAL FEATURES
The most common presenting symptoms are abdominal pain and bleeding. More than half of patients with nonspecific colon ulcers present with acute or chronic abdominal pain, often in the right lower abdomen and mimicking appendicitis.59 One third have lower gastrointestinal bleeding with hematochezia, and 16% present with an abdominal mass, most often when the ulcer is located in the left or sigmoid colon. A cecal ulcer should be suspected in a patient with gastrointestinal bleeding when the clinical picture is otherwise consistent with appendicitis or in a patient with symptoms suggesting pelvic inflammatory disease, ovarian disease, or Crohn’s disease in the absence of these diseases.
DIAGNOSIS
Colonoscopy currently is the diagnostic test of choice.54 Flexible sigmoidoscopy is inadequate because most colonic ulcers are beyond the reach of the instrument. Abnormalities have been described in up to 75% of air-contrast barium enemas59 and include mucosal irregularities, intraluminal filling defects or narrowing, a mass effect, or localized colonic spasm (Fig. 124-5). Roentgen findings are nonspecific, however, and are diagnostically inferior to direct inspection by colonoscopy. Computed tomographic (CT) scans are most helpful in the presence of perforation or associated abscess formation.

Figure 124-5. Nonspecific ulcer of the colon. Film from a barium enema examination showing the lesion in Figure 124-4 (arrow). The initial interpretation was carcinoma of the ascending colon.
TREATMENT
Surgery is recommended for patients with ulcers complicated by perforation or by significant gastrointestinal bleeding and for those with persistent symptoms and failure of the ulcer to heal. In uncomplicated cases, however, an expectant approach has been advocated, with colonoscopy every six weeks to monitor healing. The most common surgical procedures are local excision of the ulcer, oversewing of the ulcer if there is significant bleeding, and occasionally, segmental colectomy.54,67
NSAID-INDUCED COLONIC LESIONS
In contrast to nonspecific colonic ulcers, lesions that are now considered to be pathognomonic for NSAID-induced colitis are known as diaphragm disease68 of the colon. Although it is well known that small bowel strictures are associated with use of NSAIDs, only a small number of cases have been reported since their first published description in 1989.69 The presence of diaphragms with ulcers distinguish these lesions from other nonspecific ulcers.
It is believed that the diaphragm-like strictures are due to scarring following an ulcerating injury. Strictures are concentric, often with a pinhole-size lumen. Lesions in the colon are similar to those found in the small intestine (see Chapter 115). The mucosa between diaphragms (if multiple) is normal. Strictures are characterized by submucosal fibrosis with normal overlying epithelium.
PATHOGENESIS
The pathogenesis of these uncommon lesions is unknown but is thought to involve direct contact of the NSAID with colonic mucosa. The vast majority of cases involve oral intake of NSAIDs, and most of the patients in one study were known to have taken extended-release formulations.68 Half had used diclofenac, and most patients had lesions in the proximal colon. The injury is presumed to involve a high local concentration of active NSAID, which increases intestinal permeability, a prerequisite for NSAID-induced enterocolopathy. This is in contrast to gastroduodenal injury, which is thought to be mediated more often by systemic effects. Postulated mechanisms of injury include prostaglandin inhibition alterations in mucosal blood flow and increased permeability to injurious luminal substances. The risk of lower gastrointestinal toxicity is reduced by the use of selective COX-2 inhibitors.70
CLINICAL FEATURES
The most common clinical presentations include occult blood in the stool, iron-deficiency anemia or frank bleeding, abdominal pain, or change in bowel habits. Other findings can include intermittent bowel obstruction, diarrhea, or colonic perforation with an acute abdomen. Many patients have an underlying rheumatologic disorder and have been using NSAIDs chronically, although lesions have been reported after using NSAIDs for only a few days.71
DIAGNOSIS
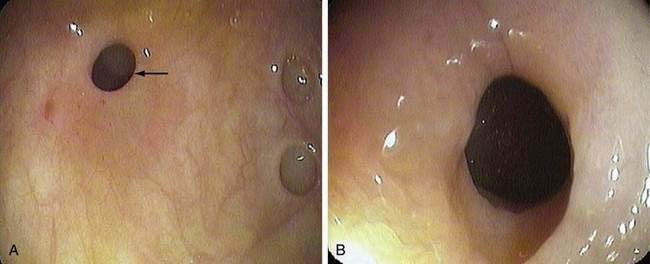
As with nonspecific colonic ulcers, colonoscopy is currently the diagnostic test of choice; flexible sigmoidoscopy is inadequate because most diaphragm disease colon ulcers are proximal to the descending colon (Fig. 124-6). Whereas the differential diagnosis of nonspecific colonic ulcers and NSAID-associated colitis and erosions is broad, the presence of characteristic diaphragmatic webs with normal intervening mucosa in a setting of NSAID use is virtually pathognomonic.
TREATMENT
For nonstricturing NSAID lesions, discontinuing the NSAID often is curative and is essential to management; obstructive symptoms associated with strictures, however, require more-aggressive management. For strictures that are easily accessible, endoscopic dilation with a through-the-scope (TTS) balloon has been reported to be safe and effective.72 If endoscopic dilation is not possible, the area should be marked endoscopically to guide the surgeon, because there may be no serosal abnormalities or palpable areas of transition to guide resection. Surgery also is indicated for significant bleeding or perforation and when carcinoma cannot be excluded with confidence.
DIEULAFOY-TYPE COLONIC ULCERATION
In 1897, Georges Dieulafoy described massive gastrointestinal bleeding emanating from a relatively enlarged (“persistent calibre”) submucosal artery by way of a minute mucosal ulcer at the most superficial point of the vessel.73 Although originally described in the stomach and most commonly occurring in the gastric fundus, identical lesions have been described in other gastrointestinal organs, including the colon and rectum.74–76 In the colon, Dieulafoy-type lesions appear to have a strong male predominance and have been reported in all age groups.
The clinical picture is one of acute and massive bleeding. Colonoscopy can identify the lesion in some cases, but in most cases identification is often difficult or impossible, especially when bleeding continues or thorough cleansing of the colon cannot be accomplished. Selective mesenteric angiography is the diagnostic study of choice, and surgical resection has been the principal form of therapy. Even after angiographic detection of the bleeding site, precise localization of the lesion is usually difficult, and extended resection often is required. In some cases, colonic lesions appear as pseudopolyps,74 and successful treatment with sclerotherapy, electrocautery, or endoscopic hemoclipping might obviate the need for surgery.76,77
CATHARTIC COLON
Cathartic colon is an uncommon and severe sequela of chronic irritant laxative abuse. In 1943, Heilbrun first described radiologic abnormalities of the colon and terminal ileum associated with prolonged abuse of irritant cathartics.78 Fewer than 50 cases have been reported in the literature, all in women with a duration of laxative abuse ranging from 10 to 70 years. It is important to emphasize that the term cathartic colon is based on barium enema characteristics and is not synonymous with prolonged use of laxatives or with laxative abuse. Indeed, misuse of the term cathartic colon has led to inappropriate concerns over the chronic use of laxatives which, when appropriate, is not associated with structural or functional damage to the colon. Cathartic colon is not the inevitable consequence of chronic laxative abuse, which may be associated with a variety of reversible symptoms as well as fluid and electrolyte abnormalities. In a review of 240 cases of chronic laxative abuse published in more than 70 reports, no case of cathartic colon was demonstrated.79,80
RADIOLOGIC AND PATHOLOGIC FEATURES
Heilbrun originally described the following characteristics in his original case report: loss of haustrations, pseudostrictures, dilated colon and terminal ileum, and gaping of the ileocecal valve78; similarity to the radiologic appearance of chronic ulcerative colitis was noted in this and subsequent studies. Characteristic changes are not always found throughout the colon, and there is a predilection for involvement of the ascending colon. Pathologic changes in resected specimens of cathartic colon have included mucosal atrophy, chronic inflammation with thickening of the muscularis mucosae, submucosal fatty infiltration, and mild fibrosis. Irreversible strictures and degenerative changes in intestinal neurons are absent. Neuronal changes have been found in patients with chronic laxative abuse, but these patients did not exhibit cathartic colon as defined here.81
CHANGING ROLE OF LAXATIVES IN COLON DAMAGE
The original suggestion that irritant laxatives, predominantly anthraquinones, damage the colon was based on studies in laboratory animals and in colons resected from laxative abusers.82 Although mucosal atrophy and abnormalities of the enteric nervous system were described, the identities of the laxatives were not documented, nor was there information concerning preexisting conditions that might have prompted chronic use of laxatives.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree