Accurate lymph node staging in genitourinary (GU) malignancies is important for planning an appropriate treatment and establishing an accurate prognosis. This article discusses the novel imaging techniques for detection of metastases in various GU malignancies, including prostate, bladder, penile, and testicular cancers. Discussion includes nuclear medicine techniques of 18 F-fluorodeoxyglucose positron emission tomography/computed tomography (PET/CT), 11 C-choline and 18 F-choline PET/CT, and ProstaScint scanning, as well as sentinel lymph node mapping. Magnetic resonance (MR) techniques include lymphotropic nanoparticle-enhanced MR imaging and diffusion-weighted MR imaging.
Precise lymph node staging in genitourinary (GU) malignancies is crucial for planning an appropriate treatment and establishing an accurate prognosis. Computed tomography (CT) is a widely used tool for initial evaluation of the nodal involvement. According to the accepted size criteria, any node with a short-axis diameter greater than 1 cm and any rounded node larger than 8 mm is concerning for malignancy. However, as nodal evaluation on CT relies solely on nodal size rather than on nodal function and physiology, this method is limited in its accuracy, as small nodes may harbor micrometastases and enlarged lymph nodes may be reactive in nature. Improvement in preoperative diagnosis of nodal metastases is crucial, as micrometastases may be present in up to 25% of patients with clinically organ-confound prostate cancer. Multiple novel techniques are emerging to improve the accuracy of nodal involvement in GU malignancies.
Positron emission tomography
Positron emission tomography (PET) scanning using 18 F-fluoro-2-deoxyglucose (FDG) has been shown to be an effective tool for nodal detection of some malignancies, such as small cell lung cancer. 18 F-FDG is phosphorylated to FDG-6-phosphate (FDG-6P) and is accumulated in cells with increased rates of glycolysis. Tissues with elevated metabolic rates accumulate FDG-6P, and thus can be detected on PET scanning. 18 F-FDG PET has been shown to be a useful tool in differentiating fibrotic residual mass in seminomatous germ cell tumors on restaging. However, 18 F-FDG PET has a low sensitivity and accuracy in staging prostate cancer, likely due to the low rates of accumulation of the tracer in the prostate cancer cells. In addition, as FDG is eliminated by kidneys, the excreted FDG activity accumulating in the ureters and bladder may limit the evaluation of adjacent structures such as the prostate and pelvic lymph nodes.
As with prostate cancer, the use of 18 F-FDG PET for staging of bladder cancer is hindered by urinary excretion of the tracer. For instance, Heicappell and colleagues demonstrated a 66.7% detection rate for local lymph node metastasis of bladder cancer; Lodde and colleagues demonstrated sensitivity of 57%. Moreover, in a study of 51 patients with patients with nonmetastatic invasive bladder cancer (T2 or higher, M0) or recurrent high-risk superficial disease (T1G3 with or without Tis, M0), Swinnen and colleagues found the accuracy, sensitivity, and specificity for the diagnosis of node-positive disease of 18 F-FDG PET/CT to be 84%, 46%, and 97%, respectively. Thus, the investigators concluded that FDG-PET/CT had no advantage over conventional CT, which in their study had an accuracy of 80%, sensitivity of 46%, and specificity of 92%. Although the sensitivity of 18 F-FDG PET is suboptimal, multiple studies have demonstrated high specificity for detection of nodal involvement. Similar to the high specificity (97%) demonstrated by Swinnen’s group, Jensen and colleagues found high specificity of 93.3% when evaluating 18 F-FDG PET for preoperative staging of bladder cancer. In attempts to improving 18 F-FDG PET performance for bladder cancer, Anjos and colleagues added 1-hour delayed images after furosemide injection. While clearing the tracer from the urinary system allowed detection of recurrent bladder lesions in an additional 6 (35%) of 17 patients, additional metastatic lymph nodes on the delayed images were seen only in 2 (12%) of 17 patients. Although sensitivity of 18 F-FDG PET for detecting nodal involvement in bladder cancer is somewhat disappointing, it still may be a useful prognostic study. For instance, in 40 patients with bladder carcinoma evaluated by Drieskens and colleagues, median survival time of patients with nodal and/or distant metastases on 18 F-FDG PET/CT was 13.5 months, compared with 32 months in the patients with negative 18 F-FDG PET/CT, with P <.004.
Addition of CT to the PET acquisition improves anatomic localization of abnormal PET activity, and the combination of 18 F-FDG PET and CT was shown to be very accurate in detecting pelvic nodal metastases in the setting of penile carcinoma, with reported sensitivity of 88.2% to 91%, specificity of 98.1% to 100%, positive predictive value of 93.8% to 100%, and negative predictive value of 94% to 96.3%.
Similarly high performance of 18 F-FDG PET/CT has been shown in detection of testicular cancer metastases with reported sensitivity, specificity, positive predictive value, and negative predictive value of 93.3%, 97%, 93.3%, and 97%, respectively. 18 F-FDG PET has also been shown to be a useful tool in evaluation of residual disease in patients with metastatic nonseminomatous germ cell tumors (GCT). Kollmannsberger and colleagues compared the ability of 18 F-FDG PET to predict the viability of 85 residual masses in 45 patients with nonseminomatous GCT after chemotherapy with that of CT and tumor marker changes. The investigators found that 18 F-FDG PET had higher sensitivity for predicting a viable residual tumor (59%) than CT and tumor marker changes (sensitivities of 55% and 42%, respectively), and specificity higher than that of CT (92% vs 86%, respectively) but less than that of tumor marker changes (92% vs 100%, respectively). Similar results were demonstrated by Pfannenberg and colleagues, who evaluated 60 residual masses following high-dose chemotherapy in 28 patients with metastatic GCT. The investigators found no difference in sensitivity for prediction of viability of residual masses between 18 F-FDG PET, CT/magnetic resonance imaging (MRI), and tumor marker levels (sensitivities of 70%, 62%, and 69%, respectively), but specificity of 18 F-FDG PET (83%) was higher than that of CT/MRI (72%) but lower than that of tumor marker levels (88%). In addition, combination of all 3 modalities resulted in very high sensitivity (93%) and specificity (100%) for predicting viable residual disease. The investigators concluded that positive 18 F-FDG PET results are highly correlated with the presence of viable residual tumor, but residual masses with negative PET findings still require resection. When tumor progression is established by CT and elevated tumor markers, additional 18 F-FDG PET seems to be of no significant benefit, but in patients with stable disease or partial remission in CT/MRI and normalized tumor markers as well as in marker-negative disease, 18 F-FDG PET is a useful diagnostic adjunct.
In addition to being able to predict presence of a viable residual disease in patients with metastatic GCT, 18 F-FDG PET has been demonstrated to be a useful tool for early prediction of treatment response to high-dose salvage chemotherapy in patients with relapsed GCT. The clinical course of disease after high-dose salvage chemotherapy was correctly predicted by 18 F-FDG PET during chemotherapy in 21 of 23 (91%) patients. All 7 (100%) of patients who had a negative 18 F-FDG PET after initial part of treatment remained disease-free after completion of the full treatment regimen, whereas 14 of 16 (88%) patients with positive 18 F-FDG PET relapsed within 6 months following completion of chemotherapy regimen, or the histology of the resected residual mass after the chemotherapy still revealed the presence of viable carcinoma. Thus, sensitivity and specificity of 18 F-FDG PET for the prediction of the overall failure of salvage chemotherapy were 100% and 78%, respectively, with the positive predictive and negative predictive values being 88% and 100%, respectively.
11 C-Choline is a radiopharmaceutical for PET imaging that may be a preferred tracer for prostate and bladder cancer, as it lacks the urinary radioactivity seen with 18 F-FDG. Choline is one of the components of phosphatidylcholine, an essential element of phospholipids in the cell membrane. Malignant tumors show a high proliferation and increased metabolism of cell membrane components that will lead to an increased uptake of choline. de Jong and colleagues calculated a sensitivity of 11 C-choline PET for staging metastatic lymph node disease in patients with prostate cancer of 80%, a specificity of 96%, and an accuracy of 93%. In addition, 11 C-choline PET detected solitary extraregional lymph node metastases in 5 of 12 patients with nodal metastases. Similarly, in patients with bladder cancer, 11 C-choline PET was demonstrated to have a higher accuracy for detection of nodal metastases compared with contrast-enhanced CT (89% vs 82%, P <.01).
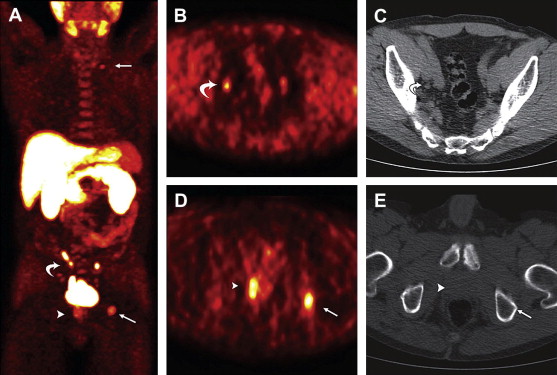
While demonstrating high potential accuracy, the use of 11 C-choline tracer is limited because of its short half-life, requiring a cyclotron to be in close proximity to the hospital. Labeling choline with the radioactive isotope 18 F could avoid this issue. 18 F-Choline accumulates in metabolically active cells and therefore can be detected on PET/CT ( Fig. 1 ). In their study of 132 patients with prostate cancer, Beheshti and colleagues found per-patient sensitivity and specificity of 18 F-choline PET/CT, in detection of malignant lymph nodes, to be 45% and 96%, respectively. Positive and negative predictive values were 82% and 92%, respectively.
Single-photon emission computed tomographic imaging
In addition to changes in metabolism, malignant cells express tumor-specific antigens. Single-photon emission computed tomographic (SPECT) imaging uses radioactive-labeled antibodies against such antigens. Indium-111 capromab pendetide (ProstaScint) is a radioactively labeled monoclonal antibody directed against the intracellular portion of the prostate-specific membrane antigen, a glycoprotein that is expressed by the prostate epithelium and is upregulated in (metastatic) prostate cancer. Polascik and colleagues reported ProstaScint scanning to detect 62% of pathologically proven metastatic lymph nodes. The investigators demonstrated that addition of a ProstaScint scan to the clinical predictive algorithms improves selection of candidates for definitive local therapy in men with clinically localized prostate carcinoma and significant risk of lymph node involvement. In high-risk patients evaluated for risk of lymph node metastases prior to pelvic lymph node dissection, ProstaScint scan was found to have a sensitivity of 62%, specificity of 72%, positive predictive value of 62%, and negative predictive value of 72%.
Single-photon emission computed tomographic imaging
In addition to changes in metabolism, malignant cells express tumor-specific antigens. Single-photon emission computed tomographic (SPECT) imaging uses radioactive-labeled antibodies against such antigens. Indium-111 capromab pendetide (ProstaScint) is a radioactively labeled monoclonal antibody directed against the intracellular portion of the prostate-specific membrane antigen, a glycoprotein that is expressed by the prostate epithelium and is upregulated in (metastatic) prostate cancer. Polascik and colleagues reported ProstaScint scanning to detect 62% of pathologically proven metastatic lymph nodes. The investigators demonstrated that addition of a ProstaScint scan to the clinical predictive algorithms improves selection of candidates for definitive local therapy in men with clinically localized prostate carcinoma and significant risk of lymph node involvement. In high-risk patients evaluated for risk of lymph node metastases prior to pelvic lymph node dissection, ProstaScint scan was found to have a sensitivity of 62%, specificity of 72%, positive predictive value of 62%, and negative predictive value of 72%.
Lymphotropic nanoparticle-enhanced magnetic resonance imaging
MRI is widely used when evaluating multiple primary neoplasms of the GU tract. MRI is particularly important in pretreatment evaluation of the prostate cancer. Combination of various pulse sequences, each of which has its own strengths and weaknesses, has been demonstrated to yield an MRI examination that has a high sensitivity and specificity for detection of the prostate neoplasm as well as defining its extent. High spatial and soft-tissue resolution of MRI as well as ability to obtain images in multiple planes allows for accurate assessment of local extent of the prostate cancer, including extension through the capsule and involvement of the seminal vesicles and/or neurovascular bundles ( Figs. 2 and 3 ). MR offers a superior soft-tissue resolution compared with CT, resulting in an improved ability to assess nodal morphology, signal-intensity changes, contrast enhancement with gadolinium, and central necrosis, all of which may be helpful in assessing malignant versus benign lymphadenopathy. However, conventional MRI, as does CT, relies on nodal size and morphology for detection of nodal metastases (see Fig. 2 ), and thus demonstrates no improvement in accuracy over CT.









