Chapter 30 Natural history of gallstones and asymptomatic gallstones
History
Gallstones have been recognized since antiquity and have even been found during autopsies of Egyptian mummies. The Greek physician Trallianus described calculi within radicles of a human liver (Glenn & Grafe, 1966). Vesalius and Fallopius described gallstones in the gallbladders of dissected human bodies (Schwartz, 1981), and in 1882, Langenbuch performed the first successful cholecystectomy, setting the path for therapeutic intervention in cholelithiasis.
Epidemiology
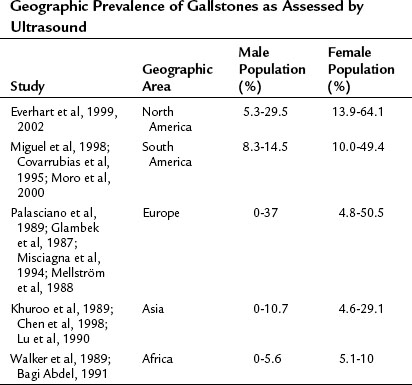
Gallstones represent a sizeable problem for the contemporary health care system in both developed and developing countries alike. In the year 2000, there were 2,624,111 admissions and 778,632 outpatient visits for gallstones in the United States. With 6.3 million affected men and 14.2 million affected women between the ages of 20 and 74 years, and at an annual cost of $6.5 billion, cholelithiasis is the most expensive digestive tract disorder today in the United States (Shaffer, 2006). Incidence of gallstones and gallstone-related operations in developed countries appears to be increasing. With an overall prevalence of 10% to 15% in developed countries, geographic-specific prevalence is from 0% to 10% in Africa and up to 60% to 70% in certain populations, such as Pima Indians; this likely reflects combined differences in environmental, dietary, and genetic factors (Shaffer, 2006). The most common type of gallstones in developed countries are composed primarily of cholesterol, and the highest incidence is in the Native American population; moderate prevalence is seen in Hispanics, and the lowest prevalence is seen in black Americans, East Asians, and sub-Saharan Africans. Increased incidence of brown-pigmented stones are noted in East Asians, reflecting a higher rate of biliary tract infections (Shaffer, 2006; see Chapter 43). More detailed information about geographic disparities in the prevalence of gallstone disease can be found in Table 30.1.
Risk Factors for Gallstones Development
Gallstone disease clearly results from a complex interaction of genetic and environmental factors. This is confirmed by an altered incidence of gallstone detection when people from diverse geographical areas travel and settle in areas with a different dietary regimen, level of physical activity, and hygiene. The common mechanisms of gallstone formation include cholesterol hypersecretion, alteration in intestinal bile salt/cholesterol absorption, and gallbladder hypokinesia, which leads to bile cholesterol supersaturation and nucleation (see Chapter 7). Bacterial infection and an increase in bilirubin load play a role in the development of black and brown gallstones. The following is a quick overview of the most common risk factors for the development of gallstones.
Age
The incidence of gallstones increases with age across all ethnic groups, and it is very low among infants and children (Chen et al, 1998). Some specific populations such as Pima Indians, mentioned previously, have an increased incidence of gallstones (up to 70%) by 30 years of age, implicating hereditary metabolic factors (Sampliner et al, 1970). Pediatric populations with chronic hemolytic conditions, such as sickle cell anemia, also represent another distinct group in whom gallstones develop early.
Gender
Female gender is a risk factor for developing gallstones, surpassing males in the incidence of gallstones and the chance of having surgery by 2 : 1 or 3 : 1 in most studies (see Table 30.1). Pregnancy is associated with up to a 30% risk of developing biliary sludge, and low-dose estrogen therapy in postmenopausal women increases the risk of gallstone formation (Maringhini, et al, 1993; Hulley et al, 1998).
Obesity, Diet, Physical Activity, and Weight Loss
Obesity is a well-established major risk factor for the development of gallstones. The association with simple obesity is important in females; in males it is mostly associated with intraabdominal (central) obesity and metabolic syndrome (Maclure et al, 1989; Heaton et al, 1991; De Santis et al, 1997; Tsai et al, 2004).
The frequency of gallstones has almost doubled in the last 60 years, in parallel with the changed composition of stones from pigment to cholesterol. In humans, most cholesterol found in gallstones is from the diet, since de novo hepatic synthesis is only about 20% (Paigen & Carey, 2002). This emphasizes the importance of high caloric and carbohydrate intake as risk factors for the development of gallstones in modern society.
Bariatric patients are at a high risk for the development of cholelithiasis after weight-reduction surgery. Sludge and gallstones form in up to 35% of patients following bariatric procedures, with weight loss more than 1.5 kg/week being a risk factor (Shiffman, et al, 1991; Weinsier et al, 1995).
Patients receiving total parenteral nutrition (TPN) are another group with a high incidence of gallstone and sludge development. After 3 months of TPN therapy, approximately 45% of patients will develop gallstones; 100% of patients will develop sludge within 6 weeks (Shaffer, 2001; Murray et al, 1992). Low levels of physical activity are associated with development of gallstones in large observational and population studies also related to obesity and diet (Leitzmann et al, 1999). Finally, patients receiving long-term somatostatin analogue therapy for various disorders (acromegaly, functional neuroendocrine tumors) are at increased risk for gallstone formation as a result of reduced gallbladder motility and reduced bile flow (Bornschein et al, 2009).
Genetics
Population studies indicate a 30% genetic component in the development of gallstone disease. Hepatic cholesterol hypersecretion, resulting in bile supersaturation and cholesterol stone formation, may be caused by increased hepatic uptake and synthesis of cholesterol, decreased hepatic synthesis of bile salts, decreased hepatic synthesis of cholesterol esters for inclusion in very-low-density lipoprotein (VLDL), and derangements in the intestinal absorption of cholesterol and bile salts. Genes controlling hepatic cholesterol metabolism have been implicated in the pathogenesis of gallstone formation in transgenic/knockout mouse models and in humans (Table 30.2). Excess cholesterol load in smooth muscles of the gallbladder can affect signaling via the cholecystokinin A (CCK-A) receptor and contribute to the development of gallstones by inducing bile stasis. Intestinal cholesterol/bile salt absorption is tightly controlled and genes responsible for cholesterol absorption (NPC1L1, Niemann-Pick C1-like protein) or cholesterol efflux (ABCG5/G8) have been implicated in the development of gallstones in certain populations because of intestinal bile salt loss. Single-gene mutations result in hemolysis and increase the incidence of black stones because of an excess of unconjugated bile acids forming polymerized calcium bilirubinate stones. A summary of genes found to be involved in gallstone pathogenesis can be found in Table 30.2 (Grünhage & Lammert, 2006).
Table 30.2 Genes Involved in Gallstone Pathogenesis
| Genes and Encoded Proteins | Mechanism | Significance in Humans |
|---|---|---|
| ABCB4, ATP binding cassette transporter B4 | Decreased biliary phospholipid secretion | + |
| ABCB11, ATP binding cassette transporter B11 | Decreased bile salts secretion | + |
| APOB, apolipoprotein B | Decreased hepatic VLDL secretion | +/? |
| APOE, apolipoprotein E | Increased intestinal cholesterol absorption, decreased bile acid secretion | +/? |
| CCKAR, cholecystokinin A receptor | Gallbladder hypomotility | ? |
| CETP, cholesteryl ester transfer protein, plasma | Increased HDL metabolism | + |
| CFTR, cystic fibrosis transmembrane conductance regulator | Increased biliary bilirubin secretion and bile salt excretion in feces, decreased bile pH | + |
| ANK1, EPB42, SPTA1, SPTB, SLC4A1, associated with hereditary spherocytosis | Increased bilirubin load | + |
| HBB, hemoglobin-β, associated with sickle cell anemia and thalassemia | Increased bilirubin load | + |
| AK1, G6PD, GPI, GSR, PGK1, PKLR, associated with erythrocyte enzyme deficiencies | Increased bilirubin load | + |
| CYP39A1, oxysterol 7-alpha-hydroxylase | Induced hypercholesterolemia | + |
| UGT1A1, Gilbert syndrome–associated protein | Increased bilirubin load | + |
NPC1L1,
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|