Minimally invasive surgery (MIS) has changed pediatric urology and general surgery, offering less morbidity and new surgical options for many procedures. This promise goes unrealized when technical methods lag. Application of MIS in children is uneven after more than 2 decades of application. Principles of versatile and proficient technique may remain unstated and implicit in surgical training, often leaving surgical training an exercise in inference and imitation. This article describes some essential practical principles of precision MIS applied to patients of any size.
Key points
- •
Do not confuse flashy technology as a substitute for precision technique, or for knowing how devices were designed to be used.
- •
Precise movement follows from specific measures that favor the surgeon’s mechanical advantage.
- •
Moving well in MIS is always a two-handed effort, in terms of coordinated motion, tension, visualization, and especially training.
- •
Precision in pediatric MIS results from a conscious rejection of the kind of movement disallowed in open surgery but often overlooked or excused in MIS.
Introduction
Minimally invasive surgery (MIS) is hard to teach. To begin with, it is hard to learn. Successful MIS originates in good, open surgical technique, but routine surgical skills translate poorly to MIS. The natural habits of humans conflict with the unfamiliar and counterintuitive methods of MIS, hampering application, and sometimes producing rotten results. The job seems even harder in small children. A child half as tall as an adult offers surgical spaces with just one-eighth the volume. Pediatric MIS can seem 8 times as difficult.
Despite skepticism about pediatric MIS, benefits are plainly demonstrated. Because MIS offers the surgeon and the pediatric patient nontrivial advantages in terms of wounds, infections, information, precision, visualization, and even speed, MIS is here to stay. MIS forms a central part of surgical training, obviating the notion of the MIS fellowship. MIS should be just another part of pediatric general, thoracic, and urologic surgery.
Nevertheless, clumsy laparoscopic technique is anything but “minimally invasive.” Perhaps this explains why reports of MIS in children often hedge with a caveat about “in skilled hands” or “in centers with adequate experience.” Ad hoc practices and imprecise maneuvers produce long anesthetic times, poor mechanical results, and return trips to the operating room. Only precision MIS lives up to the promise to help better and hurt less.
Unfortunately, typical surgical pedagogy does not prepare residents to be precise. As actually practiced, training often does not consist of transmission of principled, applied methods mastered by deliberate practice. Instead, it consists of residents absorbing surgical memes in monkey-see, monkey-do fashion. Young surgeons who do not grasp the rationale for each move simply ape poor moves poorly. Results suffer, unless luck prevails.
Surgical precision is the single critical route to patient safety in pediatric MIS. Here precision means exact achievement of the desired surgical (mechanical) objective using the most parsimonious motion. However, surgical precision will not emerge from contrived checklists or Likert scales or milestones. A surgeon might rather be lucky than good, but skill creates its own luck.
This article offers some principles of good pediatric MIS technique that can be taught and practiced. These heuristics can improve the surgeon’s mechanical advantage for any MIS case, in any size patient. Mechanical advantage (eg, improved torque, increased degrees of freedom) may seem nebulous, but it is always recognized by a peculiar sense of physical relief. The surgeon with mechanical advantage exerts less effort, makes fewer moves, feels less fatigue, and places the needle or hook exactly. Moreover, a good heuristic always contains a real verb, an observable action taking an actual object (institutional verbs do not; eg, optimize, foster, strive, endeavor, assess). Principles should apply in the real world.
Introduction
Minimally invasive surgery (MIS) is hard to teach. To begin with, it is hard to learn. Successful MIS originates in good, open surgical technique, but routine surgical skills translate poorly to MIS. The natural habits of humans conflict with the unfamiliar and counterintuitive methods of MIS, hampering application, and sometimes producing rotten results. The job seems even harder in small children. A child half as tall as an adult offers surgical spaces with just one-eighth the volume. Pediatric MIS can seem 8 times as difficult.
Despite skepticism about pediatric MIS, benefits are plainly demonstrated. Because MIS offers the surgeon and the pediatric patient nontrivial advantages in terms of wounds, infections, information, precision, visualization, and even speed, MIS is here to stay. MIS forms a central part of surgical training, obviating the notion of the MIS fellowship. MIS should be just another part of pediatric general, thoracic, and urologic surgery.
Nevertheless, clumsy laparoscopic technique is anything but “minimally invasive.” Perhaps this explains why reports of MIS in children often hedge with a caveat about “in skilled hands” or “in centers with adequate experience.” Ad hoc practices and imprecise maneuvers produce long anesthetic times, poor mechanical results, and return trips to the operating room. Only precision MIS lives up to the promise to help better and hurt less.
Unfortunately, typical surgical pedagogy does not prepare residents to be precise. As actually practiced, training often does not consist of transmission of principled, applied methods mastered by deliberate practice. Instead, it consists of residents absorbing surgical memes in monkey-see, monkey-do fashion. Young surgeons who do not grasp the rationale for each move simply ape poor moves poorly. Results suffer, unless luck prevails.
Surgical precision is the single critical route to patient safety in pediatric MIS. Here precision means exact achievement of the desired surgical (mechanical) objective using the most parsimonious motion. However, surgical precision will not emerge from contrived checklists or Likert scales or milestones. A surgeon might rather be lucky than good, but skill creates its own luck.
This article offers some principles of good pediatric MIS technique that can be taught and practiced. These heuristics can improve the surgeon’s mechanical advantage for any MIS case, in any size patient. Mechanical advantage (eg, improved torque, increased degrees of freedom) may seem nebulous, but it is always recognized by a peculiar sense of physical relief. The surgeon with mechanical advantage exerts less effort, makes fewer moves, feels less fatigue, and places the needle or hook exactly. Moreover, a good heuristic always contains a real verb, an observable action taking an actual object (institutional verbs do not; eg, optimize, foster, strive, endeavor, assess). Principles should apply in the real world.
Technology is not technique
Tools do not perform the operation. For example, the surgical robot is really a telemanipulator or waldo. Tools cannot make a novice surgeon into an expert, even if hospitals cannot resist using these devices in their advertisements. Devices should be understood as a tool for something. The surgical telemanipulator is a tool for increasing surgical degrees of freedom and for offering better movement than rigid instruments. A stapler is a tool for tissue approximation. However, endoscopic gadgets are rarely designed for very small patients, and trying to force these devices invites error (eg, trying to squeeze a standard endoscopic stapler into an infant’s chest). Features easily become bugs when the tools are misunderstood.
On the other hand, the expert surgeon has developed robust and general skills with basic endoscopic instruments. His or her suture technique is as precise as the open technique. He or she can safely and rapidly perform many procedures at least as well as (and, in many cases, better than) using open technique. Use of gadgets fosters shortcuts and poor methods, compromises outcomes, and lends MIS an air of risk. In cases of trouble, the patient is always better served by reliable technique than by technology.
An important corollary here is that the expert knows how all the tools work. She or he knows how the tools are assembled, how feedback is measured, how the various energy sources work, and what the limits and liabilities are. For example, the novice is baffled by insufflation problems. An expert quickly recognizes a problem and tracks possible causes from the wall to the patient, from the CO2 source, to the insufflator, to the tubing, to the trocars, to the instruments, to the depth of anesthesia. Similarly, the expert chooses hook, spatula, hot scissors, Harmonic Scalpel (Ethicon, Endosurgery, Cincinnati, OH, USA), or Ligasure (ValleyLab, Boulder, CO, USA) according to a desired tissue effect, how the shape of the business end fits his or her surgical field, and what problems are minimized by choosing one over the other. The novice has a single tool and tries to use it everywhere (eg, trying to use the Harmonic scalpel as a magic coagulator on a liver capsule bleed).
MIS is not technology, but it depends on it. The right tools — camera, ports, instruments, scopes — make the difference between a safe operation performed smoothly under conditions of excellent visualization…and a “flail.” The expert surgeon protects patients from the hidden cost-increases that accompany pennywise administrative choices by insisting on tools that offer objective advantages.
Although an experienced surgeon will be irritated by clunky instruments, the novice will be flummoxed, operating with jerky moves and halting over-corrections. The delicate infant liver, fine sutures, and ephemeral tissue planes become casualties of the novice surgeon’s distress. Then, disrupted anatomy and bloody views make the operation even harder, producing a feed-forward spiral to suboptimal results at best and disaster at worst. Well-chosen, well-functioning tools must be regarded (and budgeted for) as indispensable contributors to patient safety. A novice blames the tools; the expert’s tools serve her or his technique.
A hidden hazard with surgical devices lies in implied uses, sometimes called affordances. Rarely are surgeons given instruction on the elements of devices’ designs, and user manuals are an early casualty of a busy operating room. Instead, surgeons in training typically receive casual lessons or lore, often passed from a senior resident, lessons they may pass to their own trainees. Sometimes, those lessons are correct; however, they are often only someone’s workaround (eg, a Malecot drain repurposed as a gastrostomy tube). Other times, the use is simply a misunderstanding of a design that implies by its shape or structure that it should be used a particular way.
Sometimes, these hints for use are accurate but, without a real why behind some practice, the novice will have no basis with which to tell. For example, novice operators think they must always insert finger and thumb into laparoscopic instruments, often forcing the hand into awkward supination. The way around this is to palm the instrument, using a light grip.
The surgeon must understand when the design does not quite serve, how these shortcomings can increase risks, and how to mitigate them. For example, some surgical staplers require a relatively strong grip to fire. A surgeon with smaller hands may be at a serious mechanical disadvantage, shaking struggles during firing may translate to risky jarring at the business end. One way around this is to turn the handle upside down, lengthening the effective moment arm (torque = force × moment arm length), decreasing the force required to exert the same torque on the firing mechanism.
Of course, another way around this problem is to use another method. The expert has no problem switching from a stapler to a suture, endoloop, or clip. She or he has mastered multiple methods and so has greater versatility. Expert MIS technique is enabled by technology but not limited to the technology.
Set up for mechanical advantage
Face the Organ!
Mechanical advantage requires good patient positioning. However, positioning the patient properly actually begins with positioning the surgeon. Too often, surgeons operate awkwardly, stricken by the paradoxic action of their tools on the screen. Precision movement is laughable when the surgeon cannot intuit right and left, up and down. Of course, it is not funny for the surgeon.
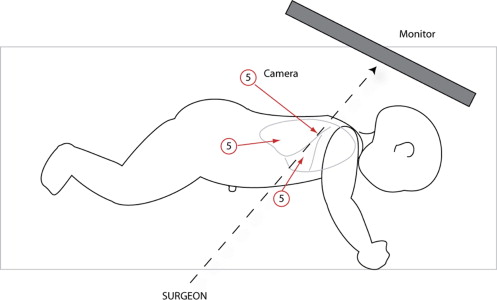
Perfect position allows the surgeon to operate with small effort. The most important principle for good position that the surgeon should face the organ he or she is operating on. In other words, the surgeon should place the monitor in a line with herself or himself, the camera, and the organ of interest. An old mnemonic is S-C-O-P: surgeon→camera→organ→picture. For example, with appendectomy, the surgeon stands to the patient’s left, facing the right lower quadrant with the screen on the patient’s right. Alternatively, when operating on the gastroesophageal junction, the surgeon should stand at the foot of the bed (with babies frog-legged at the end of the bed, larger patients in low lithotomy position) facing the epigastrium, with the monitor hung directly over the patient’s chest ( Fig. 1 ).

Meanwhile, poor position exhausts the surgeon. As the surgeon fatigues, the muscles responsible for fine movements fail first, degrading precision. For example, a surgeon who attempts to operate on a spleen from the patient’s left not only struggles with a poor angle of attack and paradoxic motion, but the awkward body position quickly leads to fatigue. If the surgeon is shaking and sore after the procedure, the set-up was probably suboptimal.
Implicit in this rule is knowing what the organ is. For example, when performing a thoracoscopic lobectomy, the organ is not the lung or the lobe; it is the major fissure, the place where most of the fine dissection occurs ( Fig. 2 ), and the surgeon should stand in line with it. Similarly, when performing laparoscopic procedures on the infant bladder or rectum the surgeon should stand at the baby’s head.
One mental barrier to facing the organ is the implicit rule that a surgeon and an assistant must operate opposite each other (with even left and right sides implying surgical hierarchy). Any other arrangement seems wrong, even taboo. However, what brings advantage in open cases may bring disadvantage in MIS cases. It is absurd for either surgeon or assistant to struggle with paradoxic motion. This unwise practice is tolerated because of the belief that an operator must stand on each side of the patient regardless of the surgical objective. Facing the organ goes for surgeon and assistant, even if both stand on the same side of a patient (as they often should).
Imitate the Pianist
Only when facing the organ can the other aspect of good positioning be used: the pianist position. Virtuoso pianists hold their arms loose at the shoulder, arms bent at the elbow, wrists loose, and fingers on the keys. Virtuoso endoscopic surgeons operate with the bed at a level that allows them the same position: head upright and level with the screen, shoulders relaxed, elbows bent at 90° to 120°, wrists loose, and action on the instruments controlled with light pressure in the fingertips. The novice can be seen with back bent, arms abducted, elbows askew, wrists stiff, and instruments held in a death grip. Expert surgeons’ moves look fluid and relaxed compared with the novice’s, in large part because the expert’s positioning is better. The comfortable surgeon attends to surgical detail; the uncomfortable surgeon thinks about his or her sore back.
Maximize Degrees of Freedom
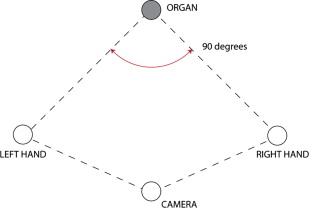
Positioning the patient and the surgeon are part of a good set up. Port placement is another. In general, the camera is in the center (however, not always; see later discussion) and trocars should be placed so that right-hand and left-hand instruments approach the organ of interest separated by approximately 90°. Meanwhile, the camera port should be offset from the 2 main working ports such that the 3 ports form a triangle, not a line. These 4 points, the 3 main ports and the organ, form a kite-like shape, a configuration that generally allows the best view, comfort, and maneuverability ( Fig. 3 ).