Sequence type
Orientation
Number of slices
Slice thickness (mm)
Slice gap (mm)
Field of view (mm)
TR (ms)
TE (ms)
Fat saturation
Matrix
Flip angle (°)
Single-shot TSE-T2 (HASTE, SSFSE, SSTSE)
Coronal
26
5
0
380 × 308
1,550
91
No
512 × 307
150
Axial
50
5
0
380 × 308
1,550
69
No
512 × 307
150
Balanced GRE (TrueFISP, FIESTA, Balanced FFE)
Coronal
28
3 and 5
0.3–0
400 × 400
4.52–4.6
2.26–2.3
No
320 × 240–320 × 250
80
Axial
50
5
0
400 × 275
4.6
2.3
No
320 × 250
80
Cine scans
Coronal
1
10
380 × 380
4.16
2.08
No
256 × 205
70
T1-3D GRE (VIBE, LAVA, THRIVE)
Coronal
48
3
0
400 × 400
3.98
1.85
Yes
384 × 269
10
T1-3D GRE (VIBE, LAVA, THRIVE)
Axial
64
3.5
0
400 × 300
3.66
1.65
Yes
256 × 166
10
DWI
Axial
31
5
0
380 × 380
6,600
69
Yes
192 × 154
90
MR Characteristic Small Bowel Findings in Crohn’s Disease
Bowel Wall Abnormalities
Wall Thickening
Thickening of the bowel wall (Fig. 5.1) occurs due to edema and infiltration with inflammatory cells in active inflammation or due to deposition of collagen in fibrostenosing disease, and is one of the most important imaging abnormalities in CD [3, 9, 18, 26]. Normal bowel wall thickness (in optimal distended bowel) ranges from 1 to 3 mm and in case of CD inflammation has values ranging from 5 to 10 mm. The bowel wall thickening may be asymmetric due to the preferential inflammatory involvement of the mesenteric side of the bowel wall. The post-contrast T1-images and the HASTE sequences allow better assessment of bowel wall thickness compared to the true FISP images. The black boundary artefact seen on the true FISP images can confound evaluation of wall thickness whereas the HASTE sequences are relatively insensitive to this artifact.
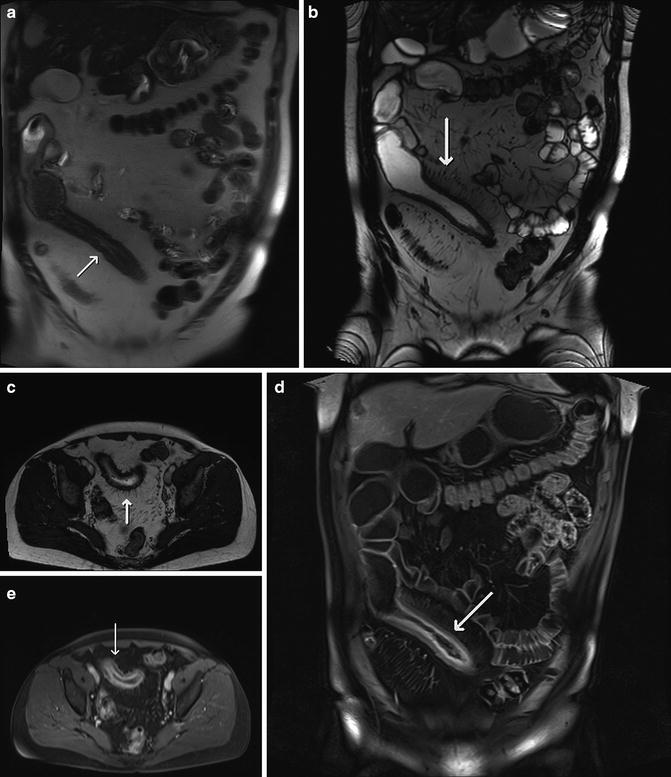
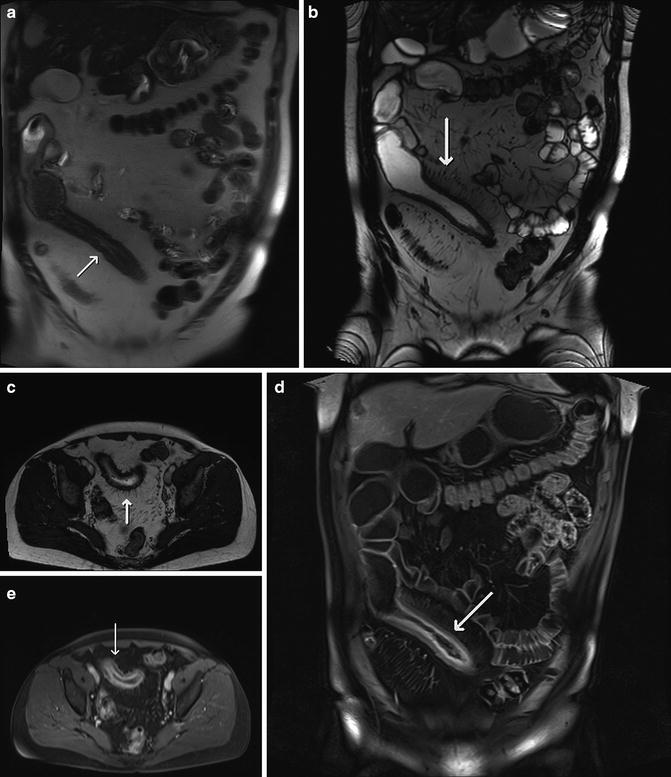
Fig. 5.1
(a) Acute-on-chronic CD in the distal ileum in a 58-year-old patient with circumferential wall thickening (arrow) on the coronal HASTE image. (b) Coronal and (c) axial true FISP images show dilated peri-ileal blood vessels or comb sign (arrows). The presence of layered enhancement pattern of the bowel wall (arrows) on (d) the coronal and (e) axial fat-suppressed 3D T1 GRE images
Bowel Wall Edema
Increased signal intensity [3, 9, 18] of the thickened bowel wall on the HASTE sequences can suggest bowel wall edema and indicate active inflammation, whereas low to moderate T2 signal intensity may suggest underlying fibrosis. However, the absence of high signal intensity in the thickened wall does not exclude active disease. High T2 bowel wall signal intensity can also be present in case of intramural fat deposition, found in chronic inflammation, and can be differentiated from edema by using fat-saturated T2 sequences (Fig. 5.2).
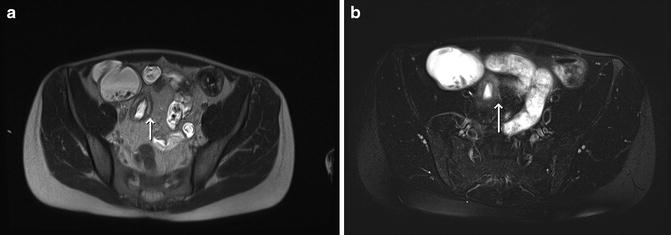
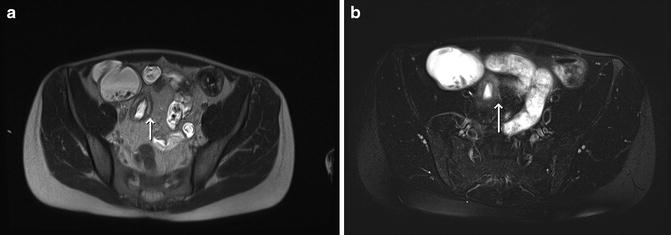
Fig. 5.2
A 31-year-old patient with acute-on-chronic CD in the distal ileum. (a) Axial HASTE and (b) axial T2-weighted fat-suppressed TSE images show bowel wall thickening with high T2 signal consistent with edema (arrows) and acute inflammation
Fold Abnormalities
Good bowel distension and absence of flow artefacts are crucial to assess fold abnormalities, to avoid false-positive and false-negative results. In case of suspected fold abnormalities and insufficient bowel distension more MR sequences can be acquired after additional ingestion of oral contrast material. True FISP images are superior for evaluating some fold abnormalities given the minor flow artifacts. The latter are also reduced by anti-spasmodic agents, given that they reduce fluid flow in the bowel lumen.
Alterations in fold patterns are more evident along the mesenteric border, characteristic of the disease and can manifest in different ways. The three main patterns of fold abnormalities are diffuse fold thickening, ulceration of folds, or in more severe disease cobblestoning [11, 20].
Early areas of mucosal ulceration (Fig. 5.3) present as small foci of hyper-intensity surrounded by a rim of edema, deeper ulcerations present as lines of high signal intensity in the thickened bowel wall on the T2 images, paralleling the lumen or protruding transversely into the wall. Cobblestone appearance is the result of a combination of longitudinal and circumferential ulcers and fissures separating islands of mucosa.
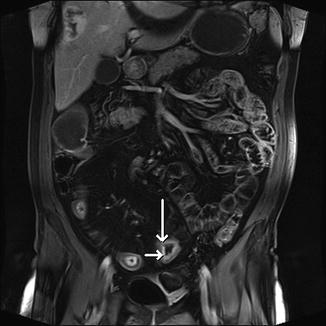
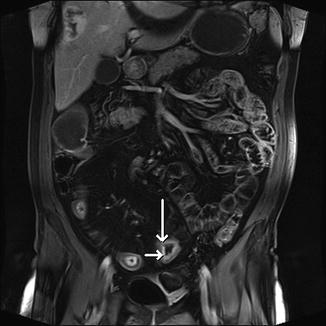
Fig. 5.3
Acute inflammation of the distal ileum with mucosal ulcerations (arrows) on the coronal fat-suppressed 3D T1 GRE image in a 58-year-old patient with CD
Better assessment of mucosal ulcerations can be obtained by using high resolution MR imaging compared to standard MRE [27], although it remains inferior compared to endoscopy.
Strictures
These are segments of persistent narrowing of the bowel lumen (Figs. 5.4 and 5.5) with or without bowel wall thickening. They are considered to be functionally significant if there is an upstream bowel dilatation of more than 3 cm and defined as nonfunctional if the bowel lumen is narrowed more than 10 % compared to neighboring bowel loops in the absence of bowel dilatation [20]. Differentiating active from chronic strictures has important therapeutic implications and remains a diagnostic challenge on MRE.
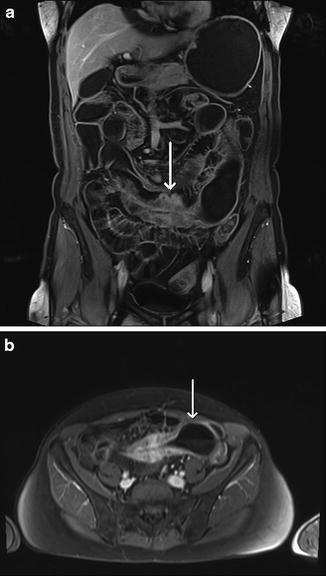
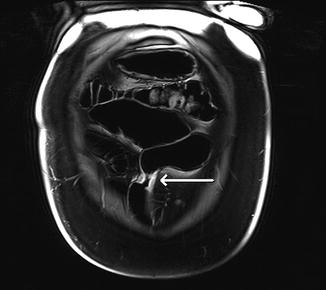
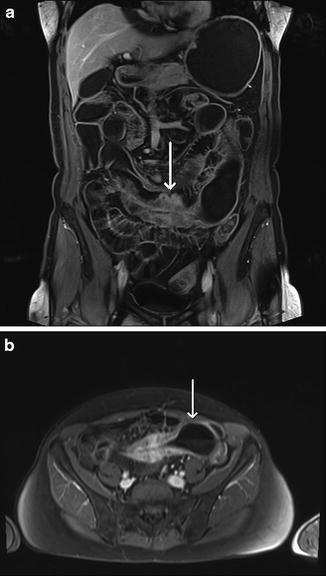
Fig. 5.4
A 58-year-old patient with long-standing CD and right colectomy. (a) Coronal and (b) axial fat-suppressed 3D T1 GRE images show severe wall thickening and stenosis (arrow image a) with secondary obstruction (arrow image b)
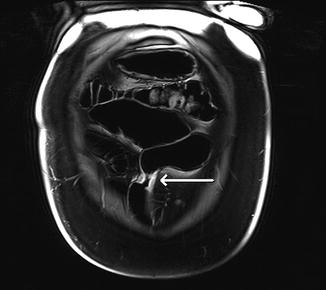
Fig. 5.5
The presence of a short inflammatory segment or skip area (arrow) on the ileum with secondary obstruction on a coronal fat-suppressed 3D T1 GRE image
Non-fibrotic strictures tend to have wall thickening with high signal intensity on the T2 sequences, suggesting the presence of bowel wall edema, whereas fibrotic strictures have lower signal intensity in the bowel wall on T1- and T2-weighted images.
Bowel Wall Enhancement
Bowel wall enhancement is increased compared to the surrounding normal bowel loops and correlates with bowel inflammation and disease activity [11, 20]. The evaluation of the different patterns of bowel wall enhancement can be useful in determining the level of disease activity.
Three-layered pattern of contrast enhancement (Fig. 5.6), also called mural stratification, consists of strong enhancement of the mucosa, relatively poor enhancing submucosa, and strong enhancement of the serosa; this type of enhancement, in combination with bowel wall edema, is found in active inflammation. Strong mucosal enhancement is one of the most sensitive indicators of active CD.
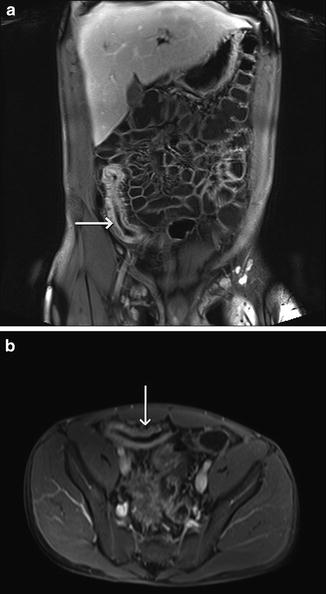
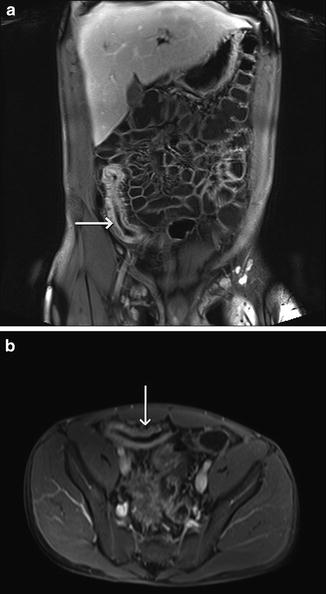
Fig. 5.6
(a) Coronal and (b) axial fat-suppressed 3D T1 GRE images in a 20-year-old male with wall thickening and strong mucosal enhancement (arrows) of the distal ileum, indicating acute CD
Diffuse and intense homogenous contrast enhancement suggests transmural inflammation, but remains nonspecific given the fact that it can be found in active and chronic disease.
Minimal and heterogeneous bowel wall enhancement is rather seen in segments where fibrosis predominates.
Pseudodiverticulum and Pseudosacculation
Pseudodiverticulum and pseudosacculation are the result of the asymmetric and preferential inflammation of the mesenteric side of the bowel wall and relative sparing of the opposite bowel wall. Fibrosis in the diseased mesenteric wall results in shorting of this side of the bowel wall and dilatation of the opposite wall, leading apparent sacculation or formation of a diverticulum [18]. In contrast to diverticular disease in the colon, CD involves all layers of the bowel wall, and focal dilations are called pseudodiverticula or pseudosacculations (Fig. 5.7). As this is seen in the chronic setting of CD, other concomitant signs of chronicity are usually present.
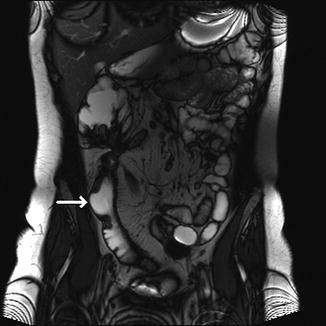
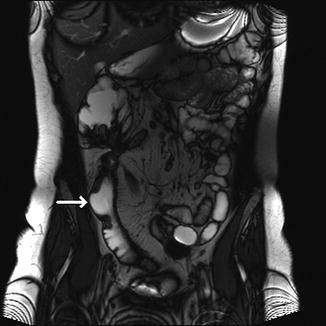
Fig. 5.7
A 34-year-old patient with CD. Pseudosacculation (arrow) of the antimesenteric wall within the inflamed distal ileum on the coronal true FISP image
Extraintestinal Findings
Engorgement of the Vasa Recta
Engorgement of the vasa recta is the result of increased blood flow through the vasa recta to the inflamed bowel segments. If these vessels have a perpendicular course to the long axis of the diseased segments it is called the comb sign (Fig. 5.8). Fine lines of low signal intensity on the true FISP images and high signal lines on the post-contrast T1 images are seen.
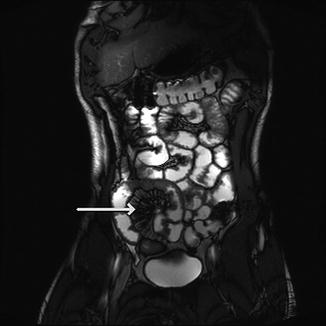
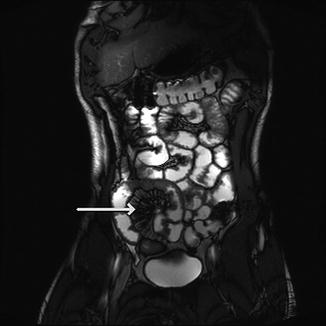
Fig. 5.8
Coronal true FISP image of a 20-year-old patient with CD, showing moderate to severe comb sign (arrow)
Fat Stranding
Inflammation of the mesenteric fat or mesenteric edema surrounding the inflamed bowel segments, together with the comb sign, bowel wall edema and strong enhancement of the bowel wall, strongly suggest active disease [3].
Fibrofatty Proliferation
Fibrofatty proliferation is usually seen in patients having a history of longstanding CD and can be a useful diagnostic discriminator as it is rarely seen with other differential diagnosis.
Hypertrophy of fat surrounding diseased bowel loops, can be symmetric or asymmetric [18], in the latter preferentially involving the mesenteric border of the bowel, and can produce mass effect on the surrounding bowel loops or organs.
Lymph Nodes
Enlarged mesenteric lymph nodes (Fig. 5.9) are often seen in patients with active and inactive CD and they are frequently, but not always located in the area of the diseased bowel loops, often around the ileocolic vessels, given the preferred side of the disease. A study [28] showed that the mesenteric lymph nodes in CD present with a different degree of homogenous contrast enhancement, depending on the disease subtypes and therefore quantification of enhancement ratios could be useful for disease subtype classification.
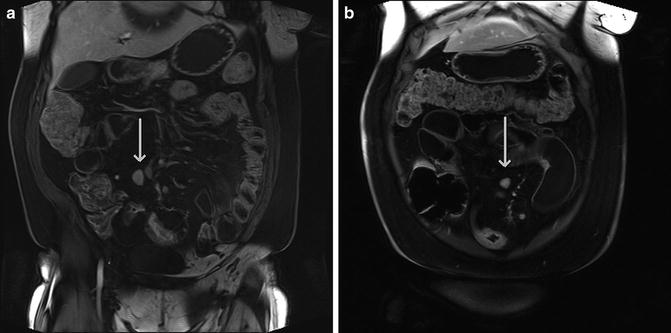
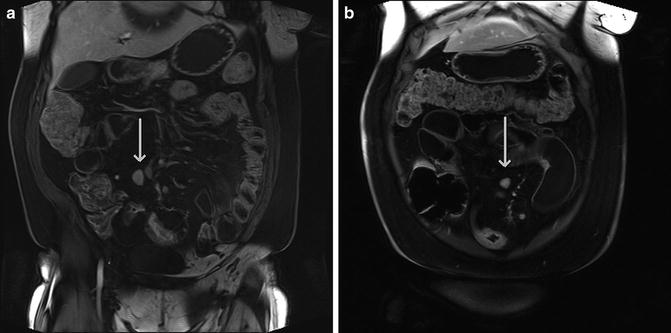
Fig. 5.9
A 52-year-old patient with CD. (a, b) Coronal fat-suppressed 3D T1 GRE images showing mesenteric lymph nodes (arrows) adjacent to the inflamed bowel segments
If multiple enlarged mesenteric lymph nodes are present, lymphoproliferative disease should be excluded, given the additional risk as a consequence of CD treatment.
Fistulas and Sinuses
When a transmural ulcer communicates with an adjacent epithelial surface, it becomes a fistula [9, 18]. Most fistulas (Figs. 5.10 and 5.11) arise between small bowel loops (entero-enteric fistula) or between a small bowel loop and a colon segment (entero-colic fistula), but can also communicate with other organs, such as bladder, skin or even local muscles. The fistulas are usually seen as high signal tracts on the T2 images, with variable degrees of enhancement after administration of intravenous contrast material. These fistula tracts may vary from single to complex, sometimes having stellate appearance with multiple tracts radiating from a central point to adjacent bowel, other organs or even local muscles, such as the psoas muscle. Fistulas can easily be depicted on MR, with the exception of enterocutaneous fistulas. The latter are harder to visualize because of their superficial location and the compression in the often prone positioning of the patient makes it more difficult to assess these enterocutaneous tracts. If there is clinical suspicion of cutaneous fistula, supine positioning of the patient is preferred and additional sequences in the sagittal plane can be taken to better assess the location and extent of the fistula. In some cases MR images provide insufficient assessment and additional conventional radiology techniques are necessary, such as fistulography.
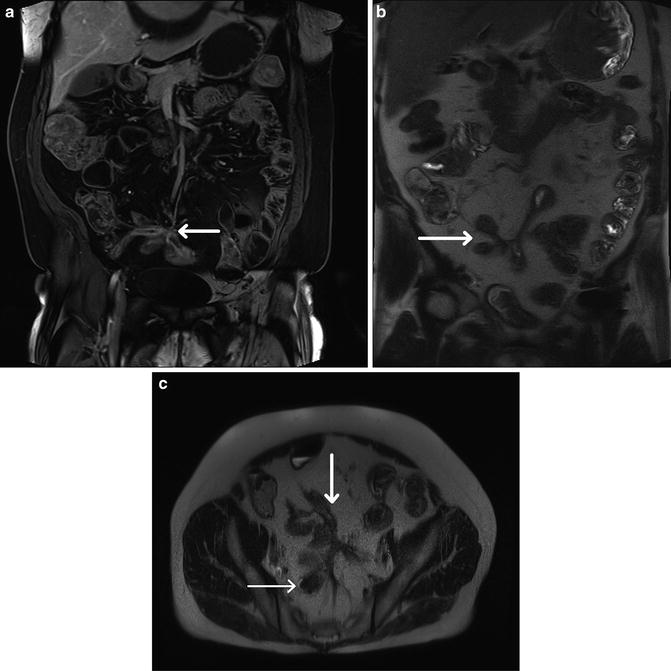
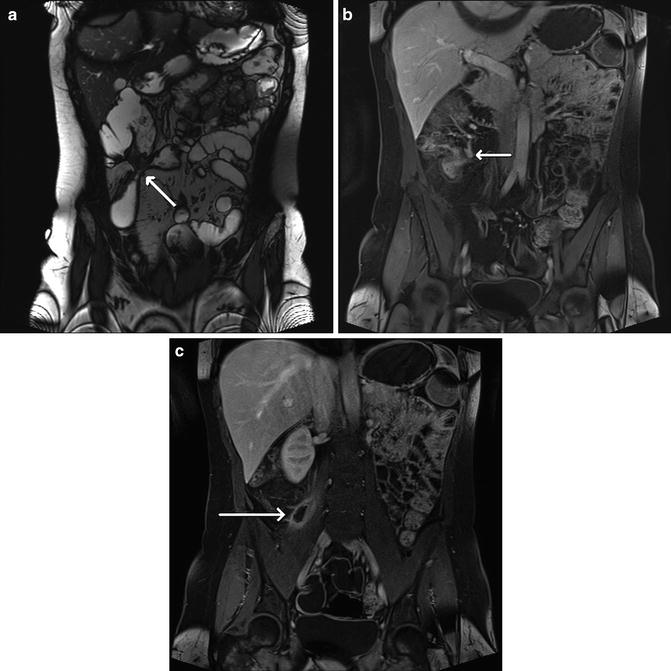
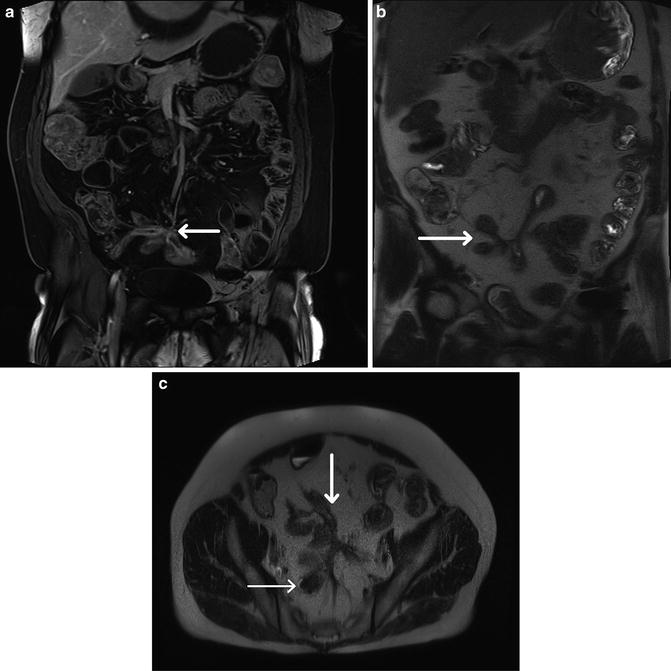
Fig. 5.10
A 52-year-old patient with penetrating CD. (a) Coronal fat-suppressed 3D T1 GRE, (b) coronal HASTE, and (c) axial HASTE show bowel wall thickening of the distal ileum with associated luminal narrowing (arrow image a). Fistula involving distal ileum segments (thick arrow image c) and the sigmoid (thin and thick arrow image c), with secondary tethering of the surrounding bowel loops (b and c)
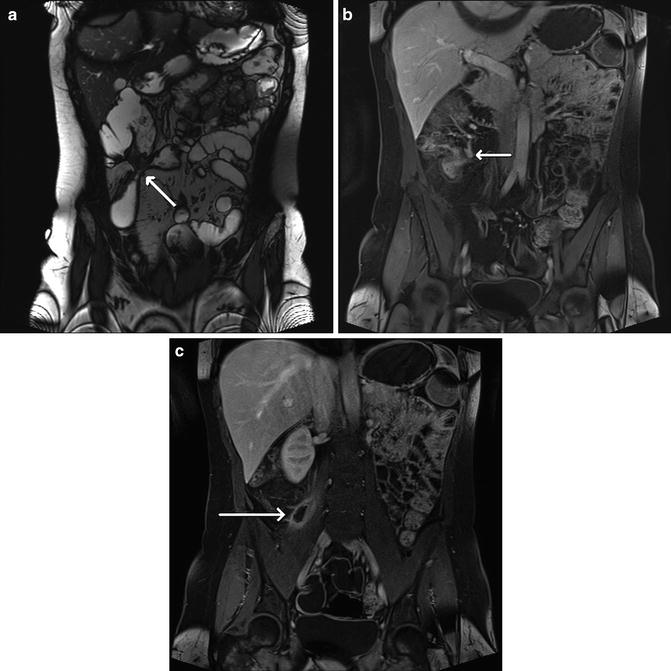
Fig. 5.11
Fistula and abscess in a 34-year-old patient with CD. (a) Coronal true FISP and (b) coronal fat-suppressed 3D T1 GRE images show the presence of fistula (arrows) involving the distal ileum, caecum, ascending and transverse colon, with tethering of the surrounding bowel loops. (c) The presence of an abscess (arrow) in the right psoas muscle on the coronal fat-suppressed 3D T1 GRE image
If a transmural ulceration does not communicate with another epithelial surface, it is a blind-ending tract and called a sinus. These sinuses have the same MR characteristics as fistulas.
Abscess
An abscess (Fig. 5.11) is an encapsulated fluid collection with peripheral contrast enhancement [18]. They can contain air and their content is often heterogeneous due to the presence of solid material and gas. Abcesses are easily depicted on MR, having high signal on T2 and low signal on T1. On the other hand, small amounts of air in a collection might be difficult to visualize. The detection of an abscess is important, because it is a relative contra-indication to the use of anti-TNF-alpha drugs. In some cases these abscesses can first be treated with imaging-guided drainage before starting medical therapy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








