■ T1 stage is associated with 88% sensitivity and 98% specificity.
■ T2 stage is associated with 81% sensitivity and 96% specificity.
■ T3 stage is associated with 96% sensitivity and 91% specificity.
■ T4 stage is associated with 95% sensitivity and 98% specificity.5
■ Detection of lymph node metastasis is associated with 73% sensitivity and 76% specificity.6
■ High-resolution pelvic magnetic resonance imaging (MRI) delineates the layers of the bowel wall in T2 weighted images. It is associated with 93% to 97% sensitivity for T staging and 77% sensitivity for lymph node metastasis.7,8
■ Computed tomography (CT) scan of chest, abdomen, and pelvis should be obtained for preoperative evaluation metastases as per National Comprehensive Cancer Network (NCCN) guidelines.9 It is associated with 40% to 86% accuracy in staging rectal cancers.8,10,11
SURGICAL MANAGEMENT
Preoperative Planning
■ Surgical decision is based on rectal cancer staging. As per NCCN guidelines, neoadjuvant chemotherapy and radiation therapy (CRT) should be considered for all N+ positive tumors based on preoperative imaging. The use of neoadjuvant CRT in T3N0 tumors is somewhat controversial. Proximal T3 tumors with no involvement of the circumferential resection margin (i.e., posterior lesions surrounded by abundant mesorectum) can selectively undergo radical resection without CRT.9
■ Neoadjuvant CRT has been shown to reduce the local recurrence rate and increase the chances of sphincter-sparing surgery.9
■ The decision for neoadjuvant chemotherapy should stem from a multidisciplinary discussion amongst the surgeon, oncologist, radiation oncologist, and patient.
■ An enterostomal therapist should be involved for counseling and for potential stomal marking prior to operation.
■ Despite the debate regarding bowel preparation, we routinely use mechanical bowel preparation at our institution for easier manipulation of the bowel during surgery. Our institution’s standard bowel preparation is 510 mg of MiraLAX® in 128 oz of Gatorade®.
■ Rectal irrigation via saline solution is performed in all patients.
■ A Foley catheter is placed in all patients after induction for bladder decompression.
■ Prophylactic ertapenem (Invanz®) antibiotic is administered prior to induction of anesthesia.
■ Sequential compression devices are placed in all patients. However, the use of pharmacologic deep vein thrombosis (DVT) prophylaxis is not routinely used. The benefit of chemical prophylaxis remains controversial.12,13
Positioning
■ The patient is placed in a modified lithotomy position with attention placed to correct technique to minimize injury:
■ The patient is ideally placed on a large high-density viscoelastic foam mat to prevent sliding.
■ The patient is brought to the edge of the table and the legs are placed into Yellofin® or Allen® stirrups with the hips slightly flexed and abducted, the feet flat within the stirrups, and pressure avoided along the lateral aspects of the legs. The ankle, knee, and contralateral shoulder should be aligned.
■ A Velcro belt is strapped over the chest to prevent side-to-side sliding.
■ The perineum is prepped if a transanal extraction and or hand-sewn anastomosis is anticipated.
TECHNIQUES
LAPAROSCOPIC MEDIAL TO LATERAL DISSECTION OF COLON
Port Placement
■ Pneumoperitoneum is established via a Veress needle at Palmer’s point (1 to 2 cm below the left costal border in the midclavicular line [MCL]).
■ The ports are triangulated and placed at a minimum of one handbreadth apart (FIG 2).
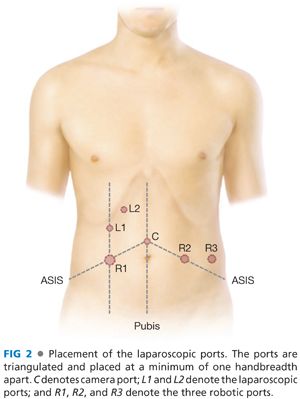
■ The camera (C) port is placed halfway between the xiphoid process and symphysis pubis.
■ Three robotic (R) ports will be placed as follows (FIG 2):
■ R1 is a 12-mm trocar inserted in the MCL halfway in between C and the right anterior superior iliac spine (ASIS). This port can be used for ileostomy placement at the end of the surgery.
■ R2 is an 8-mm trocar inserted as a mirror image of R1.
■ R3 is an 8-mm trocar inserted 8 to 10 cm lateral to R2, usually directly above the left ASIS.
■ Laparoscopic-assisted (L) ports (FIG 2):
■ L1 is a 5-mm trocar inserted in the MCL about 12 cm superior to R1.
■ L2 is a 5-mm port inserted halfway between MCL and midline about 12 cm superior to L1.
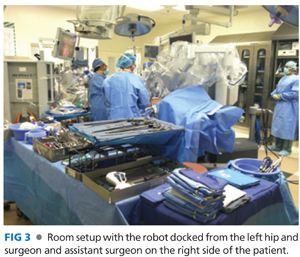
■ Both surgeon and assistant stand on the right side of patient (FIG 3).
■ R1, L1, L2, and C ports are used during the laparoscopic section.
Laparoscopic Transection of the Inferior Mesenteric Vein
■ The peritoneal cavity is explored for evidence of metastatic disease.
■ The patient is placed in a Trendelenburg position with the left side elevated.
■ The small bowel is swept out of the pelvis. Nontraumatic bowel graspers are used to avoid injury.
■ The dissection is begun at the inferior mesenteric vein (IMV), lateral to the ligament of Treitz (FIG 4).

■ The IMV is identified and dissected from its attachments to the left mesocolon.
■ The peritoneum is scored with monopolar electrocautery.
■ Blunt dissection is used to skeletonize the vessel. Once this is achieved, the vessel is clipped and divided via vessel sealer device just below the pancreas. This can also be accomplished with an Endo GIA vascular stapler.
■ Transection of the IMV will serve as a lengthening maneuver, which in turn will decrease tension on the anastomosis.
Laparoscopic Transection of the Inferior Mesenteric Artery
■ The sigmoid mesocolon is retracted toward the anterior abdominal wall, and the parietal peritoneum medial to the right common iliac artery at the sacral promontory is incised.
■ Upward traction is maintained by the assistant and blunt dissection is used to enter the avascular retroperitoneal plane. This plane is developed under the superior hemorrhoidal artery (FIG 5).

■ The left ureter and the hypogastric nerve are identified and swept posteriorly (FIG 5).
■ This dissection is continued to the origin of the inferior mesenteric artery (IMA) at the aorta.
■ The IMA is skeletonized using monopolar cautery. The junction of left colic artery and superior hemorrhoidal at the IMA can be visualized in a letter “T” configuration (FIG 6A).

■ The IMA is clipped and divided at its origin from the aorta with a vessel sealer device (FIG 6B). This can also be accomplished via Endo GIA vascular stapler.
■ The left colic artery is divided at its origin from the IMA (FIG 6B).
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








