■ During the perineal part of the procedure, the entire team shifts toward the extremity of the table once the perineum has been exposed.
■ The monitors are placed in front of the operating team and at eye level to improve ergonomics.
Port placement
■ One 12-mm supraumbilical port (port A) is introduced first using a mini-open technique. It will be used to accommodate the camera (FIG 2).

■ Two other ports, a 5-mm port in the right flank (port B) and a 12-mm port in the right iliac fossa (port C), are used as operating ports (FIG 2).
■ The fourth port in the left flank at the level of the umbilicus is inserted through the rectus muscle (port D, 5 mm in diameter), where the colostomy will be performed (FIG 2).
■ The last port introduced in the suprapubic area (port E, 12 mm in diameter) is used for pelvic retraction and for exposure of the sigmoid colon’s root (FIG 2).
■ Port fixation in the wall should be perfect in order to prevent any risk of parietal injury and to prevent increased operative times due to a loss in abdominal pressure. One should not hesitate to fix ports to the skin.
■ Additional ports may be used in case of difficulty in exposure. In this case, a port will be positioned in the right hypochondrium (port F) to retract the ileocecal area. This is particularly useful in obese patients (FIG 2).
TECHNIQUES
LAPAROSCOPIC LOW ANTERIOR RESECTION
Exploration and Exposure
■ The intervention is begun by an exploration of the abdominal cavity to locate the tumor and evaluate for possible metastases. It also allows to expose the pelvis and to evaluate the length and quality of the sigmoid loop, which will allow determining the type of mobilization of the left colon and of the splenic flexure.
■ The tumor’s identification may be necessary and especially so for tumors located proximally. Combined endoscopy may be required in cases where an effective preoperative marking could not be performed on the day before the intervention.
■ Exposure is improved by placing the patient in a Trendelenburg position with the table tilted to the right.
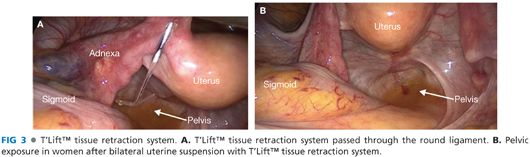
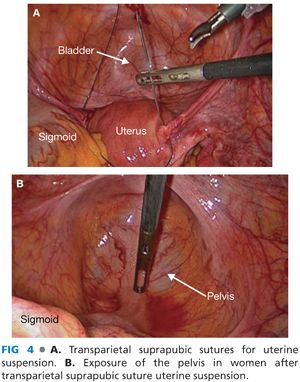
■ In women, exposure of the posterior pelvis and of the rectovaginal (Douglas’) pouch can be obtained by direct or indirect suspension of the uterus by means of the T’Lift™ (VECTEC, France) tissue retraction device (FIG 3A,B) or suprapubic transparietal sutures (FIG 4A,B).
■ Visceral obesity (in male patients) is more incapacitating than subcutaneous obesity (in female patients). The use of retractors is very helpful.
Primary Vascular Oncologic Approach to the Sigmoid Colon
■ As for any oncologic surgical procedure, a primary vascular approach is the rule.
■ In rectosigmoid cancer, one should approach the inferior mesenteric vessels at their origin in order to perform an “en bloc” removal of all lymph nodes associated with the rectosigmoid junction (D3 resection). It does not preclude the potential preservation of the proximal inferior mesenteric artery (IMA) and of the left colic artery (LCA).
■ We always start with a primary approach to the IMA. The inferior mesenteric vein (IMV) is then approached in order to prevent any venous overload related to the late ligation of the IMA.
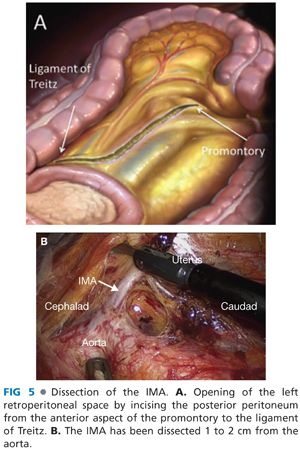
■ Once the root of the sigmoid mesocolon has been exposed, the left retroperitoneal space is opened by incising the posterior peritoneum from the anterior aspect of the promontory up to the left border of the duodenojejunal junction (ligament of Treitz) (FIG 5A).
■ Once the retroperitoneum has been opened, dissection is initiated opposite the promontory on the posterior aspect of the inferior mesenteric vascular sheath (i.e., the superior rectal artery at this level). This step is facilitated by the anterior traction on the mesocolon, which induces the pneumodissection of the retrovascular space, thanks to intraabdominal carbon dioxide pressure.
■ Dissection is carried on in contact with the vascular sheath cranially until the origin of the IMA on the aorta.
■ The dissection is continued from caudad to cephalad in contact with the artery, which is skeletonized over approximately 2 cm in order to achieve ligation and division 1 or 2 cm away from the aorta (FIG 5B).
■ This technique allows preserving sympathetic nerve plexuses, which course along the aorta on its right anterior aspect.
■ Division of the IMA is performed with the LigaSure™ vessel-sealing device using a ligation with a loop on the IMA stump.
■ Once the IMA has been divided, the assistant standing between the patient’s legs will grasp the artery using an atraumatic forceps introduced into the suprapubic port (port D) and apply anterior traction to ideally expose dissection planes in contact with the left posterior and lateral aspects of the artery.
■ It helps to preserve the nerve plexus in contact with the artery, and notably the left sympathetic trunk of the neurovegetative system that will be progressively freed and parietalized.
■ The next operative step will be to identify the IMV lateral to Treitz’s flexure underneath the inferior edge of the pancreas.
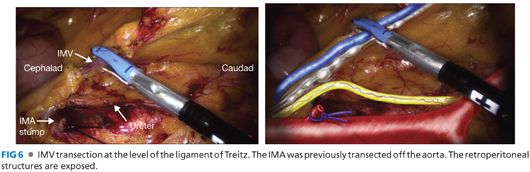
■ The IMV is then transected at the level of the ligament of Treitz with the LigaSure™ vessel-sealing device or in between clips (FIG 6).
Mobilization of the Left and Sigmoid Colon
■ Many authors prefer to start with the mobilization of the splenic flexure using a medial posterior transverse transmesocolic approach. We prefer to mobilize the splenic flexure at the end of the operation in order to prevent excessive mobilization, which can be a cause of morbidity.
■ Our main objective is to perform a medial to lateral mobilization of the mesocolon.
■ A medial to lateral mobilization of the sigmoid colon allows for traction on the upper rectum with a perfect exposure of its anterior, posterior, and lateral aspects.
■ Mobilization of the mesocolon is performed using a medial to lateral approach (FIG 7A,B) by opening the plane between Toldt’s fascia anteriorly and Gerota’s fascia posteriorly.
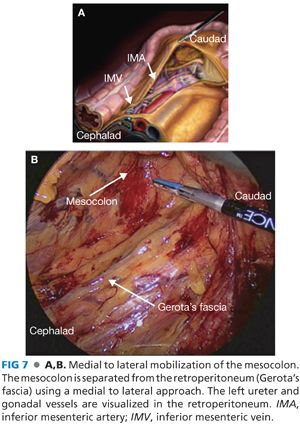
■ The dissection is carried laterally until the posterior aspect of the descending colon is reached laterally.
■ Caudally, the dissection is carried toward the pelvic inlet. One should be cautious when in contact with the aorta as well as with the left iliac vessels where nerve rami of the superior hypogastric sympathetic plexus courses.
■ The left ureter is identified during the dissection. It is located between the aorta and the genital vessels, well protected by Gerota’s fascia.
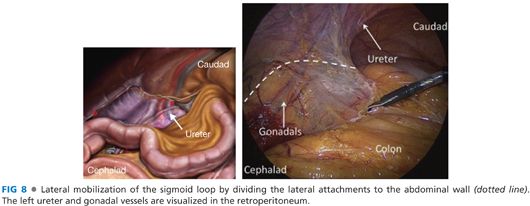
■ Mobilization of the sigmoid colon is completed with a division of its lateral attachments to the abdominal wall (FIG 8).
Dissection of the Rectum According to the Total Mesorectal Excision (Heald’s) Technique
■ The principle of TME relies on the study of the embryologic development of the pelvis and of organs located within it. A surgical intervention cannot be envisaged without a detailed knowledge of pelvic and fascial anatomy (FIG 9A) that is essential to obtaining appropriate surgical specimens.

■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








