Type
Image features and remarks
CL
Status: active
Image features: unilocular; not clearly delimited by a hyperechoic rim; cyst wall not visible
Remarks: generally early-stage and non-proliferative cyst
CE1
Status: active
Image features: visible cyst wall; hydatid sand (snow flake sign)
Remarks: generally active proliferative cyst
CE2
Status: active
Image features: multivesicular cyst; “wheel-like,” “rosette-like,” or “honeycomb-like” structure
Remarks: generally active proliferative cyst
CE3
Status: transitional
Image features: detachment of laminated membrane; double wall sign; water-lily sign or wavy membrane
Remarks: start to degenerate and produce daughter cysts
CE4
Status: inactive
Image features: Heterogeneous hypoechoic or dyshomogeneous degenerative contents. No daughter cysts
Remarks: there is no living protoscoleces
CE5
Status: inactive
Image features: thick calcified wall which is arch-shaped, producing a cone-shaped shadow. Degree of calcification varies from partial to complete
Remarks: there is no living protoscoleces
1.
Type CL: early-stage echinococcosis disease, unilocular, cystic lesion with uniform anechoic content, not clearly delimited by an hyperechoic rim, cyst wall not visible.
2.
Type CE1: unilocular, simple cyst with uniform anechoic content. Cyst may exhibit fine echoes due to shifting of brood capsules which is often called hydatid sand (snow flake sign). Cyst wall is visible.
3.
Type CE2: multivesicular, multiseptated cyst in which the daughter cysts may partly or completely fill the unilocular mother cyst. Cyst septations may produce “wheel-like” structure, or the contained daughter cysts may produce a “rosette-like” or “honeycomb-like” structure. Cyst wall is normally visible.
4.
Type CE3: anechoic content with detachment of laminated membrane from the cyst wall visible as floating membrane or as “water-lily sign” which is indicative of wavy membranes floating on top of remaining cyst fluid. Unilocular cyst may contain daughter cyst. These cysts appear at US as a “complex mass.”
5.
Type CE4: heterogeneous hypoechoic or dyshomogeneous degenerative contents. No daughter cysts. It may show a “ball of wool” sign which is indicative of degenerating membranes.
6.
Type CE5: cysts characterized by thick calcified wall which is arch-shaped, producing a cone-shaped shadow. Degree of calcification varies from partial to complete.
Types CL, CE1, and CE2 are identified as active proliferative cysts. Type CE3 is identified as transitional cyst. Type CE4 is degenerative cyst. Type CE5 is inactive cyst.
The growth pattern of alveolar echinococcosis is similar to slow-growing liver cancer, so alveolar echinococcosis also has its PNM classification system [29]. This classification is summarized in Tables 19.2 and 19.3.
Table 19.2
The PNM classification of alveolar echinococcosis
P—Parasitic location in the liver |
Px Primary lesion can’t be estimated |
P0 No lesion in the liver |
P1 Peripheral lesion without biliary or proximal vessel invasion |
P2 Central lesion with biliary or proximal vessel invasion in one lobe of the liver |
P3 Central lesion with biliary or proximal vessel invasion in two lobes of the liver and/or invasion to two hepatic veins |
P4 Any lesion grows along portal vein, inferior vena cava, or hepatic vein |
N—Neighboring organs |
Nx Can’t be estimated |
N0 No infiltration to surrounding tissue |
N1 Infiltration to neighboring tissue and organs |
M—Metastasis |
Mx Can’t be estimated |
M0 No metastasis by chest X-ray and brain CT |
M1 No metastasis |
Table 19.3
Stage of alveolar echinococcosis based on PNM classification
Staging | P | N | M |
|---|---|---|---|
I | P1 | N0 | M0 |
II | P2 | N0 | M0 |
IIIa | P3 | N0 | M0 |
IIIb | P1~3 | N1 | M0 |
IV | P4 | N0 | M0 |
P4 | N1 | M0 | |
Any P | Any N | M1 |
19.7 Surgical Indication and Preoperative Preparation
Now, drug therapy, percutaneous puncture treatment, and operation are the three principal treatments for hepatic hydatid disease. Operation is the most effective treatment for hepatic hydatid disease, and it is the only way to cure echinococcosis radically.
No Surgical Indication
1.
Patients with type CL cyst who have no clinical symptoms, and the diameter is less than 5 cm.
2.
Totally calcified cyst is generally inactive cyst.
Preoperative Preparation
At present, there is still no exact conclusion as to whether there is a need to use chemotherapy before operation. Albendazole is the most effective drug for the treatment of hepatic hydatid disease in clinic. A small sample retrospective study shows that there were only 28 % hydatid cysts still living during the operation if the patient took albendazole for a month before operation. If chemotherapy using albendazole lasted 3 months, the activity of cysts decreases to 8 % [30]. Therefore, albendazole is an effective added therapy before operation. To date, there is no study showing the exact usage of albendazole during the perioperative period. We advise starting to take albendazole at least 2 days before operation.
19.8 Selection of Operation
The principle of surgical treatment for CE is to remove all parasite groups, prevent capsule contents overflowing, close pipes connected with the cyst, and deal with residual cavity [31–33]. Removing as much parasitic tissue as possible is the key to treating and preventing recurrence. Removing parasitic tissue more thoroughly leads to a lower recurrence rate, but the operation risks increase, and vice versa [34]. Laparoscopic operation for the treatment of hepatic cystic echinococcosis has characteristics of small trauma and quick recovery, but the high risk of recurrence and planting of this method limits its application [35]. Operating methods used at present are the following:
19.8.1 Excision of Internal Capsule
This type of operation in the treatment of hydatid disease is the most classic, clinical application of more than 100 years of history; the operating method is simple and feasible, doctors and medical equipment requirements are relatively low, and it is easy for all levels of hospital, but the operative complications (2.6–10 %) and the rate of recurrence (4.5–20.2 %) are higher [36–40].
Figure 19.1 shows the lesion site and lesion position containing 20 % NaCl solution gauze, preventing extravasation of the cystic fluid and allergic reaction. Two stitches hanging in the cyst wall, diagnostic puncture in two lines, pumping out the cystic fluid, preliminary judgment without infection or biliary fistula occurred, if the cyst fluid cool, no infection; suctioning clean of the cystic content, reinjection of slightly less than the protoscolex reagent kill suction quantity, currently recommend the use of 20 % NaCl solution [42], for 15 min, once again suction clean the cystic content. (see below)
Fig. 19.1
Showing the lesion site
Bluntly dissect and remove the jellylike endocyst (see Fig. 19.3) below
Fig. 19.3
Bluntly dissect and remove the jellylike endocyst
had been soaked in 20 %NaCl solution gauze wipe repeatedly external capsule wall, note there is no bile leakage, carefully and find out the external capsule wall fistula, for by the cystic duct injection of methylene blue check without biliary fistula wound. See below as found in the fistula with thread or 4–0 vascular suture closure of the fistula routine abdominal drainage tube; the wound larger when necessary feasible “T” tube drainage of common bile duct. See Figs. 19.4 and 19.5 below.
Fig. 19.4
Check bile leakage
Fig. 19.5
Closure of the fistula
19.8.2 Total Cystectomy
Cyst enucleation takes place along the gap between the internal and external capsule of the cyst; the operation wound is small in liver resection, but the process of stripping of echinococcosis rupture spreads risk, and there is also the risk of biliary fistula.
Incise the liver capsule; find out the space between external capsule and outer cystic membrane; (Fig. 19.7)
Fig. 19.7
Find out the space between external capsule and outer cystic membrane
along the gap spiral turn to deep stripping external capsule, until the whole external capsule is completely stripped (Fig. 19.8);
Fig. 19.8
Stripping external capsule
in the stripping process, should be carefully distinguished by the outer bag oppression of intrahepatic duct system, the membrane and the pipeline system integrity retained in the liver parenchyma on one side, the pipeline system to the outer sac ligation of membrane (Fig. 19.9);
Fig. 19.9
The pipeline system to the outer sac ligation of membrane
check whether the biliary fistula and bleeding, the full treatment, plasma layer placed drainage tube after abdominal closure.
19.8.3 Liver Resection
The cyst along with normal liver tissue around a certain range is resected. The operating method is thoroughly reliable [41], and there is no residual cavity, so this method can effect a radical cure to problems, depending on the site selection of the cyst for anatomical liver resection or non-anatomical liver resection.
For hepatic hydatid, whether cystic or alveolar, hepatectomy is a radical method. Liver resection can be divided into anatomical liver resection and non-anatomical liver resection. Operating methods can be divided into hepatic segment resection, lobectomy of liver, hemihepatectomy and trisegmentectomy. Earlier, the operating method for liver resection was described in detail. Here, the emphasis is on the resection of liver hydatid.
In view of the clinical characteristics of alveolar hydatid disease, the difficulty of treatment is higher than that of cystic echinococcosis. Radical resection is the first choice for hydatid disease of the liver [43, 44]. In the whole operation for resection of the lesion, the process for malignant tumor treatment follows the “tumor-free principle.” Operation excision grades are as follows: (1) R0 resection (parasitic tissue is excised completely, without any residue), (2) R1 resection (the parasitic tissues are excised; microscopic examination shows positive margin), (3) R2 resection (the parasitic tissue is not completely removed, but the gross margin is positive). The R0 resection is regarded as radical resection; the other two approaches are considered palliative resection [45, 46]. Although radical resection is the first choice, if the lesion is larger, with invasion of the portal vein or inferior vena cava, then palliative resection combined with drug treatment can obtain good clinical efficacy [47]. The selection of a bubble-type liver resection as an example:
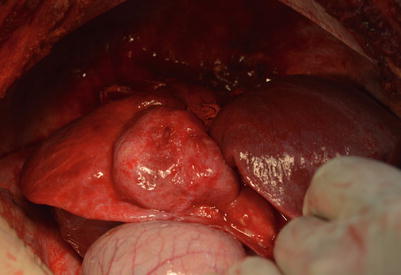
Alveolar hydatid showing invasive growth, invasion of the surrounding organs, as shown in Fig. 19.11.
Fig. 19.11
Invasion of the surrounding organs
Separation, organ and resection of hydatid violations such as graph (Fig. 19.12);
Fig. 19.12
Separation, organ and resection of hydatid violations such as graph
If the hydatid invades more than half of liver, it’s helpful to preset a blocking tape encircling the hepatoduodenal ligament, suprahepatic inferior vena cava and infrahepatic inferior vena cava, respectively (see Fig. 19.14).
Fig. 19.14
Preset a blocking tape encircling the hepatoduodenal ligament, suprahepatic inferior vena cava and infrahepatic inferior vena cava, respectively
If the lesion is localized in the hepatic segment, it is generally not necessary to block the hepatic portal, bleeding, temporary blocking of the hepatoduodenal ligament; if the lesion is localized to within half the liver, hemihepatectomy would be applicative with hemi-hepatic flow occlusion or directly cutting off the right hepatic artery and portal vein.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree