■ The surgical team setup is shown in FIG 2.
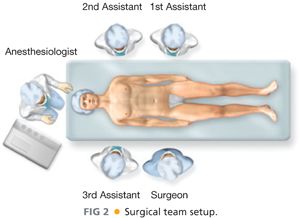
■ The surgical table must allow inclinations in every way, which will be necessary to expose regions with difficult access, such as the splenic flexure of the colon.
■ The patient must be secured to the surgical table adequately to prevent body displacements with position changes of the surgical table.
TECHNIQUES
LAPAROTOMY, REVISION OF PERITONEAL CAVITY, AND SURGICAL FIELD PREPARATION
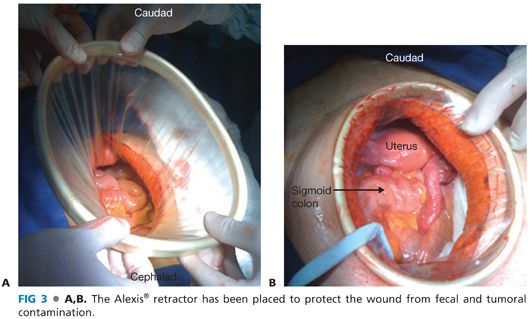
■ A medial supra- and infraumbilical laparotomy is performed, carrying the incision down to the pubis, which will improve pelvic exposure. Once the abdominal cavity is opened, it is advisable to protect the wound edges from bacterial and cellular contamination by placing an Alexis® wound protector or similar instrument (FIG 3A,B).
■ Following this, one should explore the abdominal cavity, emphasizing in the search for liver metastases and synchronous colon tumors, especially in patients in which the total colonoscopy was not possible due to an obstructive tumor.
■ Next, the small bowel is displaced toward the right upper quadrant of the abdomen and contained using pads and abdominal rolls. I personally prefer not to eviscerate the patient because this increases manipulation of the intestines and therefore increases the possibility of postoperative ileus. In order to achieve good pelvic and distal descending colon exposure, the patient is placed in a Trendelenburg position. A slight inclination of the surgical table toward the right can be helpful. Placement of a Bookwalter retractor facilitates operative exposure.
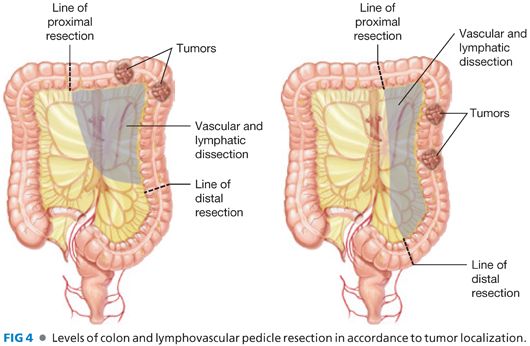
■ The exact location of the left colon tumor is identified and the extent of colonic and lymphovascular pedicle resection is defined (FIG 4).
IDENTIFICATION OF THE LEFT URETER AND START OF LEFT COLON MOBILIZATION
■ The sigmoid colon is retracted toward the right side, and the lateral peritoneal fold is exposed up to the pelvic ring.
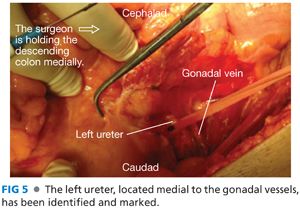
■ Peritoneal sectioning is initiated with the monopolar electrocautery in a cephalocaudal direction. The loose retroperitoneal tissue is exposed and it can be separated with a combination of blunt and sharp dissection in order to identify the gonadal vessels, the left ureter, and the left common iliac artery. It is useful to know that the left ureter is always medial to the gonadal vessels, crossing over the common iliac artery prior to its bifurcation. The left ureter is marked with a vessel loop, being careful of including its accompanying longitudinal vascularization (FIG 5).
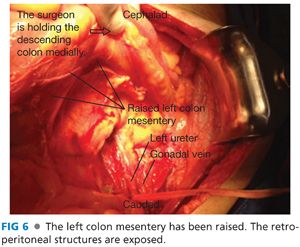
■ At this point, an avascular tissue plane located in between the ureter and the gonadal vessels in the back and the mesentery of the sigmoid and descending colon in the front should be searched for. Using blunt dissection, it is possible to separate these structures in a cephalad direction, staying in front of Gerota’s fascia, which should be preserved intact. Meanwhile, the descending colon mesentery is elevated. At the end of this maneuver, the descending colon mesentery will be raised, containing the inferior mesenteric artery (IMA) and its branches and the inferior mesenteric vein and its tributaries (FIG 6).
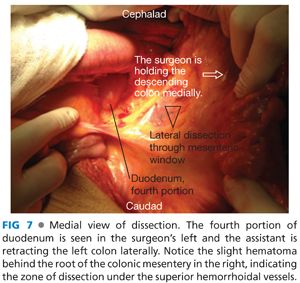
LATERAL TO MEDIAL DISSECTION AND VASCULAR ISOLATION
■ The sigmoid and descending colon are retracted laterally, and the peritoneum is sectioned in a vertical direction from the ligament of Treitz to the pelvic inlet, anterior to the aortic artery pulse. At this time, it is possible to see a slight hematoma behind the root of colonic mesentery, product of the previously described lateral dissection. Sectioning the loose tissue in the mesentery root (under the superior hemorrhoidal vessels) communicates the medial and lateral dissection planes (FIG 7).
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








