Fig. 27.1
A three-dimensional virtual multi-imaging derived from FDG-PET/CT scan, CT colonography, and CT angiography (right). The tumor is indicated in green, and the metastatic lymph nodes are indicated in red by FDG-PET/CT scan, and the entire colon is visualized by CT colonography (left). The arteries and veins related to the tumor are also visualized by CT angiography
Fig. 27.2
Dissection area with complete lymphadenectomy, depending on the tumor location
Here, we introduce our techniques for RPLLC with D3 lymphadenectomy. Our medial-to-lateral approach makes it possible to standardize the procedure for mobilization of the mesentery, ligation of the vessels at their origin, and complete lymphadenectomy in a safe and a certain manner.
27.2 Indications and Contraindications
Indications for RPLLC, like those for MLC, are Tis-T3 tumor, tumor diameter <4 cm, body mass index (BMI) <35 kg/m2, and American Society of Anesthesiologists (ASA) class <2. Advanced T4 tumor, a huge or bulky tumor ≥4 cm, severe obesity, perforated tumor, stenosis with bowel distention, prior abdominal polysurgery, and any severe comorbidity are contraindications. Complete informed consent is imperative.
27.3 Technique
27.3.1 Patient Positioning and Operative Set-up
The patient, under general anesthesia, is positioned on the operating table between sides supports mounted on the table. The patient’s feet are placed in boot-type leg holders with the legs spread apart and knees only slightly flexed. The arms are tucked along the patient’s sides. The operator, the camera assistant, and the scrub nurse stand on the right of the patient, and the first assistant and the laparoscopic monitor are on the left.
27.3.2 Access to the Abdominal Cavity
A 2–3-cm vertical skin incision and mini-laparotomy incision are made in the umbilicus. A multichannel access device such as EZ Access (Hakko Co., Nagano, Japan) with a previously installed 12-mm trocar for the laparoscope and two 5-mm trocars is fitted into the incision. We prefer to use ultrasonic laparoscopic coagulation shears (LCS) as the dissection device and atraumatic graspers or fine dissectors as forceps. An additional incision or trocar port is made without hesitation if necessary to complete the procedure, and conversion to open laparotomy is kept as an option. The indication and timing of trocar insertion or conversion to open surgery depend on the surgeon’s judgment.
27.3.3 Operative Exposure
CO2 pneumoperitoneum is established and maintained at 10 mmHg. After complete exploration of the abdomen to identify any metastatic nodules or superficial hepatic metastases with a 30-degree 10-mm rigid laparoscope, the patient is tilted into a deep Trendelenburg position and inclined to the right. The small intestine is moved into the right upper quadrant, exposing the root of the left colonic mesentery. The greater omentum is then flipped to expose the transverse colon and the splenic flexure.
27.3.4 Dissection of the Left Colonic Mesentery and the Mesorectum
By tenting the left colonic mesentery with an atraumatic grasper held in the surgeon’s left hand, the root of the left colonic mesentery is incised with LCS, starting at the sacral promontory, in a medial to lateral approach. The appropriate plane is dissected, preserving the right hypogastric nerve (Fig. 27.3). Continuous dissection below the inferior mesenteric artery (IMA) is performed by sweeping down the retroperitoneal fascia to preserve the left ureter and the gonadal vessels in the posterior plane (Fig. 27.4a). The mesorectum is dissected posteriorly in the plane of total mesorectal excision, in front of the hypogastric plexus nerves. The peritoneum is then incised cephalad beside the duodenum beyond the origin of the IMA (Fig. 27.4b). The medial dissection is continued until the inferior border of the pancreas on Gerota’s fascia is reached.
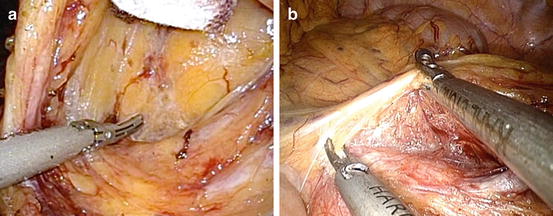
Fig. 27.3
Medial-to-lateral approach for dissection of the left colonic mesentery and the mesorectum, preserving the right hypogastric nerve
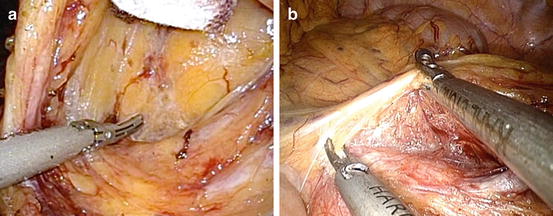
Fig. 27.4
(a) Dissection below the inferior mesenteric artery (IMA) by sweeping down the retroperitoneal fascia to preserve the left ureter and gonadal vessels. (b) Cephalad incision of the peritoneum beside the duodenum beyond the origin of the IMA
27.3.5 Ligation of the Inferior Mesenteric Vessels
The inferior mesenteric vessels are ligated, depending on the tumor location. When there is a need to ligate the IMA at its origin, the IMA is dissected between clips 0.5-cm away from its aortic origin so as not to injure the lumbar splanchnic nerves. When possible, to preserve blood flow to the superior rectal artery (SRA), the left colic artery (LCA) is dissected between clips at its origin with or without D3 lymphadenectomy around the origin of the IMA (Fig. 27.5a, b). The inferior mesenteric vein is exposed and dissected below the duodenojejunal junction between two clips (Fig. 27.6a, b).
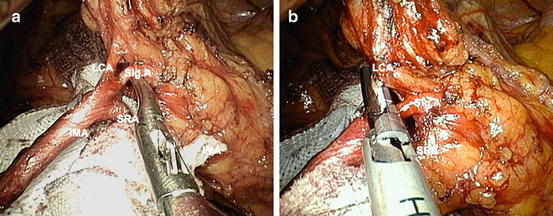
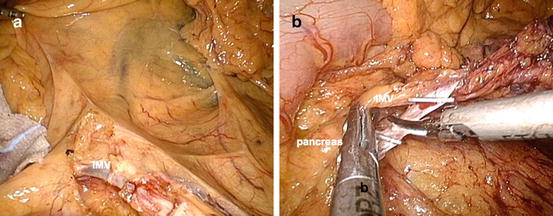
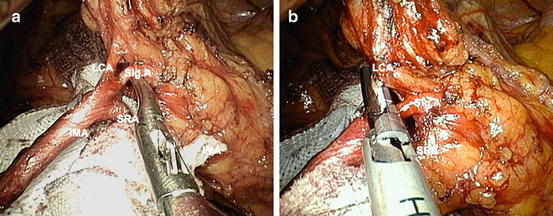
Fig. 27.5
(a) To preserve the superior rectal artery (SRA), skeletonization of the IMA and its branches with D3 lymphadenectomy around the origin of the IMA is performed. (b) Ligation of the left colic artery (LCA) by clips at its origin, preserving the SRA
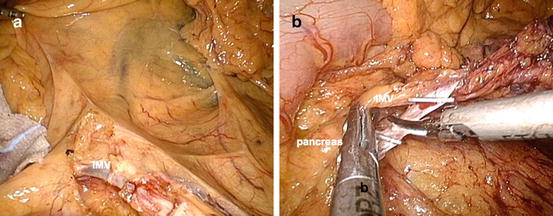
Fig. 27.6
(a) Exposure of the inferior mesenteric vein (IMV) below the duodenojejunal junction. (b) Ligation of the IMV between two clips
27.3.6 Mobilization of the Splenic Flexure
The lateral attachment of the left colon and rectum is dissected from bottom to top and is freed up to the splenic flexure (Fig. 27.7a). The operating table is then moved to a head-up position (reverse Trendelenburg position) in preparation for mobilization of the splenic flexure. The greater omentum is lifted cephalad with a retracting device such as the EndoGrab Retractor (Virtual Ports Ltd., Caesaera, Israel), and the transverse colon is pulled caudad with an atraumatic grasper held in the surgeon’s left hand. Thus, the greater omentum is separated by sharp dissection from the middle of the transverse colon to the splenic flexure by opening the bursa omentalis (Fig. 27.7b). The root of the transverse colonic mesentery is dissected laterally and freed from the inferior border of the pancreas (Fig. 27.8a, b). The splenic flexure is mobilized completely with sharp division of the splenocolic ligaments joining previous dissection of the left Toldt fascia (Fig. 27.9a, b).
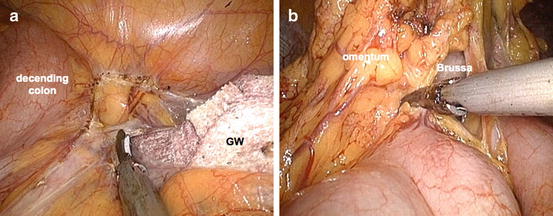
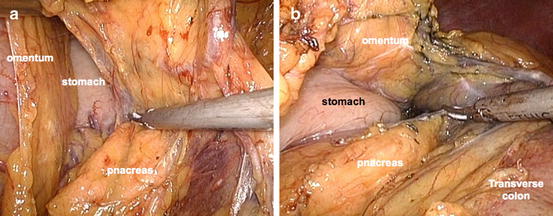
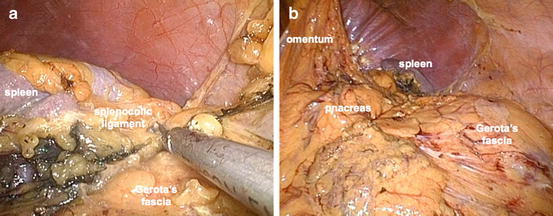
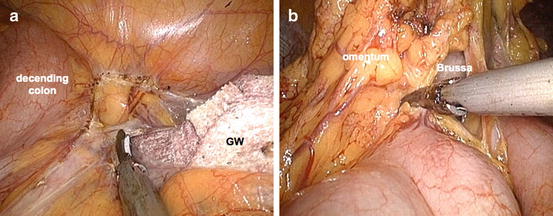
Fig. 27.7
(a) Dissection of the lateral attachment of the left colon up to the splenic flexure. (b) Separation of the greater omentum from the middle of the transverse colon to the splenic flexure by opening the bursa omentalis
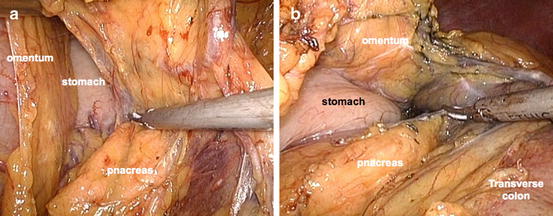
Fig. 27.8
(a) Dissection of the root of the transverse colonic mesentery laterally from the inferior border of the pancreas. (b) Complete separation of the transverse colonic mesentery from the surface of the pancreas
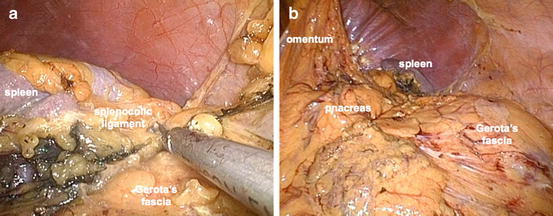
Fig. 27.9
(a) Mobilization of the splenic flexure with sharp division of the splenocolic ligaments. (b) Complete mobilization of the splenic flexure joining the previous dissection of the left Toldt fascia
27.3.7 Transection of the Rectum
When the IMA is ligated at its origin, the fat surrounding the rectum at the transection line, and usually near the promontory below Sudeck’s point, is removed, and the superior rectal vessels are dissected. In preparation for transection of the rectum, a 5-mm trocar in the access device is changed to a 12-mm trocar for the introduction of a linear stapler. The rectum is clamped and transected by one firing of an articulated linear stapler with a 60-mm cartridge. The rectum is drawn cephalad so that the staple line is perpendicular to the axis of the rectum. When the SRA is preserved, the mesentery is dissected cuneately at least 10-cm both distal and proximal to the lesion from the ligated stump of the LCA.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








