Fig. 4.1
Egg crate mattress

Fig. 4.2
Trendelenburg position
The patient is then fitted with a uterine manipulator to allow for greater movement and fewer ports to achieve the desired angles at which to operate. For the laparoscopic supracervical hysterectomies, we have been using a reusable Hulka tenaculum, and for the total laparoscopic hysterectomy, a VCare uterine manipulator (ConMed Endosurgery; Utica, NY) to outline the vaginal cuff. Other manipulators are on the market and can work equally well for these procedures.



Fig. 4.3
Hulka tenaculum

Fig. 4.4
VCare uterine manipulator (Courtesy of ConMed Endosurgery, Utica, NY)
Entry into the abdomen is gained through the use of trocars with the initial placement of a 5-mm trocar into the umbilicus for uteri up to 14 weeks in size and above the umbilicus for uteri larger than 14 weeks. This allows for adequate visualization of the pelvic structures. Accessory trocars are placed on the right and left sides traditionally 2 cm superior and medial to the anter-superior iliac spine under direct vision. We have found that this placement is often not adequate for good operating angles, and we prefer to determine placement at the time of insufflation with CO2 gas once the patient is placed in the Trendelenburg position. The size of the uterus and the pelvic pathology, such as adhesions and endometriosis, determine the placement, with a 5-mm trocar placed on the patient’s right side and a 10-mm one placed on the patient’s left side for laparoscopic supracervical hysterectomy. Larger uteri, such as those greater than 18 weeks in size, require a 5-mm trocar for the camera above the umbilicus and 10-mm trocars on each side, since 10-mm instruments are needed for movement of the large uterus secondary to the torque (smaller instruments may bend). Placement is decided at the time of insufflation once the angles needed for surgery are determined.



Fig. 4.5
Standard trocar placement

Fig. 4.6
Trocar placement for large uteri
For total laparoscopic hysterectomy, 3-mm, 5-mm, and one 10-mm port are used with a 5-mm port placed either in or above the umbilicus and 5-mm ports placed in the right and left lower quadrants as determined by the anatomy. A 10-mm port is then placed on the patient’s left side in the middle quadrant for suture introduction and sewing. These ports are moved cephalad if the uterus is larger. The insufflation tubing is placed on one of the lateral 5-mm ports, and smoke evacuation is placed on one of the ports on the opposite side. Removal of smoke or water vapor from lysed tissue is essential for good visualization. The recent introduction of the AirSeal insufflator (Surgiquest; Millford, CT), allows heated insufflation and smoke evacuation from a single port and protects the pneumoperitoneum, which is an advantage in total laparoscopic hysterectomy and obese patients.
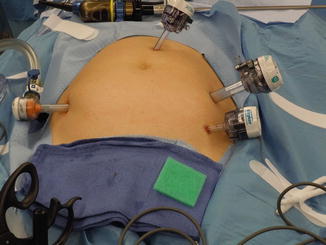

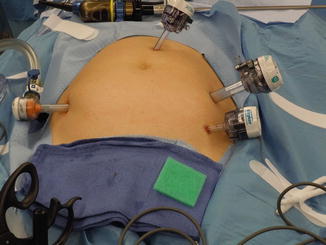
Fig. 4.7
Total laparoscopic hysterectomy trocars

Fig. 4.8
AirSeal insufflator (Courtesy of SurgiQuest, Milford, CT)
The general instrumentation for the standard laparoscopy is available in most operating rooms. Graspers such as bowel graspers and Maryland forceps as well as tenacula and laparoscopic scissors are used to manipulate the tissue and move the bowel. Electrosurgical devices are used to coagulate the blood vessels and cut the tissue. We tend to use the Sonicision Shears (Covidien Ltd.; Boulder, CO) for most dissection, vessel sealing, and cutting, as this one instrument can be used rather than several for tasks such as removing the uterus from the cervix in LSH and removing the cervix from the vagina in TLH. Large pedicles such as the infundibulo-pelvic ligament or uterine vessels are coagulated first with standard reusable bipolar cautery forceps with an impedance generator as an added precaution. Other vessel sealing and ligation devices are also available such as EnSeal (Ethicon Endo-Surgery Inc.; Somerville, NJ) and LigaSure (Covidien Ltd.; Boulder, CO).


Fig. 4.9
Sonicision (Courtesy of Covidien Ltd., Boulder CO)
4.2 Procedure for Total Laparoscopic Hysterectomy
When the patient is asleep and in the lithotomy position, a bimanual examination is performed to evaluate the size of the uterus and any additional disease that may be present. Standard prophylactic preoperative antibiotics are given for hysterectomy. A standard Foley catheter is placed to drain the bladder during the procedure, although a two-port catheter may be useful if lower uterine segment adhesions are anticipated in order to inject dye to delineate the borders of the bladder in a scarred environment. We use a paracervical block with bupivicane and epinephrine to decrease pain post-procedure. If using a VCare uterine manipulator, the cup should be sutured to the cervix to aid in retrieval of the specimen. Once the uterine manipulator is placed, a 5-mm laparoscope is placed in the camera port. With the patient in the steep Trendelenburg position, full inspection of the abdomen and pelvis is performed. The uterus and adnexal structures are evaluated. Placement of the accessory ports is then done once in the Trendelenburg position with a 5-mm port in the right and left lower quadrants and a 10-mm port in the left middle quadrant for TLH and a 5-mm port on the right and a 10-mm port on the left for supracervical hysterectomy.
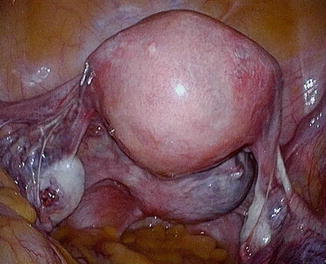
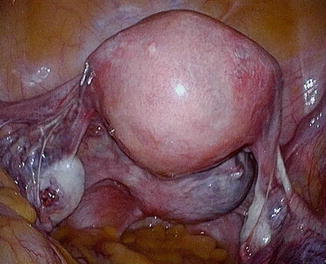
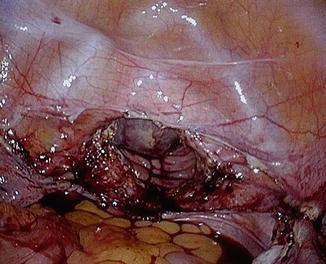
Fig. 4.10
Inspection of the pelvis
Step 1
The harmonic scalpel is then used to take the round ligament, utero-ovarian ligament, and tube on the left side as the first step in the procedure. If the ovary is to be taken, the infundibulopelvic ligament is coagulated first and then taken using the harmonic scalpel or another vessel-sealing device.
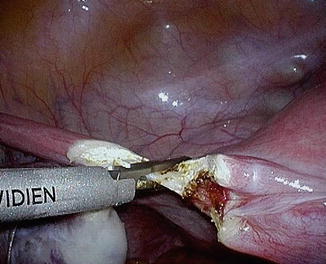
Fig. 4.11
Taking round and utero-ovarian ligament
Step 2
The broad ligament is opened, and the uterine vessels are exposed. This is done with harmonic energy to delineate the leaves using the cavitation effect of the harmonic scalpel. Alternatively, other vessel-sealing devices or plain monopolar scissors may be used for this step.
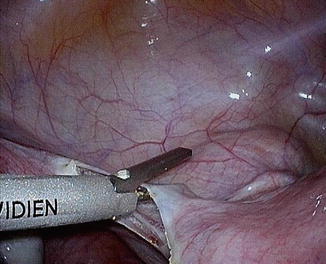
Fig. 4.12
Opening for broad ligament
Step 3
The bladder flap is then opened to expose the lower uterine segment and cervix as well as to move the bladder out of the way for the cervical dissection. Adhesions in this area are common, and sharp dissection is done to remove the bladder from the lower uterine segment. Injury to the bladder is common in this location, and if it occurs, it has been our experience to complete the dissection of the bladder from the cervix with adequate margins prior to repairing the bladder using a simple two-layer closure with polydioxanone (PDS) or Vicryl suture, usually 3-0 gauge.
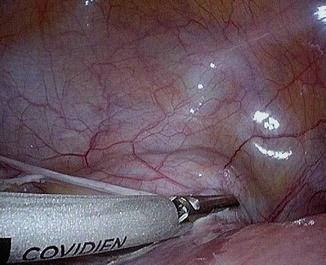
Fig. 4.13
Bladder flap
Step 4
The posterior peritoneum at the level of the lower uterine segment is opened using harmonic energy, a vessel-sealing energy source, or scissors with monopolar energy. Following this, the uterine vessels should be exposed and are coagulated with a bipolar cautery prior to incising the vessels using the harmonic scalpel. Technically, the harmonic scalpel should handle up to 7-mm vessels, which is appropriate for most uterine arteries, but our experience has been that bipolar cautery is often needed as a backup.
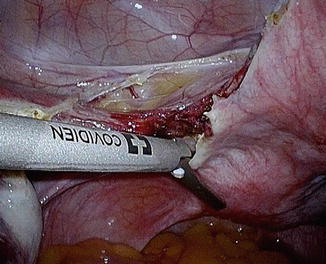
Fig. 4.14
Isolate and take uterine vessels
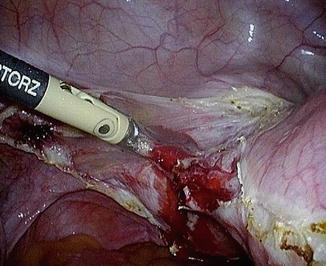
Fig. 4.15
Coagulation of the uterine artery
Step 5
This is a repeat of step 1, but on the right side, which involves taking the round ligament, utero-ovarian ligament (or infundibulopelvic ligament), and tube. The pedicles can either be taken with the harmonic scalpel or a vessel-sealing device or cauterized first with a bipolar cautery if the vessels are very large. Steps 2 and 3 are repeated on this side, as previously noted.
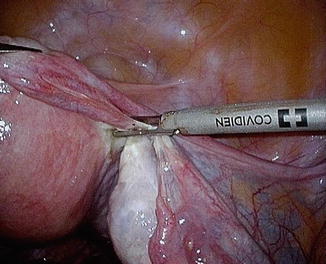
Fig. 4.16
Taking contralateral side
Step 6
The uterine vessels are isolated on the right side and coagulated with a bipolar cautery. The vessels are then moved laterally using the harmonic scalpel to move them over the cervical cup and well away from the vagina, leaving a 1- to 2-cm cuff for dissection. The ureters should be off to the side and well out of harm’s way. The blood supply to the uterus should now be completely isolated, and no further bleeding should occur.
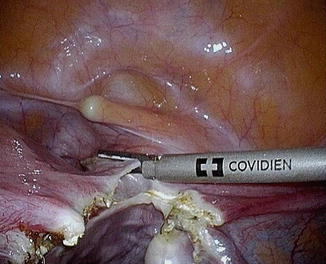
Fig. 4.17
Isolation of the uterine vessels
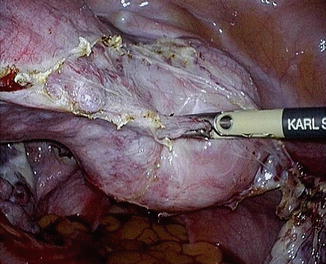
Fig. 4.18
Taking and moving of the cervical cup
Step 7
The cervix is then dissected free of the vagina using the harmonic scalpel or monopolar scissors or hook. The dissection occurs over the VCare cup, Rumi uterine manipulator (CooperSurgical; Trumbull, CT), McCartney transvaginal tube (LiNA; Glostrup, Denmark), a sponge on a sponge-stick, or other device that is being used in the vagina. The uterus is pulled into the vagina and the fundus is used to occlude the vagina and maintain the pneumoperitoneum. Alternatively, the uterus can be removed and a wet sponge placed in a glove or a similar device can be used to occlude the vagina. In the case of an excessively large uterus, vaginal morcellation can be accomplished in the standard fashion using a coring or bivalve technique to remove the uterus from the vagina.

Fig. 4.19
Dissection of the cervix
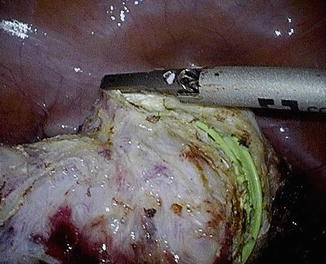
Fig. 4.20
Removal of the cervix
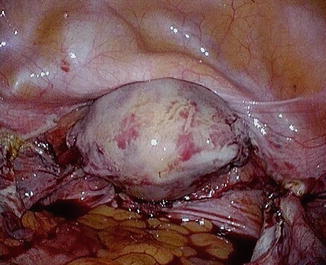
Fig. 4.21
Pulling of the uterus into the vagina
Step 8
Once removed from its vaginal attachments, the pedicles are inspected for bleeding. We have been using a modified Richardson stitch at the vaginal angles incorporating the uterosacral ligaments as originally described for open hysterectomy by Richardson in 1929 [12]. This involves placement of a stitch in a figure-of-eight fashion at the vaginal angles and taking the uterosacral ligament, being careful not to involve the vaginal mucosa when using a permanent stitch. Care must also be taken not to kink the ureter if using this stitch. We use number 1 prolene for this.