Laparoscopic Rectopexy
Howard M. Ross
Laparoscopic rectopexy is an important technique for the treatment of rectal prolapse. Laparoscopic rectopexy can be combined with sigmoid resection or performed alone as a means of treating full thickness rectal prolapse when resection is not desired. Laparoscopic rectopexy without resection is especially useful when patients have problems with fecal incontinence or when a patient or surgeon does not want to accept the risk of an anastomotic leak (1).
It is this authors and the editors’ practice to utilize a preoperative mechanical bowel preparation the evening prior to surgery. The mechanical preparation facilitates physical manipulation of the rectum with laparoscopic instruments.
Laparoscopic rectopexy is a relatively easily performed technique which includes full circumferential mobilization of the rectum to the level of the pelvic floor. Surgeons should be facile with endoscopic suturing techniques and have equipment which will permit the secure attachment of the mesorectum to the presacral fascia.
Positioning
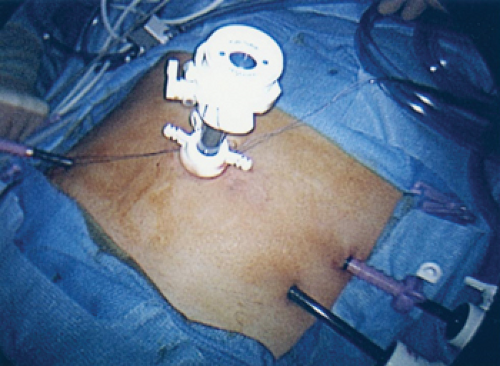
Patients should be placed in supine position in stirrups. The patient’s thighs should be parallel to the torso to enable the unencumbered motion of the surgeon’s arms. Generally a camera port is placed at the superior edge of the umbilicus, with two lateral 5 mm ports in both the right and left lower quadrants. A 30-degree telescope enables lateral viewing. On each side of the patient, the lowermost lateral port is placed two fingerbreadths anterior and superior to the iliac spine. The more superior lateral port is placed four fingerbreadths superior to the lower port (Fig. 52.1).