Laparoscopic Partial Hepatectomy
Michael D. Kluger
Daniel Cherqui
 INDICATIONS/CONTRAINDICATIONS
INDICATIONS/CONTRAINDICATIONSAlthough laparoscopic liver surgery was first reported nearly two decades ago, it has not received wide attention until relatively recently. Different resections require varying levels of expertise, but all require familiarity with preoperative planning and perioperative care of the liver patient, open liver surgery, hepatic anatomy, and advanced laparoscopic principles. The 2008 Louisville Statement divides these operations among pure, hand-assisted and hybrid laparoscopy. Pure laparoscopy involves complete mobilization and resection via laparoscopic ports, although an incision may be used for specimen extraction. Hand-assisted laparoscopy involves the elective placement of a hand-port for mobilization or resection, which is then used for specimen extraction. Hybrid refers to a procedure where the resection is performed through a mini-laparotomy, though laparoscopy with or without hand assistance is utilized for mobilization. We favor pure laparoscopy for all resections.
Lesion size and location are the most important determinants of when laparoscopic resection is appropriate. Although there is variation in this evolving field as to what some centers will consider for laparoscopic resection. Table 31.1 details the indications and contraindications generally supported by high volume centers. Asymptomatic lesions convincingly recognized by imaging to be benign, that do not have harmful potential and would normally not be resected by laparotomy, should not be resected because laparoscopy is feasible.
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNINGEquipment and Instruments
All equipment must be state of the art, tested before each operation, and nursing staff should be familiar with proper set-up and functioning. In addition to an operating room
sized to accommodate the laparoscopy and liver transection instrument consoles, the following instruments and devices are necessary:
sized to accommodate the laparoscopy and liver transection instrument consoles, the following instruments and devices are necessary:
TABLE 31.1 Indications and Contraindications to Laparoscopic Partial Hepatectomy | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
An adjustable remote controlled electric split-leg table.
10 mm 30° laparoscope, high definition camera and xenon lighting. High definition monitors positioned lateral to each shoulder and above the patient’s head when the patient is supine, and across from the surgeon when the patient is in the left lateral decubitus position.
Two CO2 insufflators (12 mm Hg is used for the prevention of gas embolism) with full tanks. Two insufflators are preferred, as intermittent suction is necessary to maintain a smokeless field when using diathermy instruments on liver parenchyma.
Comfortable ergonomic laparoscopic instruments, including ratcheted fenestrated and atraumatic bowel forceps, curved and right angle dissectors, scissors, bipolar diathermy forceps, monopolar diathermy hook, needle holders and a liver retractor.
Disposable or reusable ports (5, 10, 12, and 15 mm), laparoscopic in-line and cutting vascular staplers, ultrasonic dissector, LigaSure or Harmonic devices, clip appliers (combinations of small, large, locking, absorbable and titanium), a suction-irrigator and a large specimen bag.
An ultrasound with B- and D-modes and a high frequency laparoscopic transducer.
5-0 Prolene sutures cut to 20 to 30 cm, umbilical tapes and tourniquet materials.
Scope warmer, as smoke and splattering affect the optics.
A set of conventional instruments and retractors for open surgery should be available.
An adequate back-up supply of all mentioned equipment.
Patient Preparation
A thorough history and physical examination should be performed to evaluate for medical disease or previous abdominal incisions that might complicate a laparoscopic approach. Severe cardiac, pulmonary, or renal disease should be further evaluated at the surgeon’s discretion. High quality magnetic resonance or computed tomography imaging with vascular reconstruction should be reviewed in order to evaluate for intrahepatic arterial and portal anomalies and to determine if the lesion is amenable to a laparoscopic resection (see Chapter 18). Informed consent should include a thorough discussion of the risks and benefits of laparoscopic surgery relative to the risks and benefits of open surgery, with a discussion of the possibility of conversion to an open resection.
Patients are preferably admitted 1 day preoperatively and routine labs are drawn, including a basic metabolic profile, complete blood count, coagulation series, liver function tests, and tumor markers. The patient is advised to take minimal fluids for 24 hours before surgery and kept NPO past midnight with the objective of low central venous pressure during the operation.
The operation can be divided into five stages that should be planned before proceeding to the operating room: (1) patient position; (2) port placement and ultrasonography; (3) mobilization, control of inflow/outflow and marking the liver; (4) parenchymal dissection, hemostasis, and biliary stasis; and (5) specimen extraction.
 SURGICAL TECHNIQUE I: GENERAL PRINCIPLES
SURGICAL TECHNIQUE I: GENERAL PRINCIPLESPertinent Anatomy
The liver is divided into eight segments on the basis of the divisions of the right and left portal veins according to the nomenclature of Couinaud (Fig. 31.1). Just as in open resection, laparoscopic resection is defined by the Brisbane 2000 terminology of liver anatomy and resections. Tumors 5 cm or less in size located in the anterolateral segments (i.e., 2, 3, 4b, 5, and 6) are most amenable to laparoscopic resection (Fig. 31.1). Other lesions require more advanced expertise. Liver anatomy has been described elsewhere in this book.
Patient Positioning
After patient and procedure confirmation, general anesthesia is induced and a central venous catheter, arterial line, large bore peripheral intravenous catheter, nasogastric tube, and Foley catheter are placed. Routine anesthesia monitoring includes heart rate, arterial blood pressure, pulse oximetry, capnometry, and esophageal temperature. Central venous pressure is measured as required and other monitoring utilized at the discretion of anesthesia (see Chapter 18). Perioperative antibiotics are given. Bilateral intermittent venous compression devices are placed and the abdomen is prepped from the neck to the groin and then covered with a steri-drape.
For all resections, the patient can be placed in the supine position with the lower limbs apart on a split-leg table. Both arms are padded and tucked at the sides. The surgeon stands between the legs, with an assistant at each side. The scrub nurse is positioned behind the surgeon along the right leg, with the instruments behind. A mayo stand positioned over the right leg holds the most commonly utilized instruments. Reverse Trendelenburg allows the bowels to drop into the lower abdomen and the table is tilted laterally as necessary to take advantage of gravity and the weight of the liver to improve exposure. An example of the room set-up and patient position is demonstrated in Figure 31.2 (see also Chapter 29 and Figs. 29.9, 29.10, 29.11, 29.12 and 29.13). For masses in segments 6 or 7, the patient can be placed in the left lateral decubitus position. The arms, legs, and left shoulder are padded and placed in physiologic positions. The surgeon and one assistant stand on the patient’s ventral side, with the scrub nurse opposite at the legs.
Port Placement, Exploration, and Ultrasonography
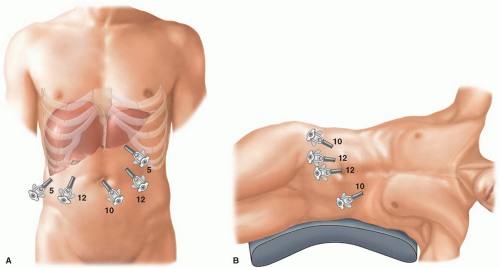
An open technique is used to gain access to the abdomen supraumbilically and a 10 mm port is placed to serve as the camera port. The remaining four ports are placed under
direct vision: Right and left para-median versa-step 5 to 12 mm working ports, and right and left lateral 5 mm ports for retraction instruments (Fig. 31.3). For left lateral decubitus positioning, four ports are used: a 10 mm in the left upper quadrant, a supra-umbilical 12 mm port, a 12 mm paraumbilical port in the mid-clavicular line, and a 10 mm trocar in the anterior-axillary line (Fig. 31.3). Port position may vary based on body habitus, but generally follow a curve from right to left similar to the profile of the liver.
direct vision: Right and left para-median versa-step 5 to 12 mm working ports, and right and left lateral 5 mm ports for retraction instruments (Fig. 31.3). For left lateral decubitus positioning, four ports are used: a 10 mm in the left upper quadrant, a supra-umbilical 12 mm port, a 12 mm paraumbilical port in the mid-clavicular line, and a 10 mm trocar in the anterior-axillary line (Fig. 31.3). Port position may vary based on body habitus, but generally follow a curve from right to left similar to the profile of the liver.
After a thorough inspection of the peritoneal cavity for ascites, carcinomatosis, and signs of portal hypertension, attention is turned to the liver for signs of superficial lesions, steatosis, cholestasis, cirrhosis, or other gross pathology. Laparoscopic ultrasound is systematically performed to confirm the location of the lesion, vascular anatomy, verify margins, and identify sub-centimeter lesions.
Mobilization, Control of Inflow/Outflow, and Marking the Liver
Liver mobilization requires freeing the liver’s ligamentous attachments from the diaphragm. Use of diathermy prevents bothersome bleeding, though the diaphragmatic and hepatic veins must be carefully avoided. The degree of liver mobilization is determined by the type of resection to be performed (see Chapters 19, 20 and 23):
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree