Laparoscopic Ileostomy
Bradford Sklow
William J. Peche
Laparoscopic ileostomy for fecal diversion is minimally invasive and can be accomplished with minimal morbidity (1,2,3). The laparoscopic approach offers the advantages of decreased pain, smaller incision, quicker return of bowel function, and shorter hospital stay. Most of the time a diverting loop ileostomy is constructed, but an end ileostomy can also be easily performed using the laparoscopic approach. The indications for performing a laparoscopic ileostomy for fecal diversion include fecal incontinence, rectovaginal fistula, perianal Crohn’s disease, obstructing unresectable colon cancer, and anastomotic leak (4). There are no absolute contraindications to performing a laparoscopic ileostomy, even in patients who are considered high risk or who have had previous abdominal surgery (5,6).
No bowel prep is needed or indicated. The patient should meet with an enterostomal therapy (ET) nurse to be marked with a permanent marker on their abdomen at the site for the planned ileostomy to ensure proper stoma location. Any questions can be answered and concerns addressed during that visit with an ET nurse. Preoperatively meeting with an ET nurse has been shown to reduce postoperative complications and problems with stomas, especially ileostomies (7,8).
The patient is positioned in the supine position on the operating room table. A beanbag is optional, but usually unnecessary for this procedure as long as the patient has been carefully secured to the table. Preoperative antibiotics consisting of a second-generation cephalosporin are administered within 1 hour of skin incision. The site of the planned ileostomy is scratched with a small needle as the marker ink can be wiped off during the prep of the skin. The operating surgeon stands on the left side of the table and a
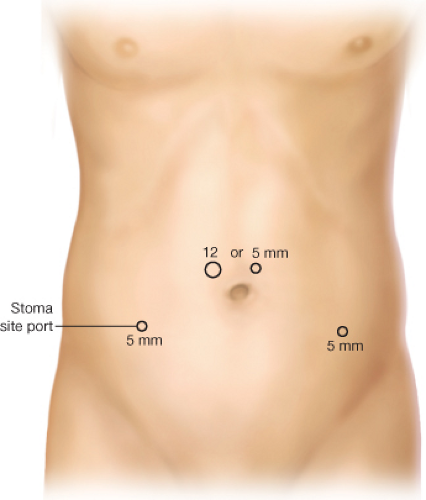
5-mm trocar is placed superior to the umbilicus after pneumoperitoneum is established using a Veress needle. A 5-mm, 30-degree laparoscope is inserted through the supraumbilical port. Alternatively, a 10-mm trocar can be placed using a direct Hassan technique above the umbilicus, and a 10-mm, 30-degree laparoscope is used (Fig. 41.1). An additional 5-mm port is placed on the left side of the abdomen two fingerbreadths medial and superior the left iliac crest (Fig. 41.1). An optional third 5-mm port can be placed through the planned ileostomy site on the right side of the abdomen (Fig. 41.2). Mobilization of the terminal ileum may be facilitated by releasing the lateral attachments along the pelvic brim up to the right gutter. The site of the stoma is chosen approximately
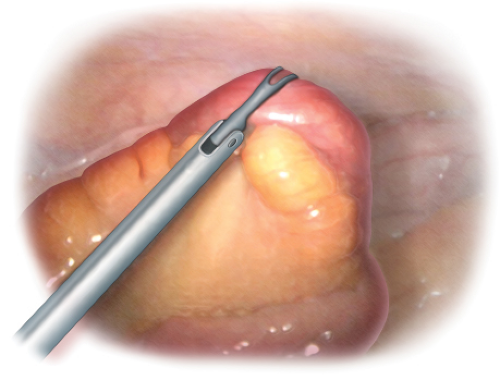
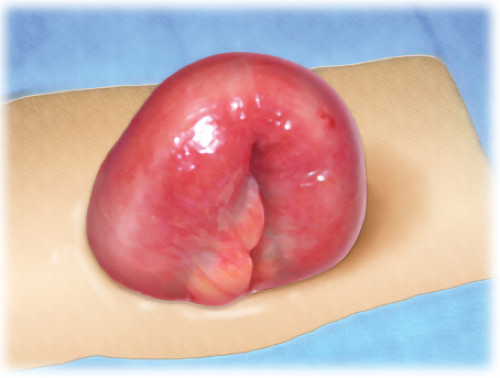
30–40 cm proximal to the ileocecal valve and grasped with an atraumatic bowel grasper (Fig. 41.3). The ileum is oriented with the grasper as not to twist the loop of ileum. The preselected stoma site on the right side of the abdomen is prepared by making a 2-cm diameter skin opening. The rectus muscle is opened to allow two fingers to pass with a muscle-splitting technique. The loop of ileum is delivered through the rectus muscle above the level of the skin (Fig. 41.4). A stoma rod may or may not be required to suspend the loop depending on the body habitus of the patient. The abdomen is then re-insufflated and the loop of ileum is visualized going into the stoma site to ensure that the ileostomy was not twisted during delivery through the abdominal wall. The distal limb is placed inferiorly and the functioning and is placed superiorly. At this point the ileum can be divided using an open surgical linear cutter to create a divided and loop stoma and the distal end tucked back into the abdomen below the fascia. This has the advantage of being completely diverting. The laparoscopic ports are removed, and the
port site incisions are closed with absorbable, subdermal sutures. Sterile dressings are applied prior to maturing the ileostomy. If a loop ileostomy is performed, an incision is made 80% around the circumference of the ileum. The proximal limb of the ileum will be everted as the functioning limb (Fig. 41.5). The proximal aspect of the stoma is Brooked above the level of the skin to the dermis with 3-0 absorbable sutures and the distal end is sutured flush to the dermis of the skin gathering the bowel wall to a small portion of the circumference of the skin opening at the most inferior part of the stoma site (Figs. 41.6 and 41.7). Ultimately, a stoma appliance is applied.
5-mm trocar is placed superior to the umbilicus after pneumoperitoneum is established using a Veress needle. A 5-mm, 30-degree laparoscope is inserted through the supraumbilical port. Alternatively, a 10-mm trocar can be placed using a direct Hassan technique above the umbilicus, and a 10-mm, 30-degree laparoscope is used (Fig. 41.1). An additional 5-mm port is placed on the left side of the abdomen two fingerbreadths medial and superior the left iliac crest (Fig. 41.1). An optional third 5-mm port can be placed through the planned ileostomy site on the right side of the abdomen (Fig. 41.2). Mobilization of the terminal ileum may be facilitated by releasing the lateral attachments along the pelvic brim up to the right gutter. The site of the stoma is chosen approximately
30–40 cm proximal to the ileocecal valve and grasped with an atraumatic bowel grasper (Fig. 41.3). The ileum is oriented with the grasper as not to twist the loop of ileum. The preselected stoma site on the right side of the abdomen is prepared by making a 2-cm diameter skin opening. The rectus muscle is opened to allow two fingers to pass with a muscle-splitting technique. The loop of ileum is delivered through the rectus muscle above the level of the skin (Fig. 41.4). A stoma rod may or may not be required to suspend the loop depending on the body habitus of the patient. The abdomen is then re-insufflated and the loop of ileum is visualized going into the stoma site to ensure that the ileostomy was not twisted during delivery through the abdominal wall. The distal limb is placed inferiorly and the functioning and is placed superiorly. At this point the ileum can be divided using an open surgical linear cutter to create a divided and loop stoma and the distal end tucked back into the abdomen below the fascia. This has the advantage of being completely diverting. The laparoscopic ports are removed, and the
port site incisions are closed with absorbable, subdermal sutures. Sterile dressings are applied prior to maturing the ileostomy. If a loop ileostomy is performed, an incision is made 80% around the circumference of the ileum. The proximal limb of the ileum will be everted as the functioning limb (Fig. 41.5). The proximal aspect of the stoma is Brooked above the level of the skin to the dermis with 3-0 absorbable sutures and the distal end is sutured flush to the dermis of the skin gathering the bowel wall to a small portion of the circumference of the skin opening at the most inferior part of the stoma site (Figs. 41.6 and 41.7). Ultimately, a stoma appliance is applied.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree