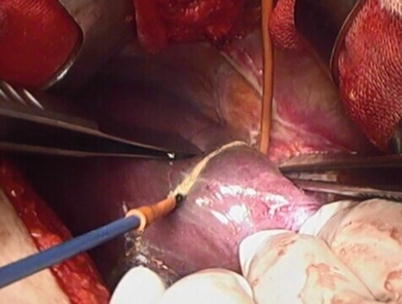
Fig. 32.1
Koffron maneuver
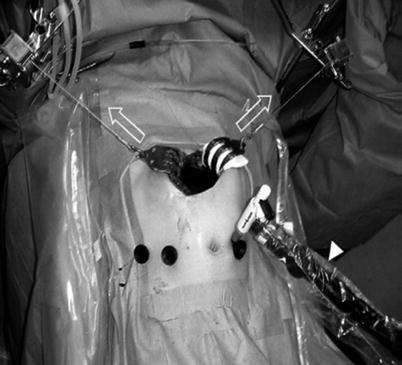
Fig. 32.2
Kurosaki maneuver
In 2009, Baker et al. [4] further confirmed the safety and feasibility of assisted laparoscopic living-donor liver resection on a group of patients. From 2006 to 2008, 33 cases of continuously conducted laparoscopically assisted open living-donor liver resection were reported. Among them, two cases were converted to open procedures to ensure the safety of the donor. Another two cases have undergone reoperation: one case developed damage from intestinal perforation, whereas another case developed a biliary fistula associated with incision dehiscence. The overall incidence of complications was 21 %, and there were no cases of perioperative death or serious complications. Compared with the earlier 33 cases of open surgery, the average duration of laparoscopic surgery was significantly shorter, whereas blood loss, postoperative hospital stay, complications, and graft survival were not significantly different.
32.2.3 Hand-Assisted Laparoscopic Liver Resection
In 2011, Suh et al. [5] reported a set of nine cases of laparoscopic living-donor liver resection. The first two cases involved hand-assisted laparoscopic liver resection, whereas the other seven cases involved laparoscopically assisted open surgery. In contrast with the Koffron reports, the transverse incision of the auxiliary device is approximately 9 cm in the right upper quadrant (Fig. 32.3). Although nine case operations were successful, two cases of hand-assisted laparoscopic surgery took 765 and 878 min, respectively, which is considerably longer than the duration of the laparoscopically assisted surgery cases (range, 310–575 min). In the report, they noted that although surgeon hand-assisted laparoscopic liver resection is feasible and safe (compared with laparoscopically assisted open surgery), laparoscopic liver resection with minimally invasive surgery has no greater advantage but does involve increased difficulty of operation and operative time, thus indicating the advantage of laparoscopically assisted open surgery over hand-assisted laparoscopic surgery.
Fig. 32.3
Hand-assisted laparoscopic liver resection
32.3 Anatomical Points of Laparoscopic Liver Resection
1.
Combined with preoperative radiographic evidence of clear structural anatomical features of the liver donor to develop an accurate donor liver resection program.
2.
Determine the variation and diameter of the bile duct branch.
3.
Determine the variation and diameter of the portal vein.
4.
Determine the variation and diameter of the hepatic artery.
5.
Determine the variation and diameter of the hepatic vein.
6.
Determine the variation and diameter of the right hepatic veins when the graft is the right liver.
32.4 Preoperative Assessment
1.
General assessment of the donor
Donors older than 18 years and less than 60 years must be informed and healthy and voluntarily decide to donate.
Donor’s height and weight are consistent with those of the recipient’s.
Living organ donor and recipient’s relationship must be in line with relevant laws and regulations.
Blood tests: ABO blood group and Rh blood group (matched or compatible).
Donor must have no history of any upper abdomen operations.
2.
Medical assessment of donor
Detailed history taking and physical examination, routine electrocardiogram, chest radiograph, and abdominal B ultrasound. Surgery can increase the risk of various acute and chronic diseases.
Blood (e.g., general testing, biochemistry, complete coagulation set, full hepatitis A panel, viral testing) and routine urine testing (culture).
Psychosocial assessment: professional psychologist assessment – exclude forced donation and potential economic interests from donation.
3.
Radiological assessment
Abdominal B ultrasound: understand the general situation and evaluate whether there is liver steatosis or fibrosis.
Upper abdominal CT measures the liver and graft volume: understand the anatomy of the portal vein, hepatic artery, hepatic vein, and inferior vena cava.
Abdominal magnetic resonance cholangiopancreatography (MRCP) to assess the biliary anatomy.
4.
Liver biopsy
It is necessary to understand whether there is liver steatosis and fibrosis.
5.
Endoscopic retrograde cholangiopancreatography (ERCP)
If necessary, ERCP should be conducted to understand the detailed biliary structure.
32.5 Laparoscopically Assisted Right Hepatectomy
1.
Navel channel is established. Explore abdominal cavity. Under direct vision, dissect the hepatic round ligament, position the blue dish, extend the left hand of the first assistant into the abdominal cavity to control the liver, tighten the blue dish, and reestablish the pneumoperitoneum (Fig. 32.4).


Fig. 32.4
Reestablish the pneumoperitoneum
2.
Use the hand-assisted ultrasonic scalpel to dissect in turn the liver sickle ligament (Fig. 32.5), the right triangular ligament (Fig. 32.6), the right coronary ligament (Fig. 32.7), and the right kidney ligament (Fig. 32.8); afterward, free the liver’s bare area to protect the right adrenal gland so that the entire right liver is completely freed.
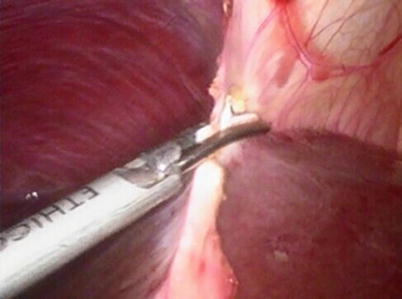
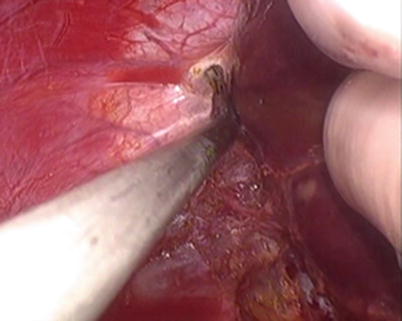
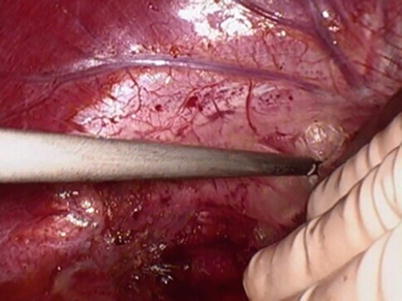
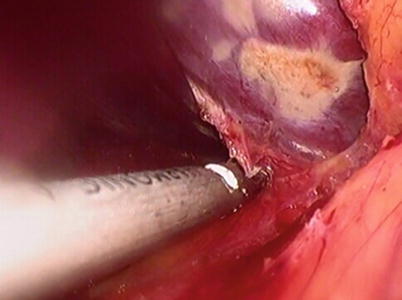
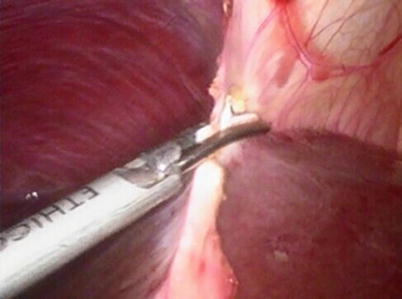
Fig. 32.5
Dissect the liver sickle ligament
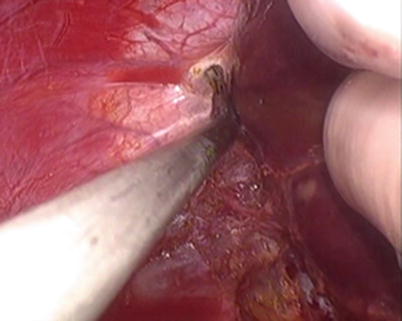
Fig. 32.6
Dissect the right triangular ligament
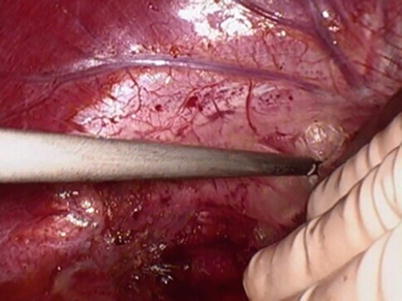
Fig. 32.7
Dissect the right coronary ligament
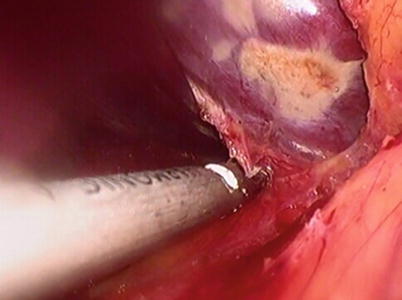
Fig. 32.8
Dissect the right kidney ligament
3.
Free from the bottom up; cut off all short hepatic veins immediately after the vein and inferior vena cava ligament so that they are completely separated from the hepatic inferior vena cava (Fig. 32.9).
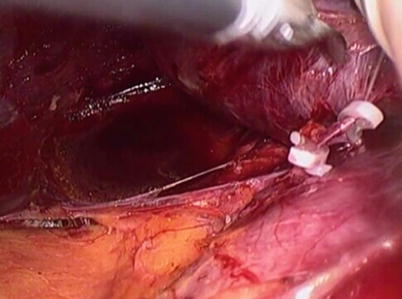
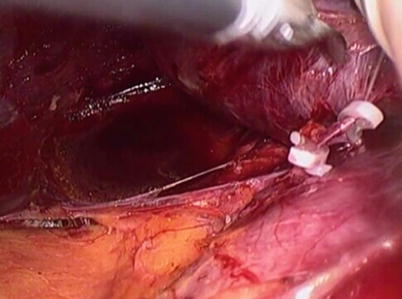
Fig. 32.9
Separated the hepatic inferior vena cava from liver
4.
Dissect the right hepatic vein in the boundaries between the right and middle hepatic veins, and concurrently position the 8th catheter, which is prepared as a guide for hepatectomy (Fig. 32.10).
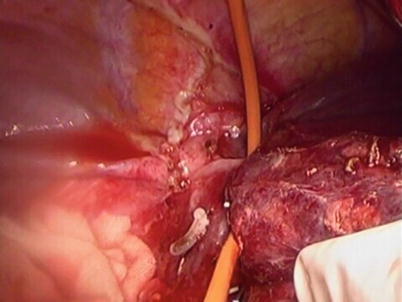
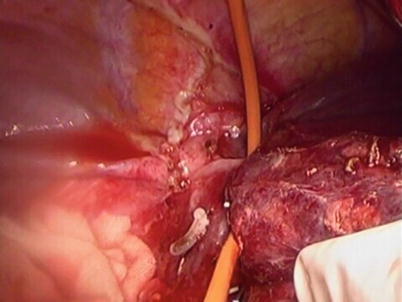
Fig. 32.10
Put an 8th catheter between the right and middle hepatic veins
5.
Remove all of the laparoscopic and hand-assisted equipment, extend the upper abdominal incision to 12 cm, perform cholecystectomy under direct vision, and insert the catheter into the cystic duct stump to perform cholangiography (Fig. 32.11).
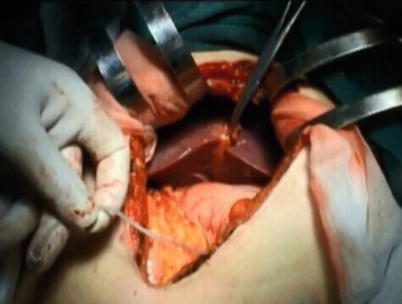
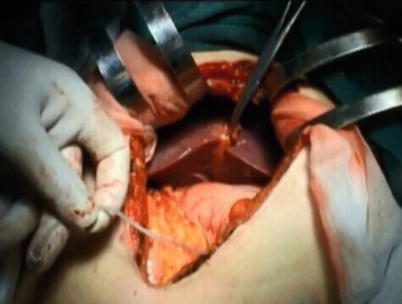
Fig. 32.11
Perform cholangiography
6.
Dissect the first porta hepatis: reveal the full length of the right hepatic artery and the bifurcation of the bile ducts (Fig. 32.12).
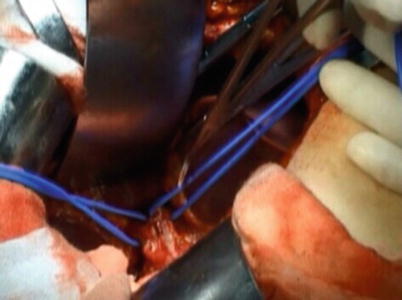
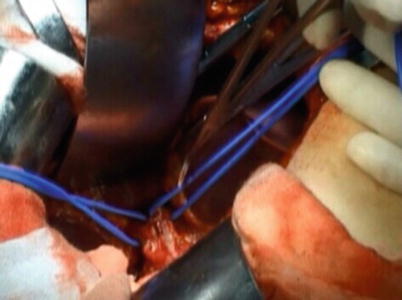
Fig. 32.12
Reveal the full length of the right hepatic artery and the bifurcation of the bile ducts
7.
Mark the dividing line in the left hepatic liver surface using the electric knife (gallbladder bed notch and right hepatic vein connection) (Fig. 32.13).