Laparoscopic
Charles B. Whitlow
David E. Beck
Colostomy formation is a procedure particularly well suited to laparoscopic techniques since there is no requirement for specimen extraction. While it is not as technically challenging as colectomy, it involves some of the same steps as colectomy and attention to detail is mandatory to ensure optimal results. This admonition is especially true for patients in whom a permanent stoma is being created, which may not always be known at the time of stoma formation.
There are numerous indications for colostomy, all with the ultimate need to divert the fecal stream from its normal anatomic egress. These indications include fistulizing perineal Crohn’s disease, rectovaginal fistula, diseases which require wide perianal skin excision with or without skin grafting, such as hidradenitis suppurativa, Buschke-Lowenstein type anal condyloma, and decubitus ulcers, fecal incontinence, radiation proctitis, obstructing/unresectable rectal cancer, anorectal trauma, and urethrorectal fistula.
For most indications, a sigmoid colostomy is superior to a colostomy created from more proximal colon. The ease with which the transverse colon can be delivered as a stoma is more than offset by the difficulty of ostomy care experienced by patients. In some cases ileostomy (described in a separate chapter) may be more appropriate or preferred to a colostomy. However, the surgeon should remember that in cases of distal obstruction, performing an ileostomy for diversion may not relieve the obstruction due to competency of the ileocecal valve.
Contraindications for laparoscopic procedures include the need for an open procedure or a history of extensive adhesions encountered during previous procedures. A history of previous abdominal surgery does not portend the presence of extensive adhesions.
One of the most important considerations for colostomy formation is proper siting of the stoma. Ideally the site is preoperatively marked with the assistance of an enterostomal therapist or wound ostomy continence nurse. The goals of siting are to select a location
within the borders of the rectus abdominis muscle, on a flat surface, which the patient can see. In many individuals this position will be at the cephalad apex of the infraumbilical fat pad. A location above or below the belt line is also dependent on the type of clothing that the patient typically wears. Additionally, the stoma should be away from scars, skin folds, and bony prominences. The proposed location must be verified with the patient supine, sitting, and standing and then marked. The marking technique will vary according to the urgency of the surgery and from the use of indelible markers or tattooing to mark the site.
within the borders of the rectus abdominis muscle, on a flat surface, which the patient can see. In many individuals this position will be at the cephalad apex of the infraumbilical fat pad. A location above or below the belt line is also dependent on the type of clothing that the patient typically wears. Additionally, the stoma should be away from scars, skin folds, and bony prominences. The proposed location must be verified with the patient supine, sitting, and standing and then marked. The marking technique will vary according to the urgency of the surgery and from the use of indelible markers or tattooing to mark the site.
Standard bowel preparation is not mandatory. However, because the empty colon intraoperatively handles better than the stool filled colon, it is the authors’ preference to have patients who can tolerate a preparation, ingest a limited isotonic lavage prep (one-quarter to half gallon of a polyethylene glycol solution). Patients are instructed to limit diet to only clear liquids the day prior to surgery. Oral antibiotics are not prescribed but standard intravenous broad-spectrum antibiotics are given within 1 hour of skin incision. Deep vein thrombosis prophylaxis is also ordered. Informed consent should include the potential for conversion to an open procedure.
Patient Positioning and Preparation
The patient is initially placed supine on a beanbag, gel pad, or cushion. After induction of general anesthesia, an orogastric tube and indwelling urinary bladder catheter are placed. The patient is then placed in modified lithotomy position with the thighs even with the hips and pressure points appropriately padded. One or both arms may be adducted to facilitate securing the patients for the extremes of positioning used during laparoscopy. The patient is then secured to the table, usually with tape. Rectal irrigation with tap water is performed until clear unless the patient has an obstructing lesion. The skin is prepped with antiseptic solution and draping is undertaken in a standard fashion.
Instrument/Monitor Positioning
The primary monitor is placed on the patient’s left near the level of the hip. A secondary monitor can be placed at the left shoulder or at an alternate site viewable by the surgical technician. Insufflation tubing, suction tubing, cautery power cord, laparoscopy camera wiring, and a laparoscope light cord are brought off the patient’s left side if possible. A 10 mm laparoscope with a 30-degree lens is preferred.
Port Selection and Placement
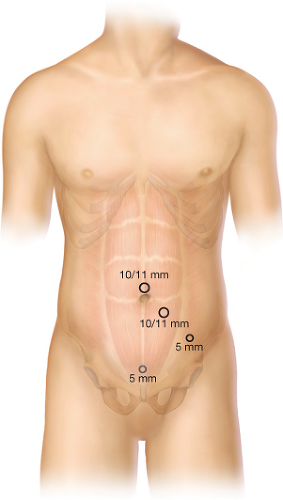
An umbilical or supraumbilical location is used for placement of a 10/11 mm port (Fig. 40.1). The port is placed using an open (modified Hasson) technique. Specifically, a vertical skin incision with a scalpel is followed by dissection down to the linea alba. An Ochsner clamp is used to elevate the midline at the level of the umbilical stump and the linea alba is then incised. S-shaped retractors are helpful in exposing the midline. Entry into the peritoneum is accomplished either bluntly with a Kelly clamp or sharply. A more cephalad midline or right upper quadrant site may be necessary if the selected stoma site is less than one hand’s breadth from the umbilicus or the patient has had multiple previous midline incisions. Once entry into the peritoneal cavity is obtained, a 10/11 mm blunt-tip balloon trocar is placed and secured. Alternatively, a 0 polyglycolic acid suture is placed into the fascia in a purse-string manner with which a standard 10/11 mm trocar is secured (12 mm if an end colostomy is planned).
Laparoscopic inspection of the peritoneal cavity is undertaken to exclude any unsuspected pathology. This time is also the time to identify if the patient has a redundant/mobile colon that does not require further mobilization. A second 10/11 mm port is then placed at the preoperatively marked stoma site. This port can be placed with a standard vertical skin incision or a 2 cm disk of skin can be excised prior to placement of the stoma-site trocar. A grasper is inserted and the sigmoid colon is identified and grasped. If the colon has sufficient mobility and reaches the abdominal wall with the pneumoperitoneum intact, then there is usually adequate redundancy to create a loop stoma. If this situation is identified, then the port at the preselected ostomy site is all that is needed.
Laparoscopic inspection of the peritoneal cavity is undertaken to exclude any unsuspected pathology. This time is also the time to identify if the patient has a redundant/mobile colon that does not require further mobilization. A second 10/11 mm port is then placed at the preoperatively marked stoma site. This port can be placed with a standard vertical skin incision or a 2 cm disk of skin can be excised prior to placement of the stoma-site trocar. A grasper is inserted and the sigmoid colon is identified and grasped. If the colon has sufficient mobility and reaches the abdominal wall with the pneumoperitoneum intact, then there is usually adequate redundancy to create a loop stoma. If this situation is identified, then the port at the preselected ostomy site is all that is needed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree