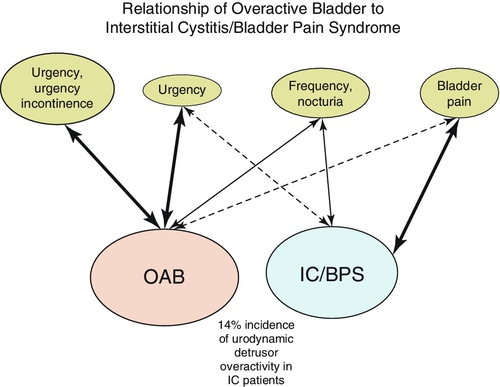
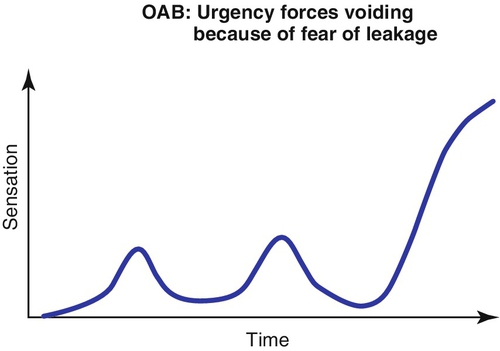
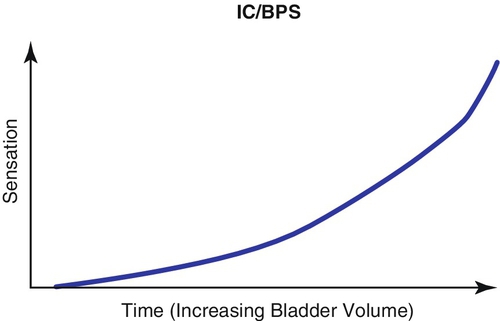
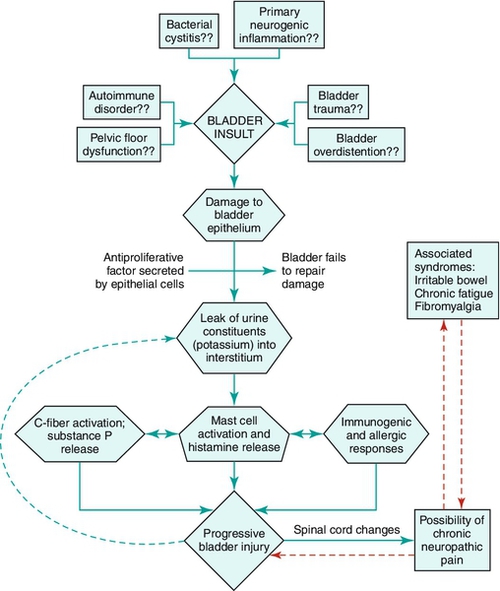
Chapter 7 Interstitial cystitis/bladder pain syndrome (IC/BPS) is a condition diagnosed primarily on the basis of clinical symptomatology. It requires a high index of suspicion on the part of the healthcare provider. It should be considered in the differential diagnosis of the patient presenting with chronic pelvic pain, often exacerbated by bladder filling and associated with urinary frequency. The sine qua non of the diagnosis is the presence of pain associated with the bladder. The older term interstitial cystitis (or IC) was not at all descriptive of the clinical syndrome and not accurate with regard to the pathologic findings. The reader should realize that the older term is still in use and common in the literature but gradually becoming less so. It is being replaced by the term bladder pain syndrome. American Urological Association guidelines have combined the terms. Originally considered a bladder disease, it is now positioned in the medical spectrum as a chronic pain syndrome that may begin as a pathologic process in the bladder in many, but not all, patients. In a small percentage of patients, it can progress into a disorder that even cystectomy may not benefit! IC/BPS encompasses a major portion of the painful bladder disease complex, which includes a large group of patients with bladder and/or urethral and/or pelvic pain, irritative voiding symptoms (urgency, frequency, nocturia, dysuria), and sterile urine cultures. Painful bladder conditions with well-understood and established etiologies included radiation cystitis, cystitis caused by microorganisms including some that are not detected by routine culture methodologies, and systemic disorders that affect the bladder. IC/BPS is a diagnosis of exclusion. It may have multiple causes and represent a final common reaction of the bladder to different types of insults. Essentially, one must be confident that the patient with IC/BPS is not actually suffering from any known treatable cause of bladder pain before making the diagnosis. The American Urological Association guideline defines IC/BPS as “An unpleasant sensation (pain, pressure, discomfort) perceived to be related to the urinary bladder, associated with lower urinary tract symptoms of more than 6 weeks duration, in the absence of infection or other identifiable causes.” The term interstitial cystitis (IC) has classically been used to describe the clinical syndrome of urgency/frequency and pain in the bladder and/or pelvis that is unrelated to any defined urologic pathology. When considering IC/BPS, the symptom of pain should be broadened to include pressure and discomfort. Urgency is left out of the definition of IC/BPS because it is the cardinal symptom of overactive bladder (OAB) (a confusable disease) and proves to be unnecessary for definition purposes. One can often separate out those patients with the hypersensitivity of IC/BPS from those with the urgency of OAB by doing a cystometrogram. The OAB patient will generally have uninhibited bladder contractions, whereas the IC/BPS patient will have a stable bladder with hypersensitivity during bladder filling. Simple questions will often suffice to differentiate between the two conditions. “Does your urgency to find a restroom come on suddenly, and is it because you are afraid you will wet yourself, or is it a more gradually appearing sensation of increasing pain and discomfort that you feel in the bladder area?” The former strongly suggests OAB, and the latter is most consistent with IC/BPS. OAB is over 10 times more common in the population than IC/BPS, and the treatment algorithm is very different, making the differential diagnosis critical (Figures 7-1, 7-2, and 7-3). Epidemiology studies of IC/BPS have suffered from the lack of a universally accepted definition, the absence of a validated diagnostic marker or clinical test that assures the diagnosis is made in a uniform manner by different clinicians in different geographic areas, and the lack of a pathognomonic finding on histologic biopsy of bladder tissue. There is considerable variability in studies on incidence and prevalence not only within the United States but around the world. The first population-based study included patients with interstitial cystitis in Helsinki, Finland. The prevalence was 18.1 per 100,000 women and 10.6 per 100,000 population. The annual incidence of new female cases was 1.2 per 100,000. Severe cases accounted for 10% of the total. Only 10% of total cases were in men. Another early population study from the United States in 1987 first demonstrated the potential extent of what had been considered a very rare disorder. It concluded that while there were 43,500 to 90,000 diagnosed cases of IC/BPS in the United States (twice the prevalence in Finland), up to a half million people had symptoms of painful bladder and sterile urine, considerably expanding the population of potentially affected individuals. The median age at onset was 40 years and there was a 50% remission rate not clearly related to therapy that lasted a mean of 9 months. More recent epidemiologic studies using different operational definitions have yielded wildly disparate data, from 35 to 24,000 per 100,000 in the United States, to 1.2 per 100,000 in Japan and 7 per 100,000 in the Netherlands. Most studies show a female-to male preponderance of 5:1 or greater. Population-based studies using the O’Leary-Sant Interstitial Cystitis Symptom Index generally show a prevalence of 300 per 100,000 persons. The Rand Corp., in the largest population-based study in the United States to date, suggested that 2.7% of the adult female population has symptoms suggestive of IC/BPS. In the absence of a validated marker, it may be difficult to differentiate chronic pelvic pain syndrome (CPPS) in men (nonbacterial prostatitis) from BPS. In males who have chronic pain they associate with the bladder in the presence of urinary frequency but in the absence of urinary infection, IC/BPS should be considered high in the differential diagnosis. Men with primarily pain complaints in the absence of any voiding dysfunction fit the more classic description of type 3 CPPS. Only 10% to 20% of patients with IC/BPS in most series have true isolated inflammatory bladder lesions on endoscopy that tend to crack and bleed with distention (Hunner lesions). Men tend to be diagnosed at an older age than women and have a higher incidence of Hunner lesion. All patients with presumed IC/BPS with microhematuria should undergo cystoscopy, urine cytology, and bladder biopsy of any suspicious lesion to be sure that a bladder carcinoma is not present. Bladder carcinoma in situ can result in symptoms similar to IC/BPS. It would seem that in the absence of microhematuria and with a negative cytology, the risk of missing a cancer is negligible but not zero. There is no evidence that IC/BPS itself is associated with a higher risk of bladder cancer or transitions to cancer over time. It is important that the clinician be aware of symptoms of the following disorders, which may be associated with some cases of IC/BPS: Depression, Sjögren syndrome, irritable bowel syndrome, allergies, fibromyalgia, chronic fatigue syndrome, dyspareunia, and focal vulvitis. It is likely that IC/BPS has a multifactorial etiology (Figure 7-4). A “leaky epithelium,” mast cell activation, neurogenic inflammation, primary pelvic floor dysfunction, and sequelae of bladder infection or pelvic surgery have all been proposed at one time or another. There is little data to support the role of an active infectious etiology, but it is conceivable that a viral or bacterial cystitis could begin the cascade that ultimately leads to a self-perpetuating process resulting in chronic bladder pain and voiding dysfunction.
Interstitial Cystitis/Bladder Pain Syndrome
Definition
Epidemiology
Etiology
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


