Chapter 45 Infections of the Biliary Tract
![]() Video related to this chapter’s topics: Biliary Tract Infections–Worms
Video related to this chapter’s topics: Biliary Tract Infections–Worms
Introduction
The histologic definition of cholangitis is inflammation of the bile duct. However, when used in practice, cholangitis refers to a characteristic clinical presentation associated with bile duct obstruction and bacterial infection. Other etiologies of bile duct inflammation have a preceding descriptor (e.g., parasitic cholangitis). All types of bile duct inflammation may be complicated by obstruction and secondary bacterial infection. The conditions predisposing to cholangitis are listed in Box 45.1.
Box 45.1 Conditions Associated with Cholangitis
Endoscopic Retrograde Cholangiopancreatography
Contraindications
Contraindications for ERCP in biliary tract infections are similar to other endoscopic procedures. Patients who are unable to tolerate conscious sedation because of cardiopulmonary disease require an anesthesia assessment. Patients with an allergy to contrast agents or iodine are at increased risk of a contrast allergy during ERCP. Premedication with steroids and use of a nonionic or low-osmolality contrast agent are recommended to reduce this risk.1
ERCP in pregnancy is apparently safe for both the mother and the fetus, whereas a delay in definitive treatment of cholangitis may be life-threatening. Radiation exposure to the fetus is limited by shielding the uterus with a lead apron, short periods of fluoroscopy, avoiding magnification, and avoiding hard copy radiographs.2
Preparation
The patient should be given nothing per mouth (NPO) after midnight the day before ERCP. Coagulopathy should be corrected if possible. A decision to discontinue anticoagulants or antiplatelet agents should be individualized. There is insufficient evidence to support routine discontinuation of aspirin and nonsteroidal antiinflammatory drugs before therapeutic ERCP procedures. Patients with a history of a contrast allergy are given prednisone, 20 mg by mouth, 13 hours, 7 hours, and 1 hour before the procedure.1 Conversely, the use of noniodinated contrast agents in place of premedication with steroids is favored by many clinicians. Antibiotics should be administered for prophylaxis of post-ERCP cholangitis if indicated.
Postprocedure Care
The efficacy of antibiotics after successful endoscopic therapy of cholangitis is unknown. In a retrospective analysis of 80 patients with cholangitis who underwent endoscopic therapy, there was no difference in outcome between the group receiving antibiotics for 3 days or less and the group receiving antibiotics for more than 3 days after ERCP.3 No placebo-controlled study addressing the use of antibiotics in cholangitis after endoscopic drainage has been done, and we generally do not continue antibiotics after successful endoscopic therapy.
Complications
Complications of ERCP include the complications inherent to any endoscopic procedure, including reactions to medications, cardiopulmonary complications, infection, perforation, and hemorrhage, and complications specific to ERCP, such as pancreatitis, postsphincterotomy hemorrhage, and biliary infection. Infectious complications of ERCP are post-ERCP cholangitis and long-term postsphincterotomy cholangitis. The rate of complications related to ERCP is 5% to 8%; risk of complications related to ERCP is 0.3%.4,5
Post–Endoscopic Retrograde Cholangiopancreatography Cholangitis
The risk of cholangitis immediately after ERCP is very low—0.7% in a large series from a single referral center where drainage of obstructed ducts is practiced aggressively.6 The incidence of cholangitis increases 10-fold if diagnostic ERCP is undertaken without performing biliary drainage when an obstruction is found.7 This increased incidence is due to contaminating sterile bile with enteric bacteria, which in the presence of obstruction results in cholangitis. Any obstructed segment of the biliary tract opacified during cholangiography should be drained. Improper disinfection of duodenoscopes or use of contaminated water also increases the risk of post-ERCP cholangitis and bacteremia, especially with Pseudomonas aeruginosa.8,9
Long-Term Postsphincterotomy Cholangitis
Surgical or endoscopic sphincterotomy is a risk factor for bacterial contamination of the biliary tract,10 likely by facilitating transpapillary migration of enteric bacteria. Escherichia coli is the most common organism identified. Analysis of patients after cholecystectomy who underwent sphincterotomy revealed a predisposition for developing brown stones or sludge within the common bile duct (CBD) in association with bacteriobilia.11 However, these data may be biased by predilection in choledocholithiasis prompting sphincterotomy in the first place.
Cholangitis
Bacterial cholangitis results from bile duct obstruction or previous biliary instrumentation. Enterobacteriaceae are the most common causative organisms, and blood cultures are positive in 50% of patients.12 Isolation of enterococci or multiple organisms from bile is more common in patients with a biliary endoprosthesis13 or bilioenteric anastomosis. Charcot’s triad of right upper quadrant pain, fever, and jaundice is present in 70% of patients with acute bacterial cholangitis. The addition of hypotension and confusion constitutes Reynolds’ pentad, which is present in less than 5% of patients with cholangitis but is significantly associated with mortality.14 Right upper quadrant pain and fever may be absent in elderly patients, diabetic patients, or patients treated with systemic corticosteroids.
Anatomy
Postoperative Cholangitis
Patients who have undergone bile duct reconstruction with creation of a hepatojejunostomy are at risk of postoperative cholangitis. This condition is especially prevalent in patients with biliary atresia.15 Bacterial colonization of the hepatojejunostomy and stoma obstruction by food debris may be pathogenic factors.
Sump Syndrome
Sump syndrome occurs after creation of a choledochoduodenostomy to manage retained CBD stones in a dilated bile duct. The distal bile duct between the papilla and the anastomosis becomes a stagnant reservoir or sump into which sludge, calculi, and food can collect. The clinical presentation may include recurrent pain, cholangitis, hepatic abscess, or pancreatitis. Management with endoscopic sphincterotomy with extraction of debris from the bile duct is successful in most patients.16 In case series, recurrence of symptoms has been noted in 0 to 19% and results from stenosis of the sphincter of Oddi.17,18 A repeat sphincterotomy should be considered.18
Preparation
Prophylactic antibiotics are not recommended routinely in patients with biliary obstruction undergoing ERCP for prevention of endocarditis or post-ERCP cholangitis.19,20 However, in patients with cholangitis, broad-spectrum antibiotics providing coverage of gram-negative bacilli and Enterococcus species are indicated until biliary drainage is successfully completed.
Procedure
Intraluminal Obstruction
Biliary Stricture
Outcomes
Treatment of acute cholangitis includes resuscitation, antimicrobials, and biliary tract drainage (Fig. 45.2). Management of respiratory and circulatory insufficiency in a monitored setting and administration of broad-spectrum antibiotics should precede, but not delay, definitive biliary tract decompression in a severely ill or deteriorating patient.
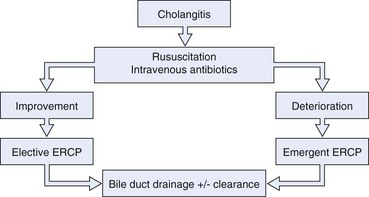
Fig. 45.2 Algorithm for management of cholangitis. ERCP, endoscopic retrograde cholangiopancreatography.
Calculous Cholangitis
Biliary drainage can be accomplished endoscopically, percutaneously, or surgically. Endoscopic treatment, either sphincterotomy with stone extraction21,22 or biliary stent or nasobiliary drain insertion, is superior to surgical treatment in patients with severe cholangitis. Endoscopic sphincterotomy with stone extraction resulted in increased survival compared with surgery in a retrospective cohort of patients with acute calculous cholangitis21; this was despite a higher number of concomitant medical problems and increased age in the patients managed endoscopically. Lai and colleagues23 randomly assigned 82 patients with calculous cholangitis requiring emergent therapy to surgery or ERCP with nasobiliary catheter placement. The mortality in the surgical arm was significantly higher than in the endoscopic arm—32% and 10%. In addition, there were an increased number of nonfatal complications in the group undergoing surgery.
Sphincterotomy and stone extraction is usually attempted during the initial ERCP. However, in critically ill patients with acute cholangitis secondary to choledocholithiasis, it may be prudent to achieve biliary drainage endoscopically, by insertion of a stent or nasobiliary catheter, and defer stone extraction to a later time. Therapeutic response, procedure-related complications, and length of procedure are similar for biliary stents and nasobiliary catheters, but inadvertent catheter removal and patient discomfort are greater in patients who receive a nasobiliary catheter.24 Approximately 10% of patients have cholangitis owing to stones that cannot be removed by standard means, including mechanical lithotripsy. These stones include large stones, stones located proximal to a stricture, or stones greater than the diameter of the distal bile duct. Options are endoscopic EHL, extracorporeal shock wave lithotripsy, endoscopic laser lithotripsy, and permanent biliary stent placement.25–27 Increasingly, the use of adjunctive biliary balloon sphincteroplasty is being used to remove CBD stones safely and effectively. An occlusion cholangiogram at completion of ERCP may ensure clearance but carries a significant risk of bacteremia in this situation.
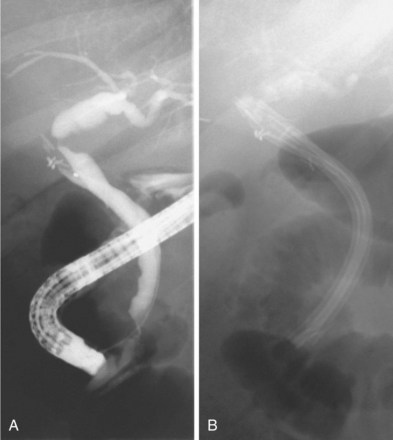
If all stones or stone fragments cannot be removed during the initial endoscopic session, a stent should be left in place to provide bile drainage and prevent further cholangitis (Fig. 45.3). Long-term stent therapy is no longer advisable because of the high incidence of cholangitis and related deaths.28,29 Similar techniques can be employed in the cystic duct to treat Mirizzi’s syndrome.26,30,31 In a patient with cholangitis and gallstones but no evidence of choledocholithiasis on cholangiography, empiric endoscopic sphincterotomy does not appear to decrease the risk of subsequent episodes of cholangitis and results in a higher ERCP complication rate.32
Cholangitis Secondary to a Biliary Stricture
Biliary tract obstruction secondary to a malignant stricture rarely causes cholangitis, unless the bile has been contaminated with bacteria during a previous biliary intervention. Patients with strictures involving the biliary hilum should undergo stent placement into the right and the left hepatic ducts when technically possible because bilateral decompression would improve patient survival.33 This is especially important if the biliary tract proximal to the stricture has filled with contrast material.
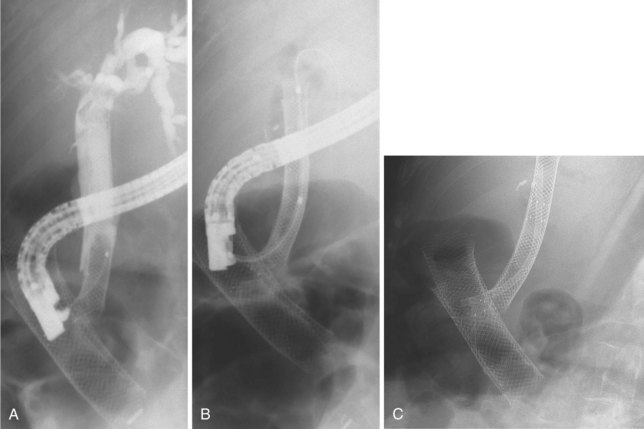
Cholangitis Secondary to Stent Occlusion
Plastic biliary stents develop a bacterial biofilm on their surface,34 which leads to stent occlusion and risk of cholangitis. Uncovered self-expandable metal stents, by virtue of their larger diameter and composition, do not develop encrustation at the same rate and have a longer patency.34 If metal stent obstruction does occur, it is usually the result of tumor ingrowth between the metal struts or tumor overgrowth at either end. Metal stents covered with a synthetic coating to prevent tumor ingrowth seem to have a similar or increased duration of patency (Fig. 45.4).35
Recurrent Pyogenic Cholangitis
Recurrent pyogenic cholangitis, also known as Oriental cholangiohepatitis, is a clinical syndrome comprising repetitive episodes of bacterial cholangitis resulting from intrahepatic biliary obstruction with calcium bilirubinate stones or strictures or both. The bile ducts in the left lateral segment of the liver are often the only ducts affected or the most severely affected. This segment may be anatomically predisposed to stasis because of duct angulations slowing bile drainage. Chronic obstruction eventually causes permanent dilation of the proximal biliary tract, often filled with intrahepatic stones. Bile stasis and bacterial contamination may result in the development of multiple hepatic abscesses. Enterobacteriaceae bacteria are the most frequent organisms cultured from bile. P. aeruginosa may be seen in patients who have previously undergone endoscopic or surgical biliary intervention. Anaerobes are less common. Growth of multiple organisms, although unusual in other causes of cholangitis, often occurs in recurrent pyogenic cholangitis.36 Isolation of biliary parasites in patients with recurrent pyogenic cholangitis is common,37,38 but it is unclear whether the parasite is an etiologic agent or an incidental finding.
Preparation
Prophylactic antibiotics have been recommended to decrease the risk of cholangitis during ERCP in patients with recurrent pyogenic cholangitis.39 Magnetic resonance (MR) cholangiography before ERCP should be considered. The major advantage of MR cholangiography is complete visualization of the biliary tract including segments obstructed by calculi or strictures40 that may not be apparent by ERCP. Detailed knowledge of intrahepatic segment anatomy is necessary to correlate MR imaging to the opacified ducts at ERCP and guide endoscopic management.
Procedure
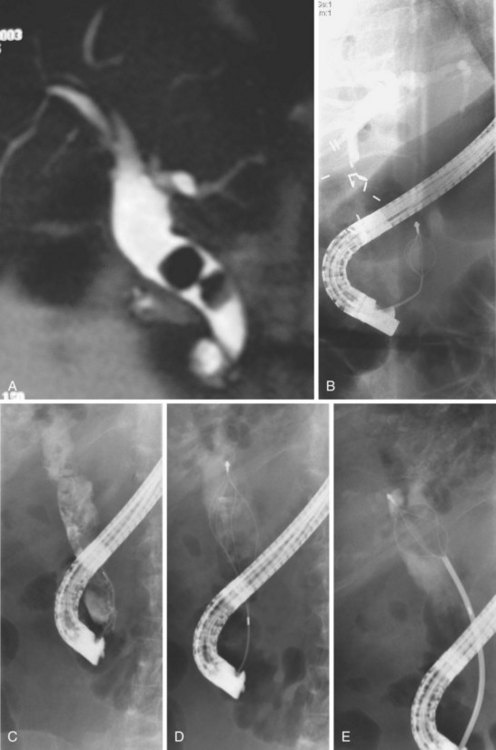
Cholangiography during ERCP also accurately documents duct dilation, intraductal stones, and gallstones (Fig. 45.5). The intrahepatic ducts appear straightened and acutely angulated at branches, likely secondary to periductal fibrosis. There is often distinct tapering of the intrahepatic ducts proximally, described as the “arrowhead” sign, and decreased duct branching. Complete occlusion of an intrahepatic duct by a stone may be represented by segmental absence of contrast material and is better assessed by MR cholangiography.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree