The conditions indicated for endoscopic en bloc resection are as follows:
1. Lesions for which en bloc resection with snare EMR is difficult to apply
∙ LST-NG, particularly LST-NG (PD)
∙ Lesions exhibiting a VI-type pit pattern
∙ Cancers with mild submucosal invasion
∙ Large depressed-type tumors
∙ Large malignant protruded-type lesionsa
2. Mucosal tumors with submucosal fibrosisb
3. Sporadic localized tumors that occur due to chronic inflammation
4. Local residual early cancers after endoscopic resection
Indications for Colorectal ESD at Japanese National Cancer Center Hospital (Table 3.2)
Table 3.2
Indications for Colorectal ESD at the Japanese National Cancer Center Hospital
Based on previous clinicopathological analyses of laterally spreading tumors (LSTs) [7, 8], LST non-granular type (LST-NG) lesions (Fig. 3.1) have a higher rate of SM invasion, which can be difficult to predict endoscopically. Approximately 30–56 % [9] of LST-NGs have multifocal SM invasion, which is primarily SM superficial (T1a). This is especially difficult to predict before endoscopic treatment. In addition, LST-NGs >20 mm in diameter are quite difficult to resect en bloc by conventional EMR; therefore, these tumors are definite candidates for ESD (Fig. 3.1).
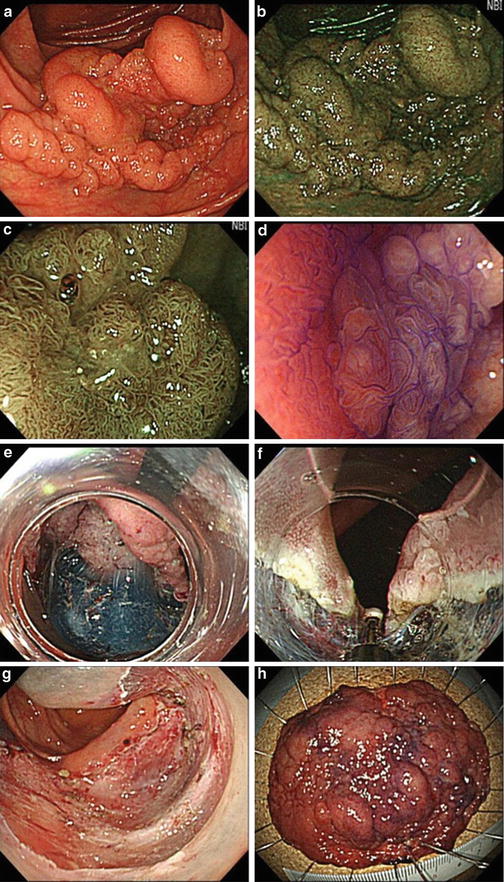
Fig. 3.1
(a) A 3/4 circumferential LST-NG was located in the transverse colon. Prominent fold convergences were observed and submucosal invasion was suspected. (b) Narrow band imaging (NBI) revealed the margin of this tumor clearly. (c) A 0.4 % indigo carmine dye was sprayed on this LST-NG, clearly delineating the margin. (d) A 0.05 % crystal violet staining was conducted and the IIIs pit pattern was observed on this tumor’s surface, despite its large size and prominent fold convergences. A magnified colonoscopic diagnosis was IIIs (non-invasive) pit pattern and this lesion was diagnosed as intramucosal cancer. (e) ESD was started in retroflex position with a pediatric-type colonoscope equipped with a short-type hood. (f) An IT-nano knife was used for submucosal dissection. (g) Successful en bloc resection was achieved in 140 min without any complication. (h) Histopathology revealed a well-differentiated adenocarcinoma with intramucosal depth of invasion, so curative R0 resection was achieved
In contrast, LST granular type (LST-G) lesions have a lower rate of SM invasion, which is generally found under the largest nodule or depression. These lesions are easier to predict endoscopically [7, 8]. LST-Gs >20 mm can be treated by elective piecemeal EMR [7] rather than ESD. The area containing the largest nodule should be resected before the rest of the tumor. LST-Gs >30 mm are possible candidates for ESD since such lesions are more difficult to treat by piecemeal EMR (Fig. 3.2). A high SM invasion rate and 25 % rate of multifocal invasion were recently reported [9, 10], compared to other recent series [11, 12].