CHAPTER 120 Ileus and Pseudo-obstruction
The functions of the small intestine and colon are regulated through the integrated activities of intestinal smooth muscle, the interstitial cells of Cajal (ICC), intrinsic and extrinsic nerves, neurohumoral peptides, and gastrointestinal hormones (see Chapters 97 and 98). Neurons located in the intestine wall constitute the intrinsic neural network known as the enteric nervous system (ENS) (Fig. 120-1). The extrinsic network consists of visceral sensory afferents in the vagus, thoracic, and pelvic splanchnic nerves (Fig. 120-2) and visceral motor efferents of the autonomic nervous system. These extrinsic neurons synapse with the ENS and connect it to the central nervous system.
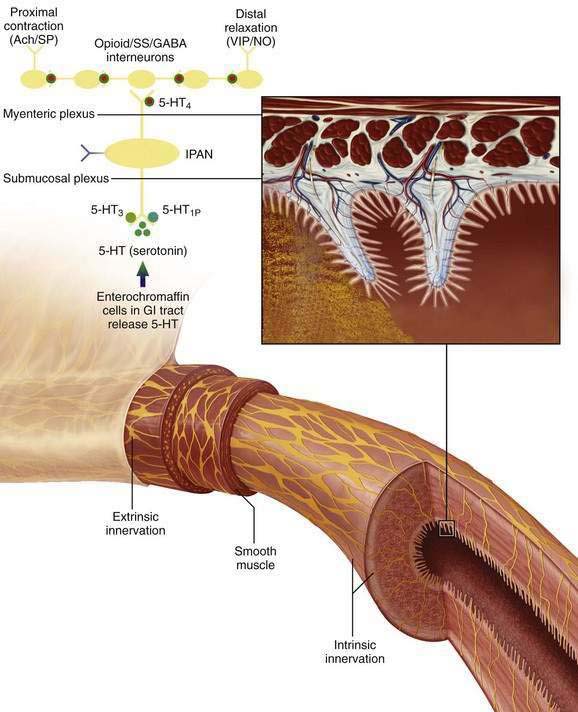
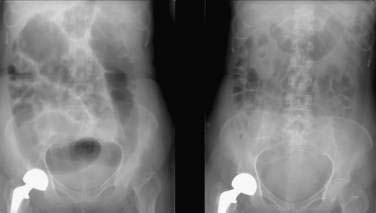
Figure 120-1. Intrinsic pathways that govern intestinal motility. The enteric nervous system (ENS) includes intrinsic motor neurons (efferent), extrinsic motor neurons (efferent), interneurons, and sensory neurons, which together make the ENS capable of carrying reflexes and acting as a center of integration in the absence of input from the central nervous system. Ach, acetylcholine; CGRP, calcitonin gene-related peptide; GABA, γ-aminobutyric acid; GI, gastrointestinal; 5-HT, serotonin; 5-HT1P, serotonin 1p isotype; 5-HT3, serotonin 3 isotype; 5-HT4, serotonin 4 isotype; IPAN, intrinsic primary afferent neuron; NO, nitric oxide; PACAP, pituitary adenylate cyclase-activating peptide; SP, substance P; SS, somatostatin; VIP, vasoactive intestinal peptide. (See text and Chapters 97 and 98.)
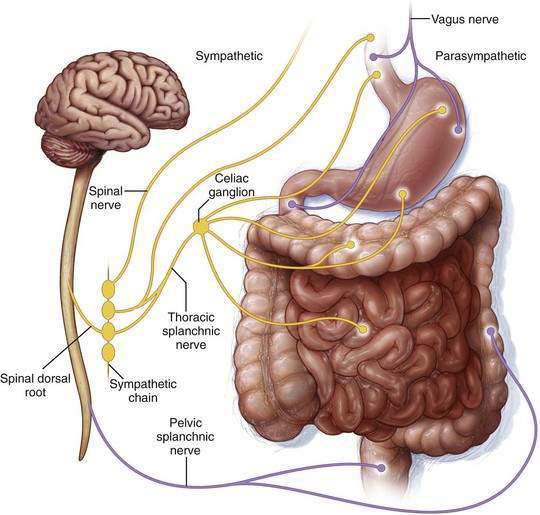
Figure 120-2. Extrinsic pathways governing intestinal motility. Enteric control is modulated by the parasympathetic and sympathetic nerves of the autonomic nervous system, which respectively stimulate and inhibit nonsphincteric muscle. (See text and Chapters 97 and 98.)
EPIDEMIOLOGY
The prevalence of intestinal dysmotility varies according to the underlying pathology and pathophysiology. Postoperative ileus is an unavoidable adverse response to abdominal or retroperitoneal surgery that accounts for delayed refeeding, prolonged hospitalization, and increased costs. It is the main determinant of length of hospital stay after uncomplicated abdominal surgery.1 The economic impact of postoperative ileus in the United States is estimated to be more than $7.5 billion annually, not including lost work expense. Acute colonic pseudo-obstruction is estimated to occur in 0.1% of surgical patients, 0.05% of patients admitted for trauma,2,3 and 0.3% of critically ill patients with burn injury.4 More than 95% of patients with acute colonic pseudo-obstruction have factors that predispose them to develop the condition,3 including nonsurgical trauma, pelvic or hip surgery, cardiovascular disease, or infection.5 Spontaneous perforation rates in this condition range from 3% to 15%, with an associated 50% mortality rate.
Most cases of chronic pseudo-obstruction result from primary acquired defects in nerves, ICC, and smooth muscle cells, or they are secondary to metabolic disorders, inflammation, infiltrating disease, autoimmune conditions, or cancer, namely paraneoplastic chronic pseudo-obstruction.6,7 Of the developmental neuropathies, the prototypical congenital dysmotility disorder, Hirschsprung’s disease, occurs in one in 5000 live births (see Chapter 96). The literature documents several heritable degenerative smooth muscle disorders—familial visceral myopathies (FVMs) and childhood visceral myopathies (CVMs)—and inherited degenerative disorders of the myenteric plexus (familial visceral neuropathies [FVNs]) that are rarely encountered, even in tertiary centers. A small number of families, mostly whites and less often African Americans8 and Latin Americans,9 has been documented with these conditions.
NEURAL CONTROL OF SMALL BOWEL AND COLONIC MOTILITY
The enteric nervous system (ENS) consists of extensive ganglionated plexuses located in the muscular wall of the gastrointestinal tract10; functionally most important are the myenteric and submucosal plexuses (see Fig. 120-1). In association with the muscle layers, the networks of ICC are recognized as pacemakers that activate neuromuscular function. The ENS consists of approximately 100 million neurons in higher mammals, roughly equal to the number of neurons in the spinal cord. Histologic and physiologic studies11–13 of the intestinal tract have characterized the properties of the neurons and transmitters mediating its functions, including the peristaltic reflex, and the neuroimmune interactions between neurons and inflammatory cells.
Precursor cells arise from three axial levels of the neural crest: vagal, rostral-truncal, and lumbosacral14 levels. The enteric neurons mainly arise from the vagal neural crest of the developing hindbrain and colonize the bowel by migration in a rostrocaudal direction. Vagal crest cells are not restricted to a particular intestinal region. Some enteric neurons arrive in the hindgut from the lumbosacral level via a caudorostral wave of colonization. Rarely, these migrating cells do not reach the entire bowel; usually this affects the terminal portion of the colon, as in the classical forms of Hirschsprung’s disease.15
Neural control of the intestines is covered in Chapters 97 and 98.
ILEUS
Ileus refers to the inhibition of propulsive intestinal motor activity in the absence of a mechanical obstruction. Abdominal or retroperitoneal surgery is the most common cause of ileus, which develops in essentially all such cases16 and is the focus of this section. Other causes of ileus are listed in Table 120-1 and include general anesthesia, medications, inflammation, infection, ischemia, and various metabolic and neurologic processes.
Table 120-1 Factors That Contribute to Ileus
| Infection |
| Inflammation |
| Metabolic |
| Neurohumoral |
| Pharmacologic |
| Surgery |
| Miscellaneous |
The autonomic nervous system plays a key role in regulating gastrointestinal motility.17 Parasympathetic nerve activity stimulates intestinal motility by inducing the release of acetylcholine from excitatory neurons in the myenteric plexus. Sympathetic nerve activity inhibits activity by blocking the release of acetylcholine from the same excitatory fibers while also providing the efferent limb of multiple reflex pathways. Sympathetic neural input appears to be the main physiologic mechanism involved with impaired intestinal motility in the postoperative period. Afferent neural input caused by irritation (incision) or inflammation of the peritoneum results in an increase in inhibitory sympathetic efferent neural activity via the splanchnic nerves and an overall decrease in bowel activity.18 Sympathetic blockade does not entirely prevent the delayed intestinal motility induced by abdominal surgery, and so alternate mechanisms such as nonadrenergic, noncholinergic (NANC) nerves are believed to contribute to peripheral autonomic neuroeffector transmission and to influence postoperative ileus.19
Uncomplicated postoperative ileus resolves in a predictable fashion. The small intestine resumes activity within 24 hours, the stomach in 24 to 48 hours, and the colon generally within 72 hours.20,21 Ileus is an important cause of prolonged hospitalization and escalating costs associated with surgery.1 Determining when ileus has resolved depends on the endpoint chosen, and all endpoints have relative weaknesses. Return of bowel sounds requires frequent examination, and their presence does not ensure propulsive activity.21 Passage of flatus requires verbal feedback and a willingness of the patient to report such activity. Bowel movements may be the most reliable end point, but they represent distal bowel activity rather than global gastrointestinal function. Resolution of postoperative ileus is complete when oral intake is tolerated without pain, bloating, or emesis.
PATHOPHYSIOLOGY
The pathophysiology of postoperative ileus involves several mechanisms including disruption in autonomic neural pathways, release of neurohumoral stress mediators, intestinal inflammatory response, perioperative fluid excess, and various pharmacologic elements.19,22,23
Disrupted Neural Pathways
Parasympathetic (vagal) neural input stimulates intestinal motor activity, whereas sympathetic (splanchnic) input is inhibitory. Sympathetic activity is the predominant inhibitory influence on intestinal motility and provides the efferent limb of multiple reflex pathways. Sympathetic stimulation is a key factor in the development of postoperative ileus. Local stimuli trigger an inhibitory reflex that results in intestinal dilatation, for which the somatic and splanchnic nerves provide both the afferent and efferent pathways.24 Local stimuli include incising the abdominal wall and handling of the intestine; blocking sympathetic stimuli during surgery does not fully prevent such inhibition of intestinal motility.
NANC neurotransmitters also play a role in postoperative ileus. Nitric oxide (NO) may be the predominant NANC neurotransmitter that mediates the inhibitory influence of ENS neurons on smooth muscle. Other NANC neurotransmitters, including vasoactive intestinal peptide (VIP) and neuropeptide Y act through inhibitory pathways similar to the NO pathway to relax intestinal smooth muscle; substance P and adenosine triphosphate (ATP) act through excitatory motor pathways to influence postoperative ileus.25,26 NO inhibitors, and VIP and substance P antagonists decrease postoperative ileus in animal studies, but the potential usefulness of these agents in humans is unclear.18,25
Release of Neurohumoral Stress Mediators
Surgical stress and circulating inflammatory mediators activate pathways that trigger release of hypothalamic corticotrophin-releasing factor (CRF).27 CRF modulates feeding behavior under stressful conditions—explaining why anorexia is a common reaction to stress—and is considered essential in orchestrating the stress response.28 Experimental studies have shown that administration of CRF or CRF-related peptides delays gastric emptying and inhibits gastric motility29,30 similar to postoperative gastric ileus, whereas administration of the CRF1 antagonist, CP-154,526, blocks surgery-induced delay in gastric emptying.19
Abdominal surgery also stimulates capsaicin-sensitive afferent fibers, activating the inhibitory efferent pathways that disrupt coordinated intestinal motility.31 These fibers have been shown to play a crucial role in acute gastroprotection. Release of neurotransmitters such as calcitonin gene-related peptide (CGRP) and the related increase in mucosal blood flow have been identified as key factors in the protective effect of the stimulation of these fibers by capsaicin.32 Capsaicin-sensitive afferent nerves can influence ulcer healing by mediating the hyperemic response through the release of CGRP and facilitating acid disposal in the mucosa.32 Studies are ongoing to determine mechanisms of CRF activity and other stress mediators in the inhibition of gastrointestinal motility.
Intestinal Inflammation
Handling the intestine during surgery results in a marked inflammatory reaction,33–35 leading to induction of inducible nitric oxide synthase (iNOS) and cyclooxygenase (COX)-2 and the release of mast cells, monocytes, and neutrophils within the muscularis propria, but not the mucosa. Bowel handling also leads to secretion of numerous proinflammatory cytokines including interleukin (IL)-1β, IL-6, tumor necrosis factor (TNF)-α, and monocyte chemotactic protein (MCP)-1 and up-regulates intercellular adhesion molecule (ICAM)-1.36 Thus, extensive manipulation of the intestine or exposure of the peritoneum to irritants (e.g., pus or blood) increases the probability of developing postoperative ileus. The effect on intestinal transit appears to be proportional to the magnitude of the inflammatory response.37
In addition to autonomic signaling pathways, extrinsic noradrenergic nerves contribute to the regulation of various digestive functions, including intestinal propulsion, mucosal secretions, and bowel sensation, through activation of α2-adrenoceptors. In the presence of intestinal inflammation, enteric α2-adrenoceptors are up-regulated, giving enhanced inhibitory control of cholinergic and noradrenergic transmission.38,39 Located on neurons and inflammatory cells, α2-adrenoreceptors may be important in the pathogenesis of postoperative ileus, because their location provides a link between the inflammation induced by intestinal handling and activation of neuronal pathways.40
Perioperative Fluid Excesses
Intravenous fluid overload during or after surgery delays recovery of gastrointestinal function41 and is associated with poor survival and complications.42 In patients undergoing colon resection, use of perioperative and postoperative restricted fluid regimens has resulted in reduced hospital stays, faster return of gastrointestinal function, and fewer postoperative complications including reduced nausea and vomiting compared with higher-volume strategies.43
Pharmacologic Mechanisms
Anesthesia
All anesthetic agents have an inhibitory effect on intestinal motility, although the technique of administration can significantly influence the duration of postoperative ileus.44 Mid-thoracic (T6-T9) epidural anesthesia often is used as an adjunct to general anesthesia in abdominal operations. The technique allows local placement of the anesthetic for sympathectomy, which substantially reduces the severity and incidence of postoperative ileus44 and theoretically blocks afferent and efferent inhibitory reflexes associated with abdominal surgery.19,45 Local epidural anesthesia appears to increase splanchnic blood flow to the intestine, disrupt afferent inhibitory effects, and further reduce sympathetic neural input.18,46,47 Use of systemic opioid therapy or epidural opioids, regardless of whether administered by a low-thoracic or a low-lumbar route, does not shorten the duration of ileus compared with nonopioid epidural anesthetics.48,49
Opiates
Endogenous and exogenous opiates contribute significantly to the development of postoperative ileus.50,51 Of the three main classes of opiate receptors (µ, κ, δ) located in the central nervous system (CNS) and gastrointestinal tract,52 the CNS µ receptors mostly modulate analgesia within the brain and the spinal cord. Endogenous opioids released from neurons within the submucosal and myenteric plexus of the gastrointestinal tract modulate sphincteric and peristaltic activity in a coordinated fashion.53 Activation of intestinal µ receptors suppresses release of acetylcholine from cholinergic neurons, resulting in delayed intestinal motility.54
Exogenous opioids increase antral and proximal duodenal tone with an overall inhibitory effect on motility. The effect of morphine on the small intestine is biphasic, initially stimulating MMC activity followed by atony, which impedes propulsion and delays intestinal transit.55 In the colon, morphine increases the tone and amplitude of nonpropagating contractions, thus reducing propulsive activity and slowing transit. The overall effect of opiates is to decrease intestinal motility.
CLINICAL FEATURES
Factors that contribute to the development of ileus are listed in Table 120-1. Plain abdominal films can show air-filled stomach or distended loops of intestine or colon. Abdominal computed tomography (CT) can confirm the diagnosis while delineating extraluminal findings including abscess, retroperitoneal hematoma, pancreatitis, ascites, and inflammation, which might contribute to nonmechanical obstruction.
TREATMENT
Standard
Bowel rest neither shortens the time to first bowel movement nor decreases the time to oral intake. Large meals can induce nausea and bloating, but small meals can stimulate gastrointestinal motility and reduce the duration of postoperative ileus.56,57 Nasogastric tube decompression, once considered standard of care, is not recommended in routine abdominal operations because it does not hasten recovery from ileus.58,59 In fact, routine use of nasogastric decompression has been associated with a higher postoperative complication rate of atelectasis and aspiration pneumonia and prolonged hospitalization. Early mobilization after surgery is recommended to reduce complications of atelectasis, pneumonia, and deep venous thrombosis; however, there is little evidence that ambulation hastens resolution of ileus.60
Preventive
Operative Period
Nature of Surgery
When compared with open surgical procedures, laparoscopy decreases the duration of postoperative ileus.61 Theoretically, reducing the mechanisms known to cause postoperative ileus (see earlier) by making small incisions and minimizing tissue handling should improve surgical outcome. Circulating levels of cytokines (e.g., IL-1β and IL-6) and C-reactive protein are significantly lower after laparoscopy than after open abdominal procedures and may reflect reduced tissue injury.62 Return to a normal interdigestive pattern occurs 40% faster after laparoscopic colectomy compared with conventional colectomy, and time to first bowel movement is reduced 27%.63 Also, tolerance of oral feedings and improved transit occur earlier after laparoscopic resection.64
Anesthesia
Epidural anesthesia, but not general anesthesia, interrupts sympathetic outflow, blocking afferent and efferent mechanisms that trigger inhibitory reflexes and the CRF-mediated stress response that can restore metabolic activities and reduce postoperative morbidity.65 A significant reduction in the duration of ileus occurs in patients who receive epidural bupivacaine compared with those receiving epidural opioid.66–68 Epidural bupivacaine alone was superior to epidural bupivacaine combined with opioid in reducing the duration of ileus without compromising pain relief. Delivery of local anesthetic via a mid-thoracic (T6-T9) epidural catheter for abdominal surgery significantly reduces duration of ileus and hospitalization,18 whereas low thoracic and lumbar epidural deliveries do not show similar benefit.46,47 Local anesthesia may be more important in reducing postoperative ileus when used as an adjunct to open abdominal surgery rather than to laparoscopic surgery.69 The optimal duration of epidural anesthetic appears to be two to three days beyond the operation.70 Epidural anesthesia might not be necessary in laparoscopic colorectal surgery and, in some cases, it may be replaced by opioid-sparing multimodal analgesia, including oral acetaminophen, NSAIDs, systemic local anesthetics, or continuous infusion of the wound with local anesthetic.71,72
Perioperative Fluid Management
Several large trials have shown that excessive hydration in the perioperative period increases morbidity. Fluid excess, which can cause bowel edema42 and pulmonary compromise, is linked to prolonged postoperative ileus and extended hospital stay.73 Fluid management by perioperative optimization of hemodynamic function, known as goal-directed therapy, maximizes cardiac stroke volume by using small fluid challenges43,74 and has been shown to improve patient outcome. Avoiding fluid overload by using goal-directed therapy can reduce postoperative complications and facilitate rapid functional gastrointestinal recovery.43
Postoperative Period
Postoperative nausea and vomiting (PONV) occurs in 20% to 30% of low-risk surgical patients and in up to 80% of high-risk surgical patients.75 General anesthesia increases the risk of PONV nine-fold greater than the use of regional anesthesia.76 Reducing risk factors (Table 120-2) when possible and using prophylactic agents in patients at high risk for PONV can shorten the duration of ileus; low-risk patients are less likely to receive benefit. Dexamethasone, droperidol, and the 5-HT3 antagonist ondansetron, alone or in combination, can provide effective antiemetic prophylaxis against PONV77 in high-risk patients. Aprepitant is a substance P antagonist that acts on the neurokinin 1 receptor and is FDA approved for prevention of PONV.
Table 120-2 Risk Factors for Postoperative Nausea and Vomiting
| Anesthesia |
| Patient |
| Surgery |
Modified from Gan TJ, Meyer TA, Apfel CC, et al. Society for Ambulatory Anesthesia guidelines for the management of postoperative nausea and vomiting. Anesth Analg 2007; 105(6):1615-28.
Chewing Gum
Several studies show gum chewing in the postoperative period significantly reduces the time to first flatus and the time to first passage of feces compared with standard treatment alone,78,79 although the length of hospital stay is only marginally reduced. Chewing gum does not increase complications or readmissions and is a low-risk, inexpensive, first-line approach to resolving ileus after colorectal surgery.80
Early Oral Intake
Several randomized, controlled trials support early postoperative feeding (within 24 hours) in patients undergoing gastrointestinal surgery.81 Although early postoperative feeding can increase vomiting, mortality is reduced with a trend toward reduction of risk of postsurgical complications and shorter hospitalization. Early oral nutrition attenuates catabolism and reduces intestinal permeability that can lessen infectious complications.82,83 Despite ongoing controversy, studies suggest early postoperative feeding may be of benefit.
Drug Therapy
Opioid-Sparing Analgesia
Ketorolac tromethamine is an NSAID that can be administered parenterally, thereby circumventing the time lag accompanying postoperative oral intake. Ketorolac is equivalent to morphine in analgesic effect after major abdominal surgery without the functional gastrointestinal side effects of morphine.84 Ketorolac has anti-inflammatory and antipyretic activity and reduces postoperative ileus and morphine requirements.85
Continuous epidural infusion of lidocaine86 after colonic resection can reduce morphine use, improve pain relief, and hasten recovery. Ketamine, gabapentin, pregabalin, and neural blockade are recognized opioid-sparing agents or techniques with the potential to accelerate postoperative recovery; additional study is required because results of their effects are inconsistent.87 In addition, use of postoperative patient-controlled analgesia (PCA) that allows on-demand intravenous delivery may be as effective as continued epidural administration and can reduce medication dose and duration.88
Opioid Antagonists
Stimulation of µ-opioid receptors in the brain and intestine by morphine and other opioids imparts a potent central analgesic effect plus dose-limiting debilitating constipation and other unwelcome side effects.51 Therefore, effective blockade of peripheral opioid receptors in the gastrointestinal tract should manage opioid-related bowel dysfunction. Alvimopan and methylnaltrexone are selective µ-opioid antagonists with activity that is restricted to the peripheral receptors.
Alvimopan (12 mg, orally two hours before surgery, then twice daily for seven days) shortened the time to gastrointestinal recovery (passage of flatus, tolerance of solid food, first evacuation) by 15 to 18 hours and the hospital stay by one day following bowel resection.89 The effects of alvimopan are achieved without adverse effects on abdominal pain scores or patient-administered analgesia.89–92 The alvimopan studies used general (not epidural) anesthesia and nasogastric tubes up to 24 hours postoperatively; oral feeding was initiated at 48 hours postoperatively. Avoiding known risk factors and implementing measures to prevent postoperative ileus as it occurs in fast-track postoperative surgery can alter outcome.
Methylnaltrexone has been shown to reverse morphine-induced delay in gastric and orocecal transit time in healthy subjects.93 In patients with opioid-induced constipation with advanced illness, methylnaltrexone induced laxation and reduced symptoms of constipation.93
Prokinetic Agents
There are no available effective prokinetic agents for the treatment of postoperative ileus. Cisapride is a serotonin agonist that facilitates acetylcholine release from the intrinsic neural plexus with inconsistent effect on resolution of postoperative ileus. Cisapride was removed from the market because of potentially dangerous cardiac side effects, but it is available under a limited-access program through Janssen Pharmaceutica.94 Neostigmine and lidocaine require additional studies with clinically relevant outcomes to prove treatment effectiveness.92 Erythromycin has demonstrated a consistent absence of effect in hastening postoperative recovery in several prospective randomized clinical trials. Metoclopramide, a mixed cholinergic agonist and dopamine antagonist, shows only small or insignificant benefit in the treatment of postoperative ileus.92
Laxatives
There is some evidence to support the use of laxatives in the postoperative period. Osmotic and stimulant (suppository) laxatives appear safe and beneficial in producing early bowel evacuation and might shorten the duration of postoperative ileus. Small trials have examined the effect of bisacodyl suppository alone,95 bisacodyl in combination with milk of magnesia,96 and magnesium oxide combined with disodium phosphate,97 the latter used in a fast-track rehabilitation protocol following abdominal hysterectomy. No significant adverse events have been reported with any agent. High-quality prospective trials are needed.
Emerging Drugs
Lubiprostone, a chloride-2 channel activator that stimulates intestinal fluid secretion and increases intestinal transit, is under investigation as an agent to treat postoperative ileus. Other drugs emerging from trials or preclinical testing as potential agents for the treatment of postoperative ileus include linaclotide (a guanylate cyclase-C agonist), motilin agonists (KOS-2187, GM-611, GSK-326416), a neurokinin-2 receptor antagonist (MEN-11420), and growth hormone secretagogues (ipamorelin, TZP-101).31
Multimodal Approach to Preventing Postoperative Ileus
The advent of laparoscopic surgery, opioid-sparing analgesics, regional anesthesia, and other factors that hasten recovery from postoperative ileus (Table 120-3) has led to improved care of patients undergoing abdominal surgery. First described in the 1990s, enhanced recovery management strategies—fast-track surgery methods—combine treatment modalities that individually improve outcome following major surgery.98 An overarching goal of fast-track surgery is to lower rates of organ dysfunction, thereby reducing morbidity, hastening recovery, and shortening hospital stay.69 Some benefits of fast-track surgery are listed in Table 120-4. The concept has proved valid across all surgical specialties, but the most physiologic data are available for colonic surgery. Fast-track surgery has been shown to enhance recovery from postoperative ileus: More than 90% of patients have a normal oral intake, defecate within 48 hours, and have a hospital stay of two to four days (reduced from five to 10 days) after uncomplicated open colonic surgery.71,99,100
Table 120-3 Factors That Contribute to Enhanced or Delayed Recovery from Postoperative Ileus
| FACTOR | RANDOMIZED CONTROLLED STUDIES (RCTs)* |
| Enhances Recovery | |
| Chewing gum | x |
| Early oral feeding† | |
| Goal-directed fluid therapy and avoidance of fluid overload | x |
| Intravenous or wound (local) anesthetics | x |
| Laparoscopic vs. open surgery|| | x |
| Laxatives† | |
| Length and/or type of incision‡ | |
| Mobilization‡ | |
| Peripheral opioid antagonists | x |
| PONV antiemetic agents | x |
| Thoracic epidural local anesthetics | x |
| Delays Recovery | |
| Administration of excess perioperative fluid | x |
| Nasogastric tubes | x |
| Opioids | x |
| Restrictions on oral intake† | |
PONV, postoperative nausea and vomiting.
* Based on two or more RCTs or meta-analyses.
† Preliminary studies are positive, but further studies are required before general recommendations are made.
‡ Data are limited or inconclusive.
|| Data are difficult to interpret because of the use of nasogastric tubes, use of opioid analgesia, and restrictions for oral intake in “open” groups.
Used with permission and adapted from Kehlet H. Postoperative ileus—an update on preventive techniques. Nat Clin Pract Gastroenterol Hepatol 2008; 5(10):552-558.
Table 120-4 Benefits of Fast-Track* Surgery
* Fast track refers to the use of enhanced recovery management strategies to improve outcomes after surgery.
ACUTE COLONIC PSEUDO-OBSTRUCTION
Acute colonic pseudo-obstruction, also known as Ogilvie’s syndrome,101 is characterized by acute massive colon dilatation involving primarily the right side of the colon and without a mechanical cause. It is most often diagnosed in hospitalized, debilitated medical or surgical patients with a wide array of medical conditions (Table 120-5). Ogilvie’s syndrome is estimated to occur in 0.1% of all surgical patients,3 and patient outcome depends on the severity of the underlying illness, the person’s age, the maximum diameter of the cecum, the delay until colonic decompression, and the presence of colonic ischemia.
Table 120-5 Conditions Commonly Associated with Acute Colonic Pseudo-obstruction
| Cardiovascular |
| Drugs |
| Inflammation |
| Metabolic |
| Neoplasia |
| Neurologic |
| Post-surgical |
| Post-traumatic |
| Respiratory |
Used with permission from De Giorgio R, Stanghellini V, Barbara G, et al. Prokinetics in the treatment of acute intestinal pseudo-obstruction. IDrugs 2004; 7(2):160-165.
PATHOPHYSIOLOGY
Disrupted autonomic nervous system activity is considered a key factor in the pathogenesis of acute colonic pseudo-obstruction. Parasympathetic (excitatory, causing contraction) innervation of the colon is from the vagus nerve, which supplies the right colon and extends to the splenic flexure; parasympathetic innervation of the distal colon and rectum is from the spinal supply sacral plexus. Sympathetic (inhibitory, causing relaxation) innervation of the colon is from the celiac and mesenteric ganglia (see Fig. 120-2). The current proposed mechanisms of acute colonic pseudo-obstruction are summarized in Table 120-6.
Table 120-6 Proposed Mechanisms for Acute Colonic Pseudo-obstruction
| Intestine Fails to Contract |
| Intestine Fails to Relax |
Modified from Delgado-Aros S, Camilleri M. Pseudo-obstruction in the critically ill. In: Scholmerich J, editor. Bailliere’s best practice & research in clinical gastroenterology: gastrointestinal Disorders in the Critically Ill, vol. 17. London: Elsevier Science; 2003. pp. 427-44.
Local stimuli effect an inhibitory reflex that results in dilatation of the colon, for which the splanchnic nerves provide both the afferent and efferent pathways. Local stimuli, including peritoneal inflammation, infection, and handling of the colon, result in the release of mast cells, leukocytes, and monocytes.33–35 Inflammatory mediators such as ICAM-1, MCP-1, iNOS, and COX-2 are up-regulated during the first 18 hours after abdominal surgery, and the degree of postoperative intestinal impairment correlates with the intestinal inflammatory response.
The release of endogenous opioids after surgery has been related to the inflammation and impaired motor activity that characterize the physiologic response to surgery. Administration of antidepressant, phenothiazine, anti-parkinsonian, or narcotic medications can induce acute colonic pseudo-obstruction.102 Opioids inhibit release of NO from inhibitory motor neurons in vitro and delay transit in vivo.
CLINICAL FEATURES
Acute colonic pseudo-obstruction typically occurs in older (mean age, 60 years) men who are hospitalized or institutionalized (60%) with severe underlying medical or surgical conditions (see Table 120-5).
Symptoms and Signs
The most characteristic feature of acute colonic pseudo-obstruction is abdominal distention, which can develop gradually over three to seven days or more acutely within 24 hours. About 60% of patients experience nausea and vomiting. Abdominal pain (80%) tends to be mild and constant, with occasional slight rebound tenderness and painless distention.103 Low-grade fever may be present. Disturbances of electrolyte levels occur, notably hypokalemia, hypocalcemia, hyponatremia, and hypomagnesemia. New abdominal pain or tenderness, increasing fever, and increasing white blood cell count are features of ischemia or perforation. About 90% of patients have abnormal bowel sounds, which vary from absent to hyperactive. In many cases, the abnormal bowel sounds are high-pitched and suggest mechanical obstruction.2
Radiology
The most distinctive feature of acute colonic pseudo-obstruction on a plain abdominal film is dilatation of the colon that preferentially affects the right side of the colon. The maximal diameter of the cecum typically ranges from nine to 25 cm, often with a cutoff sign at the hepatic or splenic flexure (Fig. 120-3). The left colon, including the rectosigmoid, and the small bowel also may be dilated. Air-fluid levels can be seen in the small intestine but usually do not occur in the colon. Haustral folds often are visualized despite severe distention.
PROGNOSIS
The mortality rate of patients with acute colonic pseudo-obstruction varies from 0% to 32% and is partly determined by their comorbidity.3,104 Older patients, poor clinical condition, and surgical treatment for acute colonic pseudo-obstruction are associated with an increased risk of mortality. There are no randomized clinical trials comparing surgical and medical treatment to clarify whether surgery itself or selection bias influences mortality associated with surgical treatment. Intestinal ischemia or perforation, which supervenes in about one in every six or seven cases, is associated with a 40% increase in the risk of death.3
The diameter of the colon is also a risk factor for mortality. When surgical decompression is utilized in mechanically obstructed patients with a cecal diameter greater than nine centimeters, there is a dramatic reduction in mortality,105 which is the basis for the nine-centimeter cutoff as a sign of impending perforation in patients with acute colonic pseudo-obstruction. In one study, perforation rates for cecal diameters less than 12 cm, 12 to 14 cm, or larger than 14 cm were 0%, 7%, and 23%, respectively.3 Mortality also was associated with delay in decompression: 15% in those decompressed less than four days after onset of dilatation; 27% when the decompression occurred after four to seven days; and 73% after day seven.
PREVENTION
Minimally invasive surgery, thoracic epidural anesthesia, and nominal use of opioid analgesia have led to improved care of surgical patients. Enhanced operative recovery programs, referred to as multimodal or fast-track programs, combine modalities that individually have a lower morbidity compared with standard treatment.72,106 Methods used in some fast-track programs are listed in Table 120-7.69 Studies have shown various fast-track programs can reduce the duration of ileus and the costs and duration of hospital stay while decreasing cardiopulmonary morbidity and postoperative convalescence.
Table 120-7 Some Methods Used in Fast-Track* Rehabilitation Programs
* Fast track refers to the use of enhanced recovery management strategies to improve outcomes after surgery.
Modified from Kehlet H. Fast-track colorectal surgery. Lancet 2008; 371(9615):791-3.
TREATMENT
The goal of management is to achieve colonic decompression. With correction of reversible potential causes or associated imbalances (e.g., infection, hypovolemia, hypoxemia, electrolyte levels), discontinuation of medications that can induce ileus (e.g., anticholinergics, opiates), the ileus disappears by day six in 83% to 96% of patients.3 Intravenous saline and glucose solutions suffice for hydration because of the short-lived and reversible nature of the dysfunction in most cases; in patients with prolonged acute colonic pseudo-obstruction, parenteral or enteral nutrition may be necessary.107 Nasogastric aspiration for nausea and vomiting may be beneficial, but often it is ineffective because the functional obstruction affects the colon. Rectal tubes may be useful if the sigmoid colon is dilated. Enemas might “cleanse” the colon, but only Gastrografin enemas have shown efficacy in anecdotal reports. Enema use has been complicated by colonic perforation.108 When the diameter of the cecum is greater than nine centimeters and has not responded to treatment within the first 72 hours after diagnosis, decompression should be performed to reduce the risk of ischemia, perforation and death.3 A treatment algorithm is shown in Figure 120-4.
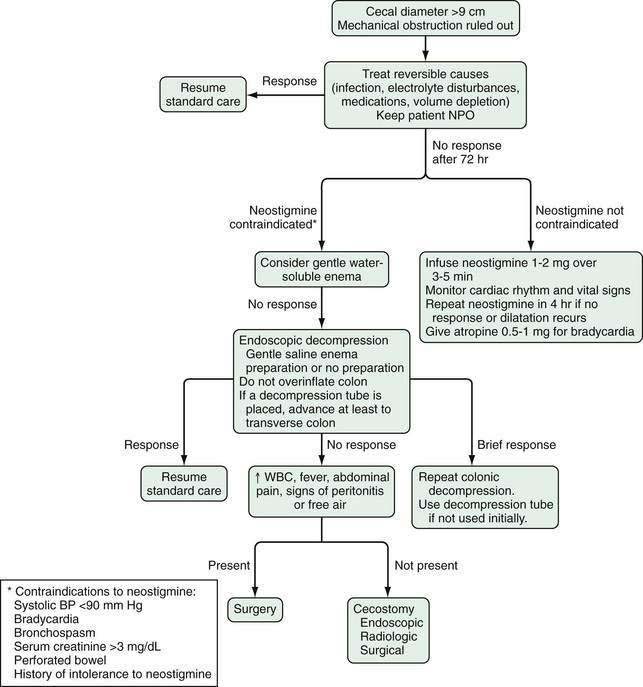
Figure 120-4. Algorithm for the treatment of acute colonic pseudo-obstruction. NPO, nothing by mouth; WBC, white blood cell count.
Medical Decompression
Adrenergic blockers and the acetylcholinesterase inhibitor neostigmine have been tested in open-label studies. Only neostigmine has been tested in a randomized, controlled trials and has an effective initial treatment response rate of 60% to 90%.109,110
5-HT4 receptor agonists, motilin receptor agonists, and muscarinic receptor agonists have been the subject of anecdotal reports, but none have been formally tested in the setting of acute colonic pseudo-obstruction.108 Metoclopramide has shown very small or insignificant benefit in the treatment of postoperative ileus.92 The peripherally acting µ-opioid receptor antagonist alvimopan significantly shortens the duration of postoperative ileus, but neither metoclopramide nor alvimopan has been sufficiently tested as treatment for acute colonic pseudo-obstruction.89–92
Endoscopic Decompression
Randomized, controlled trials of endoscopic decompression are lacking. Colonoscopic decompression can be achieved technically in 80% of patients with acute colonic pseudo-obstruction, albeit with a high risk of cecal perforation.110 The complication rate ranges from about 1% to 5%,5 with a 3% perforation rate.104 Colonic decompression has not been shown to improve the outcome of these patients. It has a high recurrence rate and colonoscopy of unprepared bowel can distend the colon further and result in perforation.3 Placement of a decompression tube into either the right or transverse colon has a similar technical success rate.104 Endoscopic decompression should be considered in patients with a high risk of cecal perforation when conservative and pharmacologic maneuvers have failed.