Figure 86 Upper GI endoscopy showing candida in the esophagus as white curd-like patches
Esophageal candidiasis is seen most common in patients with hematologic malignancies and human immunodeficiency virus-infected patients.
• Most patients also have oral thrush.
• Esophageal candidiasis may also be seen with steroid use, even inhaled corticosteroids.
• The most common symptom is localized retrosternal odynophagia.
• Differential diagnosis if from other infections like cytomegalovirus, herpes simplex virus, medication-induced esophagitis, and eosinophilic esophagitis.
• Diagnosis is made during upper endoscopy, showing white or yellowish plaque-like lesions on the mucosal surface. Microscopy and cultures can confirm the diagnosis, if in doubt.
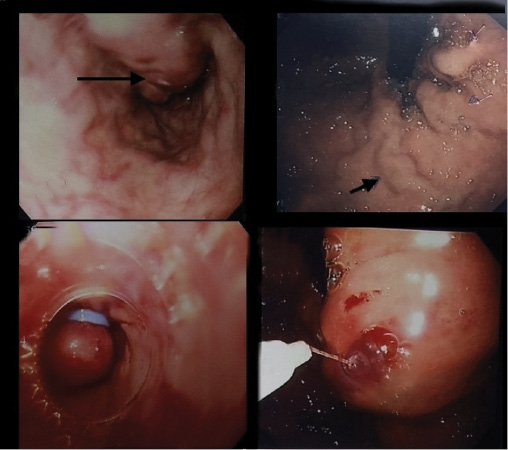
Figure 87 Endoscopy showing esophageal and gastric varices treated with esophageal ligation and gastric varices cyano-histoacryl injection. Top slides show esophageal and fundal varices. Bottom slides show intervention by band ligation for esophageal varices and cyanohistoacryl injection of the fundal varices
Treatment of acute variceal hemorrhage.
• Hemodynamic stabilization and correction of coagulopathy and transfusion (avoid over transfusion) to target hematocrit of about 40.
• Offer terlipressin, somatostatin, or octreotide at admission, even before confirmation by endoscopy, and continue for three to five days in addition to endoscopic band ligation or sclerotherapy, depending on the expertise within 12 h of presentation. A second session may be performed, if needed.
• Balloon tamponade is reserved for unresponsive cases waiting for TIPS (transjugular intrahepatic portosystemic shunt) or surgical interventions.
Figure 88 Esophagoscopy showing severe esophagitis, esophageal ulcer, and hiatus hernia. (a = severe sloughed mucosal lining, b = severe esophagitis active, c = hiatus hernia, d = severe esophagitis covering more than 75 percent of the esophagus, e = severe esophagitis with friable mucosa, f = distal esophageal ulcer)
Esophagitis is most commonly seen with gastroesophageal reflux disease. It may also be associated with the following conditions:
• Candidiasis.
• Medications, radiation, caustic and nasogastric tube associated.
• Infection with herpes, cytomegalovirus, and HIV infection.
• Crohn’s disease.
• Eosinophilic esophagitis.
• Tuberculosis and actinomycosis.
• Behcet’s disease, pemphigoid, and epidermolysis bullosa.
Figure 89 Endoscopy showing proximal esophageal web (narrowing), which was associated with Plummer–Vinson syndrome
Plummer–Vinson syndrome presents as a classical triad of dysphagia, iron-deficiency anemia, and esophageal webs. Also see details of Plummer Vinson syndrome on page 102 in Volume I.
• The syndrome is extremely rare.
• Most of the patients are white middle-aged women, in the fourth to seventh decade of life.
• The importance of Plummer–Vinson syndrome is due to the association with upper alimentary tract cancers, especially squamous cell carcinoma of the pharynx and the esophagus.
• Plummer–Vinson syndrome can be treated effectively with iron supplementation and mechanical dilation (before the development of carcinoma).
Figure 90 Duodenal kissing ulcers in background of mild duodenitis
Peptic ulcer disease may be asymptomatic in two-third of the patients and only present when there is a complication. Dyspepsia with upper abdominal pain and discomfort is present in 80 percent. Also see details of peptic ulcer disease on page 94 in Volume I.
• Upper GI endoscopy is best for diagnosis (Figures 93 and 94), but asymptomatic cases may be picked up on a barium study (Figure 57).
• Bleeding is manifested by hematemesis or coffee ground vomiting, and melena. Massive bleeding may lead to hematochezia and volume loss causing postural hypotension and tachycardia.
• Gastric outlet obstruction is a feature of pyloric channel or duodenal ulcers.
• Penetration is associated with change in pattern and radiation of the pain that is not relieved. Posterior penetration may be associated with rise in serum amylase.
• Perforation most commonly is seen with duodenal ulcers accounting up to 60 percent of the cases.
• Any patient having peptic ulcer disease should be tested for H. pylori infection.
Figure 91 Endoscopy showing active duodenal ulcers in the first part, being treated with endoclipping in the background of duodenitis
Peptic ulcer disease represents about 40 percent of all cases of upper GI bleeding. Also see details of peptic ulcer disease on page 94 in Volume I.
• Risk of developing bleeding peptic ulcer with steroids use is debated, but when combined with nonsteroidal anti-inflammatory drugs (NSAIDs), incidence of hemorrhage increases by tenfold.
• Peptic ulcers are very often associated with H. pylori or NSAID uses (approximately 96 percent).
• A rapid urease test (RUT) on biopsy is done in PUD (patient should not be bleeding or taking PPI). Histology can be followed. Other option is a delayed 13C-urea breath test (UBT) and stool antigen testing or serology for H. pylori.
• Once an infection is diagnosed, antibiotic treatment is advocated.
• Outcome of endoscopic management: Hemostasis achieved in more than 95 percent, recurrent bleeding in less than 15 percent and mortality occurs in 6 to 8 percent.
Figure 92 Gastroscopy showing polypoid, umbilicated, raised ulcer-like lesions on the greater curvature of the stomach. Biopsy revealed a carcinoid tumor
Carcinoids are neuroendocrine tumors with more than half arising from the GI tract. Gastric carcinoids (Figure 92) are of three types. Type 1 being common in women are associated with atrophic gastritis and pernicious anemia. Type 2 occurs with Zollinger–Ellison syndrome (MEN-1). Type 3 is sporadic and more malignant. Also see details of carcinoid on page 121 in Volume I.
• Gastric carcinoids represent 2 to 3 percent of all GI carcinoids, but only 0.3 percent of all gastric tumors.
• The commonest site of the tumor is the terminal ileum.
• They are usually located in the body or fundus of the stomach, and may appear polypoid.
• They arise from GI neuroendocrine cells, and some are thought to develop as a result of high circulating gastrin.
• Endoscopy often demonstrates a submucosal mass with a central umbilication.
• Biochemical diagnosis requires measurement of serum 5 hydroxyindoleacetic acid (5OH-IAA).
• Clinical triad of diarrhea, flushing, and wheezing occurs when there is hepatic metastasis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree