Chapter 43 Hysteroscopic Management of Intrauterine Adhesions and Uterine Septa
INTRAUTERINE ADHESIONS
Etiology
Synechiae refers to adhesions that join together body parts, and this term is commonly used as a synonym for adhesion within the uterine cavity. In 1948, Asherman was the first to describe the frequency of uterine synechiae and the etiologic symptoms associated with the condition.1 Since then, the presence of intrauterine adhesions has also commonly become known as Asherman’s syndrome.1,2 Genital tuberculosis was first described by Netter in 1956.3 The classic observations were chronic inflammation of the endometrium resulting in severe intrauterine adhesions and often complete destruction of the endometrium, also known as Netter’s syndrome. It is quite evident that the development of adhesions requires at least one, if not all, aspects of uterine trauma and local infection to occur.
The main predisposing factor for its development is overzealous curettage postpartum or postabortion. Therefore, a mainstay in the prevention of adhesions is the avoidance of unnecessary curettage. Early detection of intrauterine synechiae is also a key preventive feature after intrauterine surgery, curettage, or spontaneous abortion to identify early adhesions that are filmy, thin, and easily resected with prompt adhesiolysis.4–6
Prevalence
The exact incidence of uterine adhesions in women of reproductive age is not known, but it is an infrequent cause of secondary amenorrhea, infertility, and recurrent pregnancy loss. The reported incidence of intrauterine adhesions with diagnostic hysteroscopy is only 1%, and the overall prevalence may be in the range of 1.5%.6,7 However, the prevalence of intrauterine adhesions seen in women undergoing hysterosalpingography (HSG) is reported to be 2.7%; in women with subfertility, adhesions are seen in 4% of cases.8,9
Dicker and colleagues4 also reported that previous abortion does not predispose to intrauterine adhesions in a review of 144 women; hence, the prevalence with an uncomplicated curettage is 2.1%. The incidence of Asherman’s syndrome in a select group of women especially after curettage for missed or incomplete abortion is reported in the range of 17%, but rates as high as 30% are reported in the literature, the majority of which are mild in severity.10–13 Furthermore, in at-risk women, such as those who have undergone postpartum or incomplete curettage, the rate is speculated to be even higher.14,15
The prevalence of intrauterine adhesions in women undergoing postpartum curettage or repeat curettage for a previously incomplete curettage for missed abortion or medical abortion was reported in a prospective study of 50 women and found to be present in 40%, of whom 75% had grade II to IV intrauterine adhesions as classified by the European Society of Hysteroscopy.21 In women with menstrual disorders, a statistically significant 12-fold increase in moderate to severe Asherman’s syndrome was noted. A history of prior abortion or infection during the initial surgery was associated with a mildly but not statistically significant increase in the risk of Asherman’s syndrome.
Risk Factors
Risk factors that should raise the index of suspicion for the presence of intrauterine adhesions include postpartum or postabortion curettage causing menstrual disturbance.11 Friedler and colleagues11 reported on the incidence of intrauterine adhesions with one or multiple abortions. The incidence of intrauterine adhesions after one, two, or three or more abortions was 16.3%, 14%, and 32%, respectively. The severity of adhesions was higher if at least two or more abortions were documented. There was no association between the number of previous intrauterine procedures and the presence of adhesions in asymptomatic women, but significant correlation was seen in women with menstrual disorders. The presence of infection at the initial procedure increased the presence of adhesions in this study, although it failed to reach statistical significance.
Pathophysiology
Any intervention that destroys the endometrium may generate adhesions of the myometrium in the opposing uterine walls. The key predictive factor to intrauterine adhesions is the gravid uterus. The gestational changes noted with a gravid uterus soften the uterine wall, resulting in greater denudation of the basalis layer with surgical intervention. The basalis layer is the regenerative layer of the endometrium.16
The most common contributing factor is an overzealous postpartum or postabortion curettage. The critical timing of the development of adhesions after uterine trauma in a gravid uterus is the first 4 weeks of the puerperium. The mechanism is probably secondary to an excessive form of wound healing. Pregnancy was found to be the predisposing factor in 91% of cases, of which 66.7% were postabortion curettage, 21.5% postpartum curettage, 2% cesarean section, and only 0.6% evacuation of a molar pregnancy.16 The contribution of infection at the time of the initial intervention in the pathophysiology of this syndrome is unknown and remains controversial13,17–19 Other reported causes include genital tuberculosis and previous uterine surgery, such as myomectomy.20
The gross pathologic changes seen in the uterus can range from marginal adhesions to complete obliteration of the cavity. The adhesions can vary from markedly dense to filmy. Adjacent to intrauterine adhesions are areas of endometrial sclerosis, which is more pronounced with dense adhesions.21
A key prognostic factor in the regeneration of endometrial tissue after adhesiolysis is the presence of the endometrial basalis, which serves as the anchoring point for the formation of new endometrium. Hence, muscular adhesions carry the worst prognosis because they are devoid or deficient in the regenerative basalis layer.22 The source of intrauterine adhesions can be endometrium, myometrium, or connective tissue, each of which has distinct characteristics.
The presence of adhesions within the uterine cavity can limit uterine muscle activity and endometrial perfusion, resulting in atrophy and consequently diminishing the amount of receptive endometrium available for normal implantation.23 Impairment of normal growth and development of an implanted embryo is due to the limited space available and the impaired blood supply to the embryo.22 The postulated mechanism for poor reproductive outcome or recurrent pregnancy loss in women with intrauterine adhesions includes implantation failure secondary to endometrial atrophy with defective vascularization.
Scanty endometrium with a damaged blood supply results in a lack of response to estrogenic stimuli associated with the extent of the adhesions present.23,24 Adhesions can also exist near the tubal ostia and cause tubal ostia obliteration or occlusion, further hindering implantation.
Classification
The classification systems in existence for intrauterine adhesions include those that classify according to pathologic localization or according to hysteroscopic findings that define the location and extent of uterine adhesions. In addition, a few prognostic classification systems based on menstrual pattern exist.6 The most commonly reported classification systems used include those by Valle and Sciarra,25 Donnez and Nisolle,26 the European Society for Hysteroscopy,27 March and coworkers,28 the American Society for Reproductive Medicine (ASRM; formerly the American Fertility Society),29 and Nasr and coworkers.30
The only two classification systems that include menstrual pattern as a prognostic factor are the ASRM and Nasr classification systems.29,30 The potential value of including in the classification system the presence or absence of menstrual abnormalities may be indicative of the amount of endometrium available for regeneration after adhesiolysis and may be of prognostic significance.
Intrauterine adhesions at the time of hysteroscopy have been classified by March and colleagues28 into three categories as mild, moderate, and severe (Table 43-1). Briefly, adhesions can be characterized either by multiple avascular strands of fibrous tissue between the anterior and posterior uterine walls, vascularized and dense adhesions that contain inactive endometrium or myometrium or muscular adhesions where there is no notable endometrial basalis.
Table 43-1 March Intrauterine Adhesion Classification System
| Grade | Finding |
|---|---|
| Minimal | |
| Moderate | |
| Severe |
From March CM, Israel R, March AD: Hysteroscopic management of intrauterine adhesions. Am J Obstet Gynecol 130:653–657, 1978.
March Classification
Intrauterine adhesions can be further characterized based on the extent of uterine involvement.28 Minimal adhesions are said to be present if less than one fourth of the uterine cavity is involved, the adhesions are thin and filmy, and the fundal and ostia areas are minimally involved or devoid of any adhesions. Moderate adhesions involve one fourth to three fourths of the uterine cavity; no agglutination of the uterine wall is seen, only adhesions are present, and the tubal ostia and fundus are only partially occluded. Severe adhesions involve more than three fourths of the uterine cavity, with agglutination of the uterine walls or thick bands with occlusions of the tubal ostia and the upper uterine cavity. The March classification system is simple and easy to apply, but it is not prognostic.28 The most accurate classification system used that describes the adhesion site and density is the European Society for Hysteroscopy system, but it is very difficult to apply or utilize clinically.27
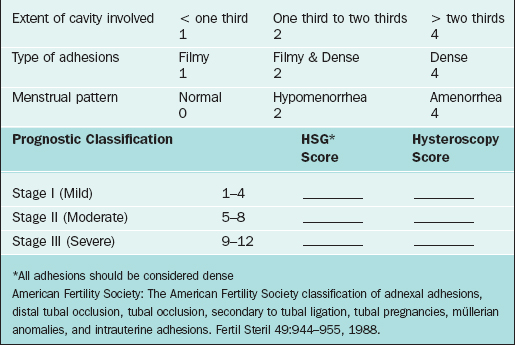
American Society for Reproductive Medicine Classification
According to the 1988 ASRM classification system, synechiae are classified in three stages, with stage III being complete obliteration of the uterine cavity (Table 43-2).11 The ASRM classification system provides both an indirect and direct grading of intrauterine adhesions with HSG and hysteroscopy, respectively. The location of the adhesions is presumed to be prognostic for reproductive outcome given that most implantation occurs in the top fundal portion of the uterine cavity, and cornual adhesions may cause tubal obstruction.
Clinical Manifestations
The most common single presentation is infertility, representing 43% of reported cases; second is amenorrhea, representing 37% of cases.31 The rate of abnormal placentation, although elevated in women with intrauterine adhesions, is the least common presentation reported in women with intrauterine adhesions.
Diagnosis
Radiologic Imaging
Transvaginal sonography has replaced transabdominal sonography as an imaging tool for detection of uterine pathology.32 Transvaginal ultrasonography (TVUS) was assessed in 200 patients being investigated for infertility. The overall sensitivity in the detection of endometrial pathology was 98.9%, with a positive predictive value of 94.3% and false-positive rate of 5.5%.32 The overall specificity of TVUS for normal findings was 31.3% and the negative predictive value was 71.4%; however, these data were limited given the small number of patients with normal findings reported. In this study the positive predictive value for the detection of intrauterine adhesions was 98.5%.32 The sonogram was performed in the periovulatory phase of the menstrual cycle.
Another report assessed the predictive value of TVUS in 74 infertile women undergoing diagnostic hysteroscopy. The sensitivity, specificity, and positive and negative predictive value for the specific diagnosis of intrauterine adhesions were 80%, 100%, 100%, and 97%, respectively.33 However, in a separate series TVUS was unable to detect any of the cases of intrauterine adhesions, with three false-positive diagnoses,34 resulting in a sensitivity and positive predictive value of 0%. These conflicting reports could be due to technique, especially variation in the time in the cycle when the scan was performed.
The poor result of TVUS in some centers has been improved with the introduction of saline infusion sonohysterography, also referred to as sonohysterography. Sonohysterography is performed with TVUS and can further enhance the detection of intrauterine adhesions. Saline solution serves as a homogeneous, echo-free contrast medium, enabling better visualization of the uterine cavity than TVUS alone. Alborzi and colleagues34 published the largest series to date to evaluate the diagnostic accuracy of HSG and sonohysterography compared to laparoscopy and hysteroscopy as the gold standard. The prospective study reviewed 86 women with infertility. In this study sonohysterography had a high diagnostic accuracy for the detection of Asherman’s syndrome, greater than that for HSG, with a sensitivity of 76.8%, a specificity of 100%, a positive predictive value of 100%, and a negative predictive value of 97.7%.
In a separate study both HSG and sonohysterography had similar diagnostic accuracy.36 Sensitivity of both studies was 75%; HSG had a positive predictive value of 43% and sonohysterography had a positive predictive value of 50%. The negative predictive value of both studies was close to 100%.35 The use of magnetic resonance imaging (MRI) in the diagnosis of intrauterine adhesions remains to be elucidated.36
Technique
Transvaginal ultrasound should be performed in the late follicular or early luteal phase of the cycle (cycle day 7, 14, or 21) using a real-time sector transvaginal probe with imaging frequencies of 5 and 7.5 MHz. In fact, the periovulatory phase is the best time to evaluate the uterine cavity contours because the endometrium is thick enough to appear more echogenic than the myometrium and not too thick to obscure the midline echo. The classic appearance of the three-layer endometrium enables better imaging of uterine defects than the postmenstrual endometrium, which is thin, less than 3 mm.
The contour of the endometrial cavity is inspected for both irregularities and echo pattern of the myometrium–endometrium interphase in the sagittal (long axis) and transverse plane. The diagnostic criteria used for the diagnosis of intrauterine adhesions is interruption in the midline echo in the periovulatory phase of the cycle. The typical appearance is focal, hyperechoic, irregular, often cordlike structures seen within the echo-free space between the basalis layers, which interrupt the continuity of the endometrial cavity. These structures can vary in size from 2 to 6 mm or in location within the cavity.33
Surgical Treatment
Historical and Uncommonly Used Techniques
The classic blind dilation and curettage has gradually been abandoned in favor of the hysteroscopic approach for intrauterine adhesiolysis.16,22,25,37,38 Hysteroscopy can be performed in an outpatient setting and allows both the determination of the extent of adhesions under direct visualization and prompt treatment concurrently. A number of studies report resection of intrauterine adhesions by hysterotomy. In a review of 31 cases in 12 published studies, only 16 patients (52%) conceived, of which 8 resulted in live births, and 4 patients required a cesarean hysterectomy secondary to placenta accreta.16
Operative hysteroscopy has replaced dilation and curettage or blind dissection in the treatment of intrauterine adhesions and is the treatment of choice.16,22,25,37,38
Hysteroscopic Surgery
The mainstays of treatment for intrauterine adhesions are early detection and prompt surgical treatment to minimize further complications. Hysteroscopy has become not only an accurate tool for the diagnosis of adhesions, but also the main method for their treatment. Hysteroscopic lysis of adhesions is indicated when the extent of adhesions is moderate to severe or access to tubal ostia is blocked. The significance of mild adhesions is still controversial, yet surgical treatment may be considered if all other causes of infertility or recurrent pregnancy loss have been excluded or successfully corrected with persistent reproductive failure. It also appears prudent to restore the uterine cavity to normal before assisted reproductive technology (ART) treatment, yet evidence remains sparse.4
An additional use, albeit with limited data, is the treatment of intrauterine adhesions secondary to genital tuberculosis prior to in vitro fertilization–embryo transfer. However, the reformation rate is reported at 100%.37
Technique
Operative hysteroscopy is performed classically under general anesthesia using either an operative hysteroscope or resectoscope. Hysteroscopic adhesiolysis can be performed under local anesthesia in an outpatient setting with or without analgesics.16 The uterine cavity is distended using nonconductive hypo-osmolar solution under manometric control if electrosurgery is used. The most common solutions used are glycine (1.5%), sorbitol (2.7%), and mannitol (0.54%). The basic technique involves resection of the intrauterine adhesions by sharp or blunt dissection. Successful hysteroscopic resection can be accomplished by the use of sharp dissection using semirigid scissors, electrosurgery, or fiberoptic laser.
The adhesions are incised with a high-frequency resectoscopic manual electrode needle using an angled electrode, 90-degree loop. The theoretical concern with the use of electrocautery is the negative effect of thermal damage on the endometrium and myometrium with potential risk of uterine rupture with a subsequent pregnancy. If the extent of adhesiolysis is severe, the use of laparoscopy has been promoted to reduce the risk of uterine perforation.16,25,28 Reports also exist of the use of intraoperative fluoroscopic division of adhesions, but often adhesiolysis is incomplete.39 However, there is no clear advantage for the use of electrosurgery or laser over sharp adhesiolysis using hysteroscopic scissors through the operative channel of the hysteroscope. Recent reports also include the use of the coaxial bipolar electrode system in a limited number of cases for intrauterine adhesiolysis. Its efficacy and safety appear to be similar to the conventional techniques used, but further studies need to be conducted.40,41
A case report introduced the concept of hysteroscopic adhesiolysis with guidance of a laparoscopic ultrasound in a patient with infertility and intrauterine synechiae.42 A 7.5-MHz laparoscopic ultrasound transducer was introduced though a 10-mm port; placing the scanning surface of the probe firmly on the uterine serosa yielded a high-quality real-time image and safe resection of the synechiae. The potential benefit over conventional transabdominal techniques includes proper localization of the hysteroscopic instruments and greater definitions of the uterine walls to minimize uterine perforation. The technique holds promise, but further studies need to be conducted before it replaces other procedures.42–44
Adhesiolysis begins inferiorly and is carried out cephalad until a panoramic view of the endometrial cavity can be obtained and the tubal ostia are seen. The initiation of the adhesiolysis is from the internal os. Filmy and central adhesions should be cut first; marginal and dense adhesions should be approached last.39 The maintenance of adequate distension is key to the successful resection of intrauterine adhesions. Valle and Sciarra25 described the use of methylene blue injection through the inferior channel of the hysteroscope when it is difficult to ascertain adhesions from a normal endometrial lining. This technique may help delineate a plane of cleavage for safe adhesiolysis. Operating time for hysteroscopic adhesiolysis varies depending on the severity of adhesions present and often may require a second intervention for adequate resection. The average operating time is 30 minutes, with a range of 10 to 60 minutes.
The published studies that describe the successful use of a coaxial bipolar electrode surgical system report similar results to conventional techniques.40,41,45–47 In a series of 50 patients, of which 12 were identified with uterine adhesions and the other 12 with uterine septum, septoplasty, and intrauterine adhesiolysis was successfully completed without any major complications reported.40 The use of the bipolar vaporization system was well-tolerated, safe, and likely an effective alternative to the conventional hysteroscopic techniques in the treatment of intrauterine adhesions. A key advantage appears to be the small diameter of the electrodes used, which can easily be inserted through a #5 French working channel of a 5.5-mm hysteroscope, as well as the use of normal saline solution, which is associated with reduced incidence of hyponatremia.
Women with severe intrauterine adhesions and complete obliteration of the uterine cavity are the most challenging surgical cases. The key to the success of treatment is in defining the correct plane of dissection without causing a uterine perforation.28 McComb and Wagner48 have described a simplified technique for women with severe Asherman’s syndrome. In a series of six women successful adhesiolysis was accomplished using a Pratt cervical dilator first. This allowed some space to start the hysteroscopy. The curved tip points laterally toward the uterine cornua aligned with the plane of the uterine corpus. The technique is performed bilaterally, thus converting the obliterated cavity in the configuration of a uterine septum.
Similar techniques have been used with the use of fluoroscopic guidance with a 16-gauge, 80-mm Tuohy needle that is introduced alongside a 5-mm hysteroscope with similar results.39 The goal is to create a passageway using either the dilator or needle with subsequent division of the adhesions under direct vision with the hysteroscopic scissors. These specialized techniques often require multiple procedures to achieve adequate adhesiolysis.39,49,50
Radiologic Techniques
Blunt disruption of adhesions using either insemination or HSG balloon catheters has also been described.51,52 Fluoroscopic-guided lysis of intrauterine adhesions was originally reported by Ikeda and colleagues51 and further developed by Karande and colleagues.52 Both procedures can be performed at the time of diagnostic HSG. Karande described a small series of patients in whom in-office lysis of intrauterine adhesions under gynecoradiologic control using balloon tip HSG catheters or hysteroscopic scissors inserted through the main port of the catheter was performed. Successful lysis of adhesions occurred in 81.2% of the patients, but in women with moderate or severe adhesions the procedure was abandoned secondary to significant discomfort, only leading to partial resection of the adhesions.
Recent reports have also described a therapeutic role of sonohysterography for the treatment of uterine adhesions. Coccia and coworkers53 described a newly developed treatment technique for intrauterine adhesions based on sonohysterography. The technique uses saline infusion under pressure lavage of the uterine cavity to mechanically disrupt adhesions. Saline solution is initially injected slowly (5 to 10 mL) and then under increasing pressure until pain is experienced by the patient, at which point the infusion is stopped. The same procedure is repeated several times until complete uterine distension is visualized with no residual interruption of the endometrial contour nor filling defects noted.
Prophylactic antibiotics and an estrogen/progesterone preparation were used after the procedure. This procedure was named the PLUG method (pressure lavage under ultrasound guidance; see Chapter 30); however, generalization of the results is limited given the small sample size (7 patients) reported. The procedure was well-tolerated, not requiring local or general anesthesia; the mean duration of the procedure was 17 minutes. The technique was more efficacious for the lysis of mild adhesions. A high rate of recurrence was noted in women with moderate to severe adhesions, due to a higher rate of incomplete adhesiolysis. Menstrual cyclicity was restored in all patients, but limited data on fertility were available. Only one of the three infertile women treated had a live birth.
Postoperative Care
Despite advances in the development of techniques for adhesiolysis, the two basic problems associated with poor outcome with these procedures still exist: the inability to treat extensive or severe adhesions and the lack of methods to prevent recurrence of the adhesions postoperatively. The use of intrauterine devices, Foley catheters, antibiotics, steroids, and high-dose estrogen postoperatively to prevent recurrence of adhesions is still widely debated, and no consensus exists.16
Intrauterine Device
An IUD was traditionally used. However, the modern IUD, such as the copper-bearing IUD and the Progestasert, may have too small a surface area or cause too much of an inflammatory reaction to be of any benefit. The reported preference was to use the Lippes Loop IUD.16,54 The value of the IUD is to keep the raw, freshly dissected surfaces separated during the initial phase of healing in hopes of reducing the chance of adhesion reformation.
Most surgeons now use a Foley catheter with an inflatable balloon to keep the freshly dissected uterine surfaces separated. The Foley catheter is inserted into the uterus posthysteroscopy and remains in situ for approximately 1 week in most circumstances. Those that do not recommend its use suggest that it may impede endometrial regeneration by the simple pressure on the uterine wall from the inflated balloon.16 A uterine balloon stent (Cook OB/GYN, Spencer, Ind.) has been developed with a balloon that is heart-shaped and flat to conform better to the uterine cavity, although no comparative data is available for this device.
Schenker16 reported on 642 patients with menstrual disorders treated with an IUD; 92% regained normal menses and 8% were hypomenorrheic. Among the 405 infertile women, 55% conceived, of whom 61% had a term delivery, 25% aborted, 7% had preterm labor, and 7% had abnormal placentation (placenta accreta). In 167 women who had insertion of a Foley balloon after adhesiolysis, 47% conceived, of whom 68% had a term delivery, 8% had preterm labor, 18% aborted, and 5% had placenta accreta. Of note, in 292 women with mild intrauterine adhesions without treatment, 133 (45%) conceived, of which 30% were term, 23% preterm, 40% aborted, and 13% had placenta accreta.
Prevention
The use of adhesion prevention barriers has been also reported to prevent intrauterine adhesions after curettage. A recent randomized, controlled, prospective trial describes the use of a bioresorbable membrane postoperatively within the endometrial cavity in 150 women with incomplete or missed abortion with or without a history of at least one or more prior curettage. In women with no prior history of curettage who used the membrane, all were able to conceive within 8 months after adhesiolysis compared to women who did not use the membrane, in whom only 54% conceived. In women who did not conceive with a history of prior curettage and the use of the membrane, 90% were found to be adhesion-free compared to only 50% in the untreated group. Further studies are needed before its routine use is advocated.55
Complications
The complications associated with hysteroscopic adhesiolysis can be viewed in two major categories: those intrinsic to operative hysteroscopy and those related to the technique of adhesiolysis itself. The complications related to operative hysteroscopy are reviewed in detail in Chapter 45. In summary, the reported complications seen with operative hysteroscopy include the possibility of fluid overload, perforation, and pelvic organ injury that includes thermal damage. The overall complication rate associated with hysteroscopy is reported to be 2.7%.45,56 Furthermore, the potential risk seen with the use of the electrosurgical system includes genital burns.57,58
The rate of uterine perforation during hysteroscopic surgery is less than 2% (1.6%), of which most are recognized (97%) during the procedure. The perforation risk is highest with intrauterine adhesiolysis or during hysteroscopic adhesiolysis.16,59 The risk of postoperative infectious complications is 1.42%, but the risk of early-onset endometritis is highest after lysis of synechiae compared to other hysteroscopic procedures, including uterine septa.59
Vaginal delivery is still recommended in women after hysteroscopic adhesiolysis unless extensive damage has occurred through thermal injury or a fundal perforation has occurred. Reports exist of potential catastrophic events, albeit rare, of uterine perforation with subsequent pregnancy or labor with or without uterine perforation. The risk of abnormal placentation is in the range of 8% and is speculated to be secondary to defective lamina basalis seen after adhesiolysis.60 It is recommended that pregnancy surveillance be vigilantly pursued to detect or rule out abnormal placentation as its lack of detection can lead to catastrophic events to both the mother and fetus.
Surgical Results
A number of series have been published reporting the outcome of hysteroscopic treatment of intrauterine adhesions. However, randomized clinical trials are lacking. There are also few reports about women with untreated intrauterine adhesions. Schenker16 reported on 292 women with mild intrauterine adhesions without treatment, of whom 133 (45%) conceived, of which 30% were term, 23% preterm, 40% aborted, and 13% had placenta accreta.
A report of 40 consecutive women with recurrent pregnancy loss (24 women) or infertility (16 women) resulting from intrauterine adhesions showed excellent surgical results with mild or moderate disease.38 Of the 40 women, 10 had mild adhesions, 20 had moderate adhesions, and 10 had severe adhesions according to the March classification system.28 Hysteroscopic adhesiolysis was performed with hysteroscopic scissors or monopolar electrosurgery. Prophylactic antibiotics were used; postoperatively, a pediatric Foley catheter was introduced and estrogen was administered. In women with hypomenorrhea as the presenting complaint, 67% reported normal menstrual cycles after adhesiolysis. All women with recurrent pregnancy loss conceived after adhesiolysis; 71% of pregnancies were term or preterm with a viable pregnancy. Among the women with infertility, 62% conceived resulting in a 37.5% live birth rate. Adhesion reformation was absent or rare in women with mild or moderate adhesions, reported as 0 to 10%. However, adhesion reformation was seen in 60% of women with severe intrauterine adhesions; none of the patients with severe adhesions conceived. Only one perforation was reported in a patient with severe adhesions.
Valle and Sciarra25 reviewed 81 infertile women and reported a term pregnancy rate of 81%, 66%, and 15%, respectively, in women with mild, moderate, and severe disease. Among these women with recurrent pregnancy loss the term pregnancy rate was 94%, 89%, and 65% in those with mild, moderate, and severe adhesions, respectively. The literature is unified and quite clear in that women with severe intrauterine adhesions, the reproductive outcome remains poor even after hysteroscopic adhesiolysis.25,38 In Valle and Sciarra’s series, of the 30 women with infertility and severe adhesions, 43% of women conceived, resulting in only a 10% live birth rate. Adhesion reformation rate is also strongly correlated with the extent of severity of the initial degree of adhesions, as is the reproductive outcome after hysteroscopic adhesiolysis. The recurrence rate of severe adhesions was 48.9% and decreased to 35% after repeat adhesiolysis.25
Zikopoulos and coworkers41 reported on 46 women who underwent hysteroscopic adhesiolysis either with the resectoscope or the coaxial bipolar electrical system. It is the largest series in which the coaxial bipolar system was used. Three women required a second attempt because of the presence of adhesions postoperatively and one patient required a third procedure. Restoration of menses in women with oligomenorrhea or amenorrhea was noted in 93% of the women.
The pregnancy complication rate noted was a preterm rate of 50% and hysterectomy for abnormal placentation (placenta accreta) in 2 of the 20 patients (10%). In addition, Zikopoulos and colleagues41 reviewed the literature of existing studies; they identified seven published studies in the past decade that examined delivery rates in women undergoing hysteroscopic adhesiolysis using an array of techniques. The overall delivery rate was 38.1% (48/126) among all the studies analyzed.
Pabuccu and colleagues38 reported the highest success rate among women with recurrent abortion with a delivery rate of 70.8% versus women with infertility, with a 37.5% delivery rate. The overall delivery rate was similar to that reported by Siegler and Valle60 in 1988 after reviewing a series of published studies that reported on a total of 775 women, of which 302 (38.9%) achieved a term delivery.
Women with adhesions secondary to genital tuberculosis carry the worse prognosis even after hysteroscopic adhesiolysis.37 In a series of 12 women undergoing 15 attempts at hysteroscopic lysis of uterine adhesions despite adequate restoration of the uterine cavity postoperatively, the reformation rate for severe adhesions was 100%, with a 25% uterine perforation rate. Women with severe intrauterine adhesions secondary to tuberculosis carry a poor prognosis; these authors recommend alternative fertility options such as surrogacy if initial attempts at surgical adhesiolysis have failed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree