Fig. 13.1
Small-caliber-tip transparent hood (ST hood). (a) A conventional ST hood (DH-16GR; Fujifilm, Tokyo, Japan). (b) A short ST hood (DH-28GR; Fujifilm, Tokyo, Japan)
Fig. 13.2
Illustration showing the sequence of pocket-creation method. (a) A flat neoplastic lesion indicated by the orange area. (b) Mucosal elevation by enough submucosal injection (indicated by the light blue area). (c) Initial mucosal incision at the closer edge of the lesion (blue line). (d) Creation of a submucosal pocket (blue area). (e) Extension of the submucosal pocket under the lesion. (f) Mucosal incision at the down-side lateral edge of the lesion. (g) Opening of the pocket by submucosal dissection at the lateral edge. (h) Extension of the mucosal incision over the middle line of the lesion at the distant edge of the lesion. (i) Extension of the submucosal dissection to the distant edge. (j) Completion of ESD
Submucosal Injection to Create a Submucosal Fluid Cushion Under the Lesion
Creation and maintenance of an adequate submucosal cushion is key factor for successful ESD. In order to create a long-lasting submucosal cushion, a 0.4 % sodium hyaluronate solution (MucoUp; Johnson and Johnson, Tokyo, Japan) is often used in Japan [9]. Sodium hyaluronate is a viscous substance with a high molecular weight that creates long-lasting mucosal protrusion when injected into the submucosa. Despite its high viscosity, it is an isotonic solution that causes no damage to the injected tissue [10].
A thick submucosal cushion with enough injection should be created. This thickened submucosal tissue provides safety margins for both the proper muscle and mucosal layers. The vertical (deep) resection margin is important for histopathologic assessment of invasion of the cancer. The depth of invasion and involvement of vessels are strong indicators of lymph node metastasis.
Using the pocket-creation method, the thickened submucosal cushion can be maintained throughout the entire ESD procedure.
Mucosal Incision at the Proximal Edge of the Lesion
After creation of a sufficient submucosal cushion, mucosal incision is made at the proximal edge of the lesion. The mucosal incision should be performed on the normal mucosa with enough distance (5–10 mm) from the edge of the lesion. The length of the initial mucosal incision should not be too long. Usually, about a 2 cm incision is enough for the initial mucosal incision for pocket creation (Fig. 13.3).
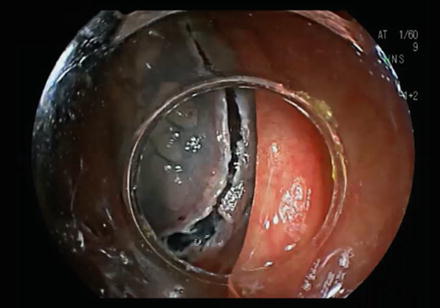
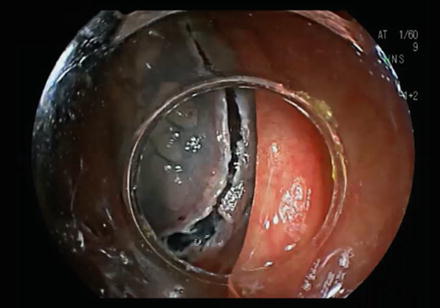
Fig. 13.3
Initial mucosal incision at the closer edge of the lesion
Submucosal Incision to Open the Incised Wound
After the mucosal incision, submucosal incision should be made to open the incised wound. At this initial stage, the incised wound cannot be opened with the tip of the hood yet, and so submucosal incision should be made by opening the wound with the tip of the sheath of the knife. Submucosal incision at the deep level close to the muscle layer is not necessary yet since it is still normal mucosa peripheral to the lesion. The submucosal layer right below the mucosa should be incised with the tip of the knife by moving the knife parallel to the muscle layer while slightly lifting the mucosa with its sheath (Fig. 13.4).
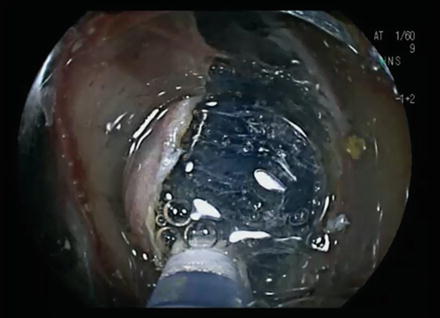
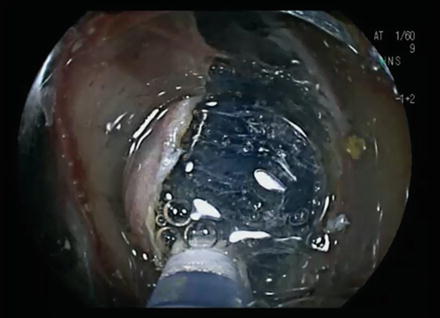
Fig. 13.4
Initial submucosal dissection with the tip of a Flush knife
Creation of the Submucosal Pocket
After repeating submucosal incision with the tip of the knife a few times, the incised wound can easily be opened by the tip of the ST hood. By opening the incised wound with the tip of the hood, the submucosal tissue can be clearly visualized (Fig. 13.5). Further dissection of the submucosal tissue should be made all the way to the deeper tissue that is close to the muscle layer, very carefully, until the muscle layer can be seen through the submucosal tissue.


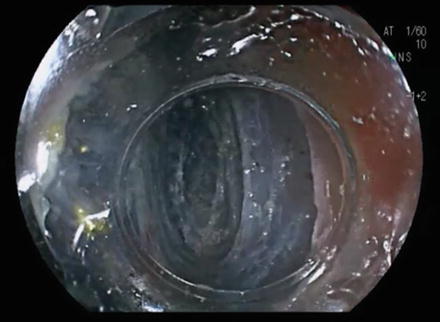
Fig. 13.5
Opening of the incised wound with the tip of the ST hood
By continuing dissection of the submucosal layer, a submucosal pocket is created. Once the transparent hood on the tip of the endoscope is inserted into the submucosal pocket, mechanical stretching of the submucosal tissue occurs. By making a submucosal pocket, the endoscope tip is stabilized, which allows for precise control of the knife. With precise control of the knife and a good safety margin obtained by the stretching of the submucosal tissue, selection of a good level of dissection becomes feasible. Adjusting the approach angle of the knife to be tangential to the wall is also easier with this method, because an adjusting force with the endoscope tip can be applied in either direction by pushing the mucosa up or pushing the muscle wall down with the tip of the hood. For every bit of submucosal dissection, the tip of the hood should be pushed down against the wall to see through the muscle layer first (Fig. 13.6). Then, the tip of the hood should be moved to the direction of the mucosa to adjust the approaching angle to be tangential to the muscle layer (Fig. 13.7). The dissection level of the submucosa should be selected at the level close to the muscle layer leaving a small amount of submucosal tissue on top of the muscle layer.
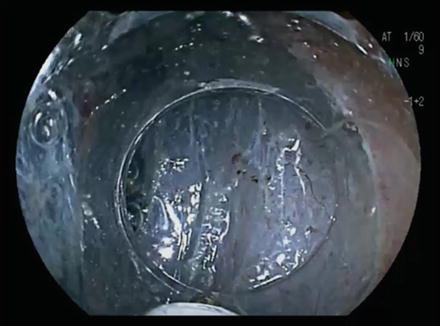
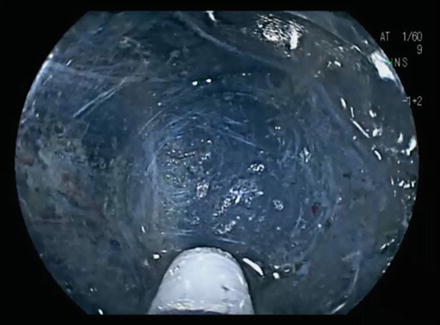
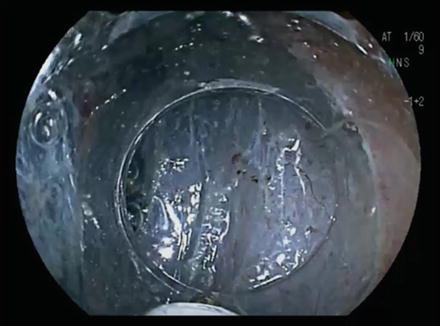
Fig. 13.6
Recognition of the muscle layer by pushing the tip of the hood down to the wall
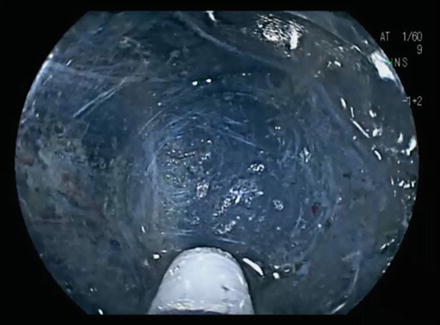
Fig. 13.7
Submucosal dissection after adjusting the approaching angle tangential to the muscle layer
With this pocket-creation method (Fig. 13.8), submucosal dissection can be happen under clear visualization of the submucosal tissue, and blood vessels can be carefully recognized for coagulation before cutting (Fig. 13.9). When a blood vessel is identified, it is better to dissect the submucosa around the vessel to isolate it (Fig. 13.10). By isolating the blood vessel, coagulation of the vessel becomes simple and effective. If bleeding occurs, the bleeding vessel should be pressed with the tip of the hood to temporarily stop the bleeding. Clear identification of the bleeding point makes hemostasis with hemostatic forceps easy. Good control of bleeding is a key factor for successful ESD.