Fig. 21.1
Indications for SPAS hepatectomy. A good indication for SPAS hepatectomy is a tumor located in the anterolateral segment of the liver. In addition, the resected specimen should not exceed 6-7 cm in size
21.3 Procedural Techniques
21.3.1 Position of the Patient and Layout of the Instruments
The patient, under general anesthesia, is placed supine with the legs apart. The operator stands between the patient’s legs. If the tumor is located on the patient’s left side, the assistant holding the scope stands at the patient’s right side, and vice versa (Fig. 21.2).
Fig. 21.2
Position of the patient and layout of the instruments for SPA hepatectomy
21.3.2 Insertion of a Multi-Access Port and Establishment of Pneumoperitoneum
A multi-access port is inserted through a 25-mm longitudinal incision made at the umbilicus. The port is fixed so that the working channels form an inverted triangle. Pneumoperitoneum is established at 8 mmHg. Upon transection of the liver parenchyma, the pressure is increased to 13 mmHg to suppress venous bleeding. A 5-mm deflectable laparoscope and two instruments are inserted through the port channels.
21.3.3 Mobilization of the Liver
Under cross-placement of the devices, an ultrasonic scalpel (SonoSurg™, Olympus Corporation, Tokyo, Japan or Harmonic ACE™, Ethicon Endosurgery, Cincinnati, OH, USA) is used to mobilize the liver (Fig. 21.3a). It is usually possible to cut the falciform ligament, left coronary ligament, and bilateral triangular ligament by means of dissecting devices inserted through the umbilical port. Extended mobilization of the right lobe is not possible in SPAS hepatectomy because the instruments inserted through the umbilical port cannot reach the superior and dorsal parts of the right lobe.
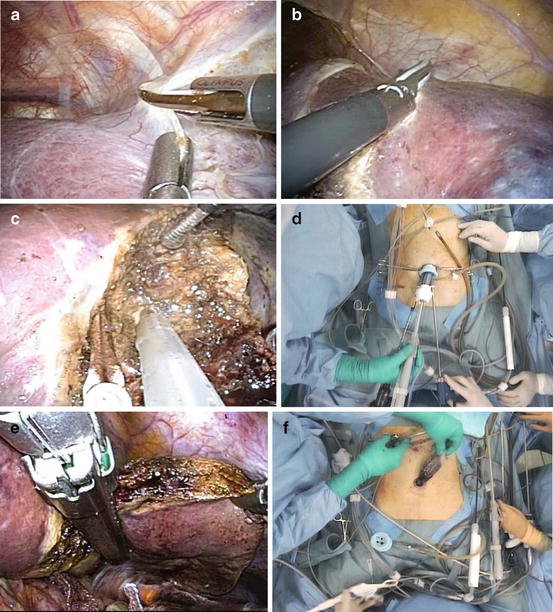
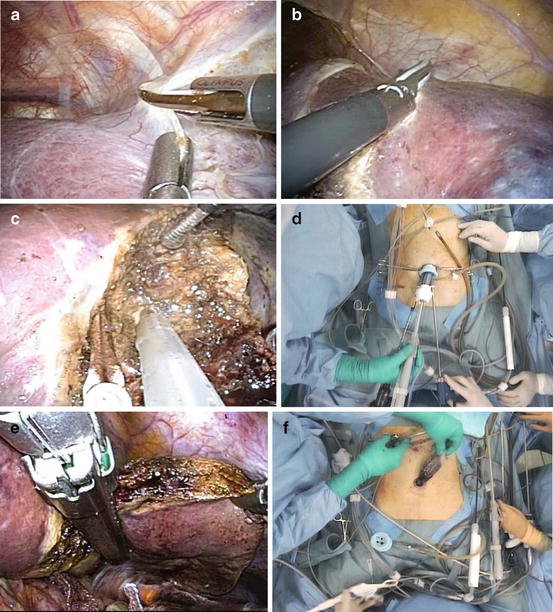
Fig. 21.3
SPAS lateral segmentectomy. (a) The falciform ligament is cut with an ultrasonic scalpel to mobilize the liver. (b) The superficial part of the liver can be cut with an ultrasonic scalpel. (c, d) We usually use CUSA Excel and BiClamp for transection of the deep part of the liver. (e) Large vascular pedicles are divided with a laparoscopic stapler. (f) The specimen is extracted transumbilically
21.3.4 Transection of the Liver Parenchyma
Intra-operative ultrasonography must be performed to determine the tumor location and the transection line. If the tumor is located at the edge of the liver, pre-coagulation will allow for bloodless transection with scissors and without energy devices. Generally, the pre-coagulation is performed along the intended line of transection with articulating microwave ablation instruments (Fig. 21.4).
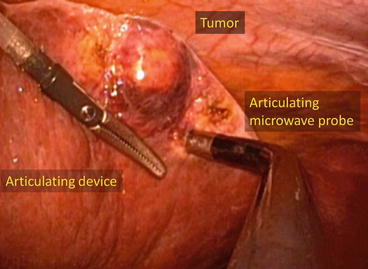
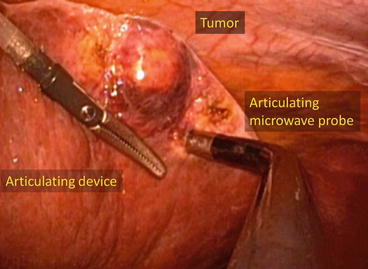
Fig. 21.4
Pre-coagulation performed with articulating microwave ablation instruments
hen a bulky part of the liver is transected, a more subtle technique is used. As in conventional laparoscopic hepatectomy, transection of the liver parenchyma in SPA hepatectomy can be done with an ultrasonic scalpel [17, 22] and the Cavitron Ultrasonic Surgical Aspirator (CUSA EXcel, ValleyLab, Inc., Boulder, CO, USA) [20] (Fig. 21.5). The superficial part of the liver can be cut with an ultrasonic scalpel (Fig. 21.3b), as there are no large vessels in this part. In contrast, in the deeper part of the liver, isolation of the vessels with the CUSA and meticulous hemostasis achieved with energy devices is necessary (Fig. 21.3c, d). We usually use a biclamp for hemostasis with a saline drip from an additional needle device inserted directly from the upper abdominal quadrant.


Fig. 21.5
Cavitron Ultrasonic Surgical Aspirator (CUSA Excel Plus, Integra Lifesciences). A handpiece for both laparoscopic and open laparotomy procedures is available
21.3.5 Hemostasis
Hemostasis is technically difficult in laparoscopic liver resection, making uncontrollable bleeding the main reason for conversion to laparotomy. In SPAS hepatectomy in particular, special attention must be paid to parenchymal transection. Thanks to recent innovations in the energy devices, laparoscopic transection of the liver parenchyma is now relatively safe. Low-voltage coagulation devices are useful for controlling bleeding during parenchymal transection [21]. The VIO electrosurgical unit (Erbe Elektromedizin GmbH, Tubingen, Germany) (Fig. 21.6a) can be operated in low-voltage “Soft Coag” mode, which allows rapid in-depth coagulation without carbonization and little sticking of the electrode. The VIO electrosurgical unit can be connected to the CUSA EXcel. The concurrent use of ultrasonic aspiration and low-voltage coagulation dramatically decreases bleeding upon parenchymal transection. The dripping of saline at the coagulation site enhances the hemostatic effect. We use a supplemental needle device inserted from the subcostal or intercostal region for the saline drip.
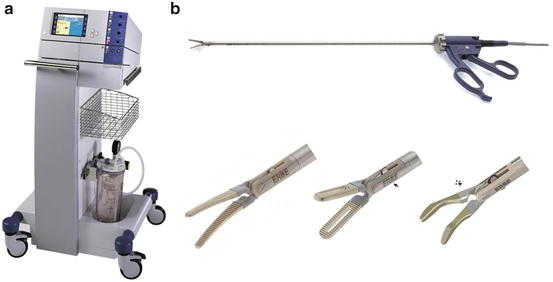
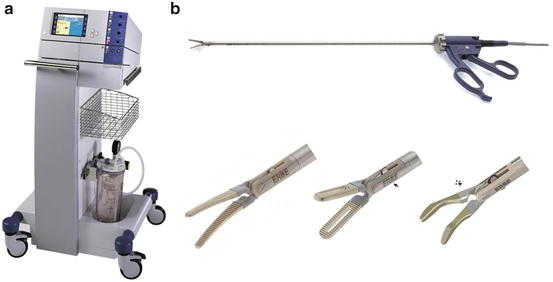
Fig. 21.6
The Electrosurgical system VIO300D generator (Erbe Elektromedizin GmbH, Tubingen, Germany) (a) and BiClamp LAP forceps, Maryland, deep-ribbed (Erbe Elektromedizin GmbH, Tubingen, Germany) (b)
The development of bipolar vessel-sealing devices has also contributed to safe parenchymal transection. The BiClamp forceps (Erbe Elektromedizin GmbH, Tubingen, Germany) (Fig. 21.6b) are bipolar and allow for firm grasping and reliable coagulation of vessels less than 3 mm in size. BiClamp is quite useful for stopping active bleeding and sealing the small vessels. LigaSure (Covidien, New Haven, CT, USA) (Fig. 21.7a) and EnSeal (Ethicon Endosurgery) (Fig. 21.7b) can seal and cut small vessels less than 3 mm in a sequential action, and no clipping is required. The number of instruments that can be used simultaneously in SPAS is limited, compelling the surgeon to change the instruments frequently. Thus, it is quite advantageous that the vessels can be sealed and cut in one action without clipping.




Fig. 21.7
(a) LigaSure (Covidien, New Haven, CT, US). (b) EnSeal (Ethicon Endosurgery, Cincinnati, OH, USA)
Vessels larger than 3 mm are clipped and transected. When the transection line is in the left lateral segment, the vascular pedicles are divided with the use of a laparoscopic stapler (Fig. 21.3e). An articulating laparoscopic stapler (Fig. 21.8a, b) is useful to achieve the ideal staple deployment angle.
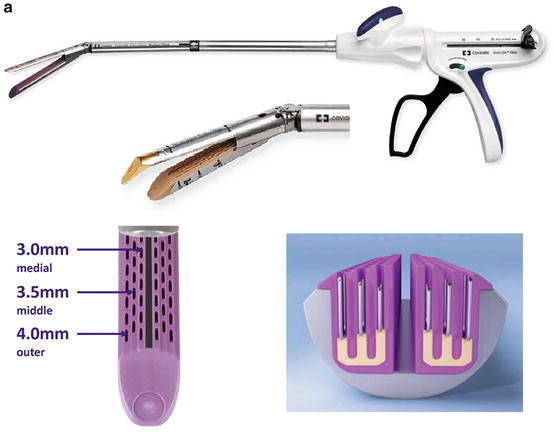

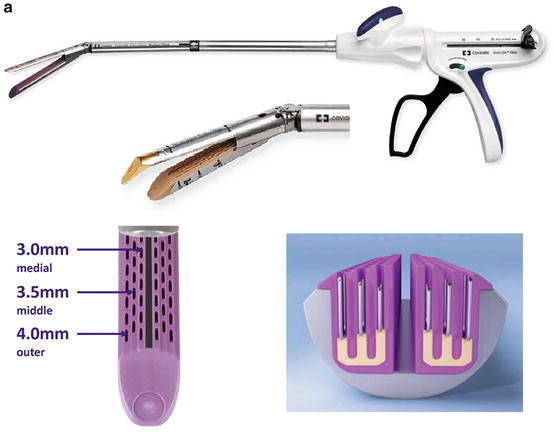

Fig. 21.8
(a) Endo GIA™ Ultra Universal staplers with Tri-Staple™ technology (Covidien, New Haven, CT, USA). (b) ECHELON FLEX (Ethicon Endosurgery, Cincinnati, OH, USA)
21.3.6 Completion of the Procedure
A plastic bag is introduced into the abdomen through the 12-mm trocar, and the specimen is extracted transumbilically (Fig. 21.3f). Because of the meticulous hemostasis, no suction drain is left in place. The umbilical fascia is closed with absorbable sutures.
21.4 Tips and Tricks
21.4.1 Crossed and Parallel Device Configuration
For the basic intra-abdominal procedure, a crossed device configuration (Fig. 21.9a)is useful because articulating devices allow non-parallel access to the surgical field and offer free movement of the manipulating devices. SPAS remains a demanding procedure; however, the cross-configuration makes it possible to triangulate even with 10-mm instruments such as the aspirator, stapling devices, and ultrasound probes. For the articulating device, we commonly use the SILS™ Clinch (Covidien, New Haven, CT, USA) (Fig. 21.10) or Autonomy™ Laparo-Angle™ grasper (Cambridge Endo, Framingham, MA, USA). These articulating graspers play an important role in exposing the operative field.