Hand Assisted
Peter W. Marcello
Restorative proctocolectomy is the procedure of choice for patients with ulcerative colitis requiring surgical intervention who wish a restorative procedure. The procedure is also indicated in patients with familial adenomatous polyposis with extensive rectal polyp formation. Unless otherwise contraindicated a laparoscopic approach is the preferred approach. Whether the procedure is performed by laparoscopy or by a hand-assisted approach is based upon the individual surgeon’s experience. In the author’s experience, hand-assisted approach has been associated with a reduction in operative time and conversions as compared to the laparoscopic technique, and therefore is the author’s preferred approach. There are rare contraindications as follow:
Extensive adhesion formation from prior surgery
Inability to tolerate pneumoperitoneum
There are no specific preoperative needs for a laparoscopic or a hand-assisted approach as compared to conventional open surgery. Appropriate preoperative antibiotics, heparin administration, and marking of a site for temporary fecal diversion should be planned.
Positioning
The patient is placed in a modified lithotomy position on a spilt-leg electric table.
The arms are at the sides surrounded by a beanbag.
Three-inch silk tape wrapped around the patient and beanbag to the table.
Technique
The operation begins with partial creation of the ileostomy (Fig. 29.1).
A core of skin and subcutaneous tissue is removed.
The anterior rectus sheath is incised vertically.
This maneuver is done to prevent the development of an obstruction of the loop ileostomy by the anterior rectus sheath following closure of the fascia in the Pfannenstiel incision. When a Pfannenstiel incision is created, the anterior rectus sheath is dissected from the rectus muscle and will be folded upward. If the ileostomy is made after the Pfannenstiel incision is created, it can act as a “shutter valve” when the fascia is closed, and may cause an obstruction at the ileostomy. This step is only done in cases where a temporary loop ileostomy is planned.
An 8-cm Pfannenstiel incision is made two fingerbreadths above the pubic symphysis.
The anterior rectus sheath is transversely incised and superior and inferior flaps are created over the rectus muscles.
The peritoneum is vertically opened between the rectus muscles.
The sleeve for the hand device is placed.
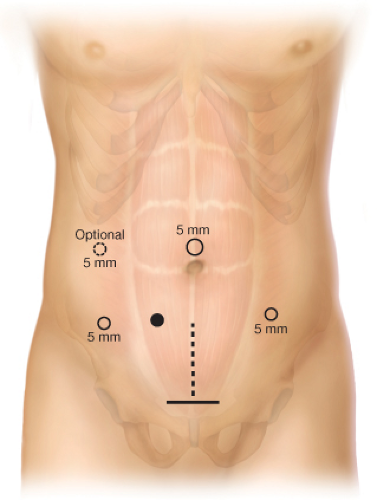
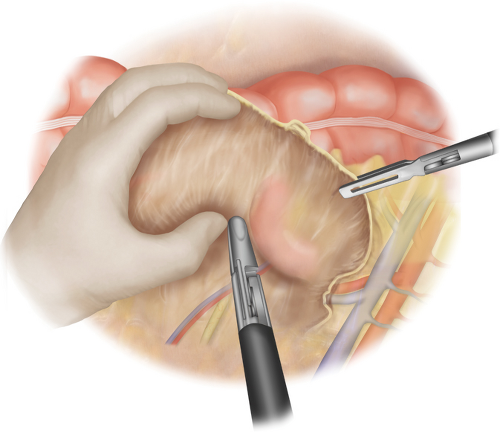
Five-millimeter trocars are positioned in the left lateral, supra umbilical, and right lateral positions. The right lateral trocar is placed lateral to and above the ileostomy site. Trocars are placed with the hand inside the abdomen to protect the intestine from injury (Fig. 29.1).
Right Colectomy—Medial Approach
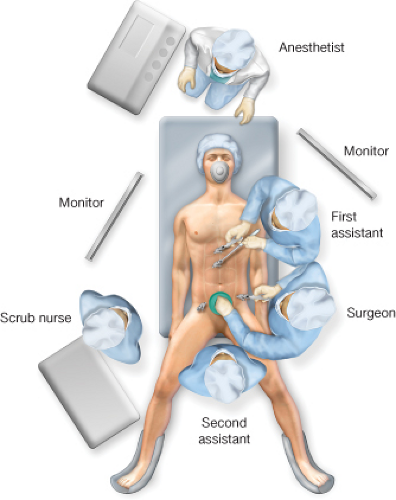
The surgeon stands at the patient’s left side with the left hand through the hand port and the right hand with a laparoscopic instrument (Fig. 29.2). The assistant stands cephalad to the surgeon, holding the camera. The patient is in slight Trendelenburg position with the right side up.
An exploration is undertaken. The colon is examined to determine the extent and the severity of disease. The small bowel is examined to exclude Crohn’s disease.
The cecum and the terminal ileum are elevated and laterally retracted with the hand.
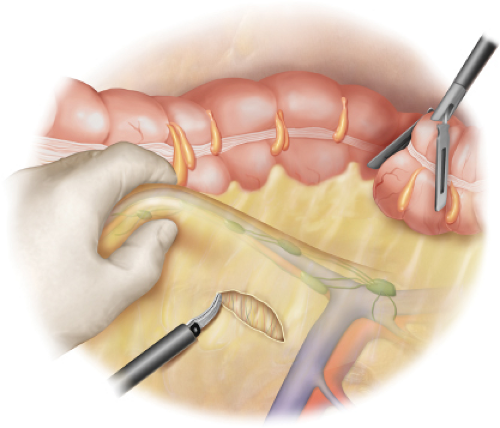
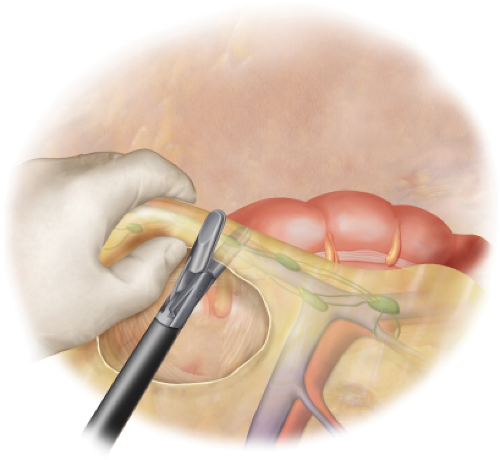
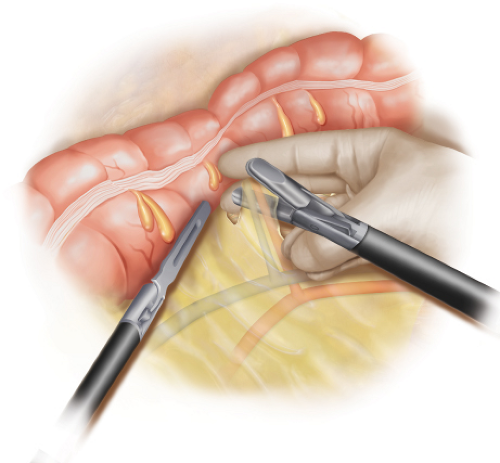
A medial to lateral dissection of the right and traverse mesocolon is performed. An incision is made under the ileocolic pedicle and the duodenum is swept downward (Fig. 29.3). The ileocolic pedicle is then isolated. The fingers are quite useful for isolating the pedicles. The ileocolic vessels are then divided and ligated using a bipolar vessel sealing device (Fig. 29.4). The 5-mm bipolar sealing device is the author’s preferred method of vessel ligation and division. Multiple applications of the device are used before the pedicle is divided. Although somewhat controversial, the ileocolic vessels are divided when performing a proctocolectomy and ileoanal pouch construction.
The right-sided colon is mobilized from medial to lateral (Fig. 29.5). The colon mesentery is freed from the retroperitoneum and duodenum. A hand is used to create traction while the scissors are used to perform the dissection.
If present, the right colic vessels are isolated and divided.
Transverse Colectomy—Medial Approach
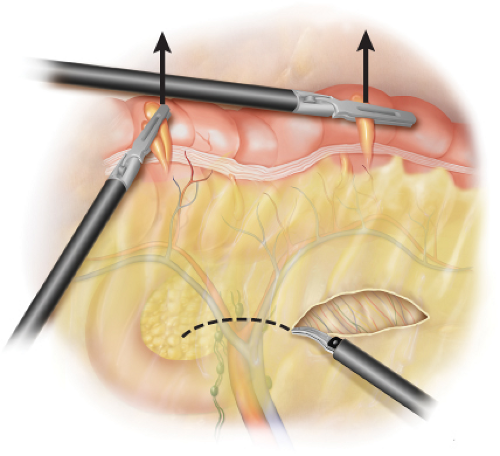
Attention is then shifted to the transverse mesocolon. The assistant moves from the patient’s left side to stand between the legs. The assistant’s left hand elevates the transverse mesocolon and a laparoscopic instrument is placed through the right lateral port. The assistant’s right hand controls the camera through the supra umbilical port. The surgeon remains on the patient’s left side with the left hand through the hand device and the right hand with a laparoscopic instrument. The assistant elevates the transverse mesocolon with a grasper in the left hand through the right-sided trocar, while the surgeon isolates each of the individual middle colic vessels. The dissection generally begins to the left of the midline in the transverse mesocolon (Fig. 29.6). This plane often has fewer adhesions into the lesser sac. The lesser sac is entered and the distal transverse mesocolon sharply divided.
Working back toward the patient’s right side, the main trunk middle colic vessel is isolated and divided (Figs. 29.7 and 29.8). The middle colic vessels may sometimes be ligated together or individually. Excessive tension on the vessels should be avoided when using a bipolar vessel-sealing device. The entire proximal and mid-transverse mesocolon is thus fully divided.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree